Day case TURP – is it feasible?
advertisement
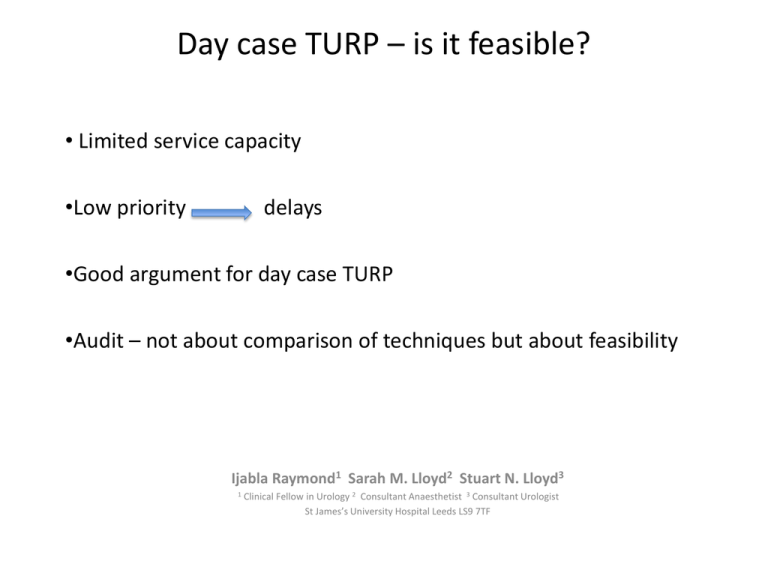
Day case TURP – is it feasible? • Limited service capacity •Low priority delays •Good argument for day case TURP •Audit – not about comparison of techniques but about feasibility Ijabla Raymond1 Sarah M. Lloyd2 Stuart N. Lloyd3 1 Clinical Fellow in Urology 2 Consultant Anaesthetist 3 Consultant Urologist St James’s University Hospital Leeds LS9 7TF Audit of 3 years inpatient TURPs in Leeds 2003-2005 ELECTIVE EMERGENCY Number of Average Total Average Pre- Average PostProcedures Stay days op Stay days op Stay days COMBINED Number of Average Total Average Pre- Average PostProcedures Stay days op Stay days op Stay days Number of Average Total Average Pre- Average PostProcedures Stay days op Stay days op Stay days Gyrus 230 4.97 1.48 3.5 126 9.39 5.35 4.04 356 6.54 2.85 3.69 Mono Polar 536 5.33 1.87 3.46 361 9.65 5.55 4.1 897 7.07 3.35 3.72 Totals 766 5.23 1.75 3.47 487 9.58 5.5 4.08 1253 6.92 3.21 3.71 No difference between techniques Inpatient culture affects duration of stay - TWOC Acutes - delay in theatre date, or medical reasons Justification for separate Day Case list Gyrus (Saline) TURP First performed in Leeds by SNL 1999 1st Day case procedure 2001 171 cases since then • Pre-assessment: catheter advice, DVT, aspirin/clopidogrel, DM medicines, Bloods, ECG • On day of surgery: consent, first on am list, GA/Spinal (avoid morphine), 3-way 18Fg foley with slow irrigation for approx 1-2hrs, no post op bloods needed • Aim home within 6hrs Recent decline due to increased need for DC ureteroscopy & TURBT loop TURP 130 loop TURP + bladder stone 7 PKVP vaporization 34 ASA % GA 157 1 15% Spinal 14 2 53% 3 32% 4 <1% Intent for early discharge (147 /171) 83 discharged same day usually after 2 hours irrigation within 6 hour surgery 49% discharged same day 49 discharged early next day - intent 23 hour stay 8 discharged after 48 hours - catheter free (some prolonged bleeding) 77% discharged within 23hrs 5 discharged after 3 days catheter free 2 discharged by 5 days catheter free Ideal plan - home with a catheter and early removal TWOC day 160/171 day 0 4 day 1 27 day 2 122 day 3 5 (bleeding) day 5 2 (bleeding) 90% had successful TWOC within 2 days All patients delighted with outcome although as expected some took time for urinary symptoms to settle 1 admission due to administration of morphine 1 re-admitted having failed a home TWOC 7 delayed discharge longer than 23 hours due to bleeding 7 readmissions with secondary bleeding (also 1 patient bled for 1 month but was not admitted) 4 re-admissions with infection, GP treated 2 at home 1 haematemesis 3 days post-op – admitted 3 re-operation TURP (2 cancer underwent channel TURP , 1 BPH patient at 3 yrs after PKVP) 4 later diagnosed with cancer, 2 underwent radical prostatectomy BPH 127 histology assumed BPH 37 vaporized Cancer 2 known; 5 new + 4 later diagnosis Reasons to do day case TURP • Reduced pressure on beds • Increasing pool of patients (e.g. 33% - ASA 3; AUR) • Reduced risk of hospital acquired infection and complications • Patient choice • Cheaper – electrodes cost £100 more; but savings on fluid + reduced hospital stay • Day case tariff incentive £300 (day case fee £1863; inpatient fee £1563) £51,300 bonus plus reduced cost of 6-7 days inpatient stay Suggested sequence of pathways • Initially do a day-case through an inpatient ward • Plan 23 hour stay for all • True day-case with early discharge with recourse to inpatient bed or 23 hour bed • Plan day-case for suitable elective cases (4-6hr stay) • Consider a urinary retention pathway - hospital discharge and readmit as a day-case • Direct booking from other units or primary care assessment