PCV - University of Louisville Department of Ophthalmology and
advertisement

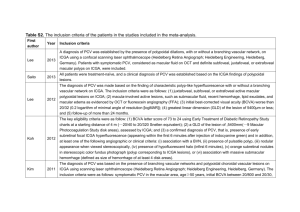
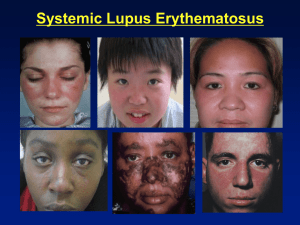
Grand Rounds Shivani V. Reddy, M.D. 7/18/14 University of Louisville Department of Ophthalmology and Visual Sciences Patient Presentation CC: Blurry Vision OD HPI: 80 y/o AAF presents for yearly Plaquenil check She states that her vision had been stable until 1 month ago when she noticed some blurriness and dimming of vision OD. She denies experiencing metamorphopsia, flashes, floaters or scotomas. History POHx: refractive error PMHx: Rheumatoid Arthritis, Hypertension, Hypothyroidism FAMHx: uknown ROS: joint pain MEDS: Plaquenil ( 3.04 mg/kg/day (65.7kg weight), 200mg daily x 5 years) Toprol, MTV, triamterone, synthroid ALLERGIES: NKDA Exam 8 20/50-2 (+0.75 +0.50 x 005) VA TP 20/20-2 (-0.25 +0.50 x 175) 4→3 P 12 4→3 no RAPD EOM: full OU CVF: full OU Exam OD OS LIDS/LASHES WNL WNL CONJ WNL WNL CORNEA WNL WNL IRIS WNL WNL LENS 2+NS, 1+CC 2+NS, 1+CC Fundus Photos OD OS OD photo demonstrates orangish-red faintly circumscribed lesions in the peripapillary region FAF Photos OD OS 1.OD 2.OD 3.OS 1. Nasal pigment epithelial detachment with associated neurosensory detachement with sub-neurosensory fluid accumulation, some loss of foveal contour 2. Nasal pigment epithelial detachment with overlying heme and fluid FA/ICG Early AV Phase 00:19:45 Peripapillary staining, supero-nasal hypofluorescence of dye Superonasal hypofluorescence, network of dilated peripapillary vasculature with terminal bulb FA/ICG AV Phase 00:29:45 Increasing peripapillary hyperfluorescence circular of hyperfluorescence at end of vascular network FA/ICG Recirculation Phase 1:21:45 continual demonstration of peripapillary dye leakage, increasing over area of polyp Hyperfluorescence of polypoid lesion and demonstration of surrounding vascular network FA/ICG Late Phase 2:00:45 Persistent peripapillary dye pooling representing leakage Decreased hyperfluorescence of polyp with surrounding area of hypofluorescence Summary 80 y/o AAF presents for routine plaquenil check with 1 month history of blurriness and dimming of vision OD. BCVA OD is 20/50-2. ICG angiography demonstrates choroidal polyps with surrounding vascular network and corresponding leakage on FA. OCT demonstrates PED’s OD with overlying neurosensory retinal detachment DDx: Polypoidal Choroidal Vasculopathy Other entities causing subretinal neovascularization AMD CSCR (central serous chorioretinopathy) Pathologic myopia Choroidal tumors or Mets Infection Treatment First Visit 20/50-2 1 month post Avastin #1 VA 20/50 1 month post Avastin #2 VA 20/40-2 Polypoidal Choroidal Vasculopathy Also known as posterior uveal bleeding syndrome First described by Dr.Yannuzzi in 1982 Characterized by sub-retinal vascular lesions associated with serous and hemorrhagic detachments of the RPE Named for its network of branching, choroidal vessels with terminal polyp-like aneurysmal dilations Polypoidal Choroidal Vasculopathy First described in middle -aged African American woman Most commonly seen in 50-65 age group Occurs 23-55% in Asian patients presenting with neovascular AMD 4% to 9.8% prevalence reports in Caucasian patients with presumed AMD Polypoidal Choroidal Vasculopathy Diagnosis based on ICG angiography high definition OCT and fundus photography FA not helpful as it demonstrates too much dye leakage Classification based on imaging characteristics Branching vascular network vs. feeder vessel supplying polyps Cluster of polyps vs. single polyp Juxtafoveal vs. extrafoveal polyps Polypoidal Choroidal Vasculopathy CNV or Not? PCV is? More likely to occur in pigmented races, although also demonstrated in Caucasians lesions more likely to be peripapillary ICG in late phases shows ‘wash-out’ of polyp in contrast to late staining seen in occult CNV Polypoidal Choroidal Vasculopathy Treatment Anti- VEGF treatment alone not helpful EVEREST TRIAL Compared PDT monotherapy and PDT + ranibizumab to ranibizumab alone Significantly higher proportion in the first 2 groups showed regression at 6 months Surgical intervention based on complications such as breakthrough vitreous hemorrhage Polypoidal Choroidal Vasculopathy Prognosis Clinical outcomes in literature vary considerably 35-68.2% of patient with reported poor outcomes Larger polyps, juxtafoveal location of polyps and clustering of polyps are risk factors for massive subretinal and subsequent vitreous hemorrhages In patients with large detachments, subretinal fibrosis can lead to eventual vision loss PDT can lead to subretinal hemorrhage in upto 31% of eyes, VH in 6-12.5% post treament, 8.9% of bleeding post anti-VEGF Retrospective chart review 17 patients with massive subretinal hemorrhages (SRH) secondary to PCV (16.7+/- 7.1 DD) and associated vitreous hemorrhage (VH) enrolled Patients underwent 20G Pars Plana Vitrectomy +/bevacizumab injection for new heme, PED or CME Main outcome measure: BCVA at end of follow-up period Mean post-op follow up of 25.2 months Mean duration from SRH to VH was 3.5 +/- 1.2 weeks Time from VH to PPV 1.3 +/- 0.7 months BVCA (LogMar) Pre VH : 0.95 +/- 0.60 Pre PPV: 2.65 +/- 0.57 3 months post-op: 1.62 +/- 0.67 Final Visit: 1.43 +/- 0.82 VA > 20/400 in 16.7% of juxtafoveal polyp patients, 87.5% of extraoveal polyp patients THANK YOU References 1.Retina and Vitreous, BSCS 2. Retina, Vitreous and Macula , David R. Guyer MD, Lawrence A. Yannuzzi MD, Stanley Chang MD and Jerry A. Shields MD 3.Yannuzzi LA, Sorenson J, Spaide RF, Lipson B. Idiopathic polypoidal choroidal vasculopathy (IPCV). Retina 1990; 10(1): 1–8. 4.Koh et al. EVEREST STUDY: Efficacy and Safety of Verteporfin Photodynamic Therapy in combination with Ranibizumab or Alone Versus Ranibizumab Monotherapy in Patients with Symptomatic Macular Polypoidal Choroidal Vasculopathy. Retina 2012; 32:1453-1464. 5. Uyama M, Wada M, Nagai Y, et al. Polypoidal choroidal vasculopathy: Natural history. Am J Ophthalmol. 2002; 133(5):639-48. 6. Lim TH, Laude A, Tan CS. Polypoidal choroidal vasculopathy: An Angiographic discussion. Eye (Lond) 2010; 24:483–490 7.Kamaeda T, Tsujikawa A, Otani A, et al. Polypoidal choroidal vasculopathy examined with en face optical coherence tomography. Clin Experiment Ophthalmol. 2007; 35(7):596-601. 8.Sato T, Kishi S, Watanabe G, et al. Tomographic features of branching vascular networks in polypoidal choroidal vasculopathy. Retina. 2007 27; 589-594. 9.Park DH, Shin JP, Kim IT. Association of plasma malondialdehyde with ARMS2 genetic variants and phenotypes in polypoidal choroidal vasculopathy and age-related macular degeneration. Retina 2013; 0:1–10.