Back Pain & Treatment modalities
advertisement

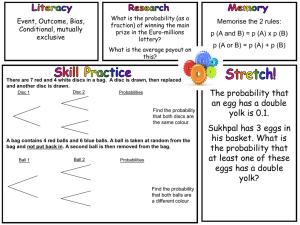
Back Pain & Treatment Modalities Dr. Dawood Nasir Director Acute Pain & Regional Anesthesia UTSouthwestern Medical Center Overview • Back pain affects most people at least once over their lifetime. • It can be a cause for lost wages & productivity • Most people will become better in 6 weeks Anatomy • The back is composed of vertebrae, muscles, ligaments, intervertebral disc,& nerves. • There are 7 cervical, 12 thoracic, 5 lumbar & 5 coccygeal vertebrae • Spinal cord has cervical lordosis, Thoracic kyphosis, & lumbar lordosis Assessment of Low Back Pain • History & Physical: Nocturnal exacerbation occurs w tumors or inf, w benign causes like herniated disc pain improves w bed rest • Limitation of spinal motion correlates with the presence of lower back disability • Palpation: Gentle & systemic palpation of the back, coccyx, sacrum, levator ani, coccygeus, & piriformis ms, & associated ligament done • Muscle spasm: has localized tenderness, & increase in ms tone Assessment of Back Pain • Pain on percussion occurs with metastases or inf, does not occur w disc protrusion & spasm • Radiological test: Plain Xrays show degenrative disc ds, spondylitis, compression fx, metabolic bone disorder, bone tumors, congenital anomalies & transitional vertebrae • Oblique view of lumbosacral level is used to visualize facet & sacroiliac joint • Flexion-extension view is added when ever spinal instability suspected Straight leg raising test • Straight leg raising test should be performed to detect nerve root irritation • Even with a soft tissue pain source, SLR can be used as an index of improvement • A +ve crossed SLR test has the highest correlation w myelographic finding of a herniated disc Causes of back pain • Pain sensitive structures are the supporting bone, articulations, meninges, nerves, muscles, & aponeuroses • Vertebral body despite being short is actually a long bone with end plates of hard bone & a center of cancellous bone • It is innervated by dorsal roots • Periosteum is pain sensitive as is facet joint which have a capsule & meniscus richly innervated w nociceptors Muscular Pain • Most back pains are caused by sprain or strain of the back muscles & ligaments • Pain will be in discrete area & tender to touch • It is of aching quality & may involve muscle spasm • Pain not involved shooting pain Spinal causes • • • • • • • Osteoporosis Osteomylitis Herniated Disc Spondylolisthesis Spondylolysis Facet hypertrophy Ischemia of the spinal cord Osteoporosis • Osteoporosis is painful due to microfracture • Absence of wt bearing due to bed ridden leads to demineralization & fx upon wt bearing • Postmenopause & pt Rx with corticosteroid is at risk • Other cond r/o w serum protein electrophoresis, sed rate, alkaline phosphatase, ca, x-rays.Rx Biphosphonate, raloxifene Osteomyelitis • Vertebral osteomyelitis presents as subacute back pain that increases over days to weeks • Pain in low back if unRx focal weakness, bowel & bladder problem results • Most common in lumbar spine in men over 50 • With AIDS younger men & cervical spine affected Osteomyelitis • In immunocompetent hosts, Staphylococcus aureus inf most common • Inf involves vertebral bodies, endplates, & disc spaces, spares post elements • In rare cases actinomycosis or coccidiodomycosis, posterior elements involved & spine becomes unstable Vertebral metastases • Vertebral metastasis presents as localized, deep, aching, back pain • If nerves are involved, pain occurs in neural distribution • Thoracic spine is most commonly affected • Epidural spinal cord compression is a medical emergency & pt may present with paraparesis, sensory loss, bowl & bladder involvement Vertebral metastases • On plain film earliest sign of spinal metastasis is erosion of pedicle • Over time vertebral body begins to lose height • MRI reveals change in signal intensity in vertebral body • As tumor progresses, it may be seen invading epidural space & compressing spinal cord Facet joint pain • The vertebral bodies have 4 facet joint, 1 pair above & 1pair below • Synovial joints mean they have fluid with in them • Back pain caused by arthritis of the facet joints is mostly midline & may spread to the back & to the flanks • Gets worse with bending backward & side to side Herniated Disc • Intervertebral disc consists of an outer fibrous body called the annulus fibrosus & an inner gel like substance called the nucleus pulposus • It acts as a shock absorber & spacer for the spine giving room for the intervertebral neural foramina which are portals for the exit of the spinal nerves • The nucleus pulposus contains noxious chemicals which can be irritating to nerves Herniated disc-cont• The intervertebral discs lie between the vertebral bodies. In front is the ant. longitudinal ligament & behind the post. longitudinal ligament & behind that is spinal cord. • Wear & tear can cause annulus fibrosus to weaken allowing bulges of nucleous pulposis • These bulges may protrude out enough to touch the spinal cord causing irritation to nerves • These large disc bulges are called herniation Herniated Disc • With extreme forces these disc bulges may tear the annulus fibrosus & allow leakage of nucleus pulposus • This is observed as sudden sharp pain radiating down the leg • The chemicals of nucleus pulposus can cause swelling of nerves resulting in constant burning pain termed lumbar radiculopathy or sciatica, pain radiating down the leg & feet Types of Herniate Disc • • • • Disc degeneration Disc prolapse Disc extrusion Disc seqestration Radiographic herniated disc Spondylosis • It can be described as arthritis of the spine • The bony surfaces may become roughened & bony spurs may develop & intrude upon the spinal canal Spondylolisthesis • It is a slippage of the vertebra upon one another • The vertebra are usually aligned so that each one is stacked like “legos” so that the spinal canal is a fairly straight tube Spondylolithesis • If there is a slippage, the spinal canal has a kink & is a smaller in that area • When spinal stenosis occurs, it squeezes upon the spinal cord • This may cause irritation or ischemia of the spinal cord & lead to cramping or aching of the legs Grades of Spondylolisthesis Piriformis Syndrome • It is a syndrome of low back & leg pain due to ch. Contracture of the piriformis muscle that causes irritation of sciatic n • Gluteal pain radiates to sciatic nerve • It occurs by compression of nerve between ms. Or ms & pelvis Buttock pain • • • • Common causes are Piriformis syndrome Ischial tuberosity inj. Rupture of gluteal ms. Piriformis Syndrome • It is also called “hip pocket neuropathy” or “wallet neuritis” • Piriformis ms is flat, pyramidal ms that originates from ant surface of sacrum from S2-S4 & sacrotuberous lig passes through the upper part of greater sciatic notch, & inserts on superior surface of great trochanter Treatment of Back Pain • • • • Walking is best exercise Physical therapy for core stabilization Spinal manipulation & manual therapy Analgesics like acetaminophen, NSAID’S, antidepressants • Application of heat or ice • Acupuncture • Corticosteroid injections Treatment of Chronic Back Pain • Treat the cause like in osteomylitis, surgery with antibiotics is used • Vertebral metastasis will respond to high doses of dexamethasone, definitive treatment with radiation & surgery • Osteoporosis treated with Biphosphonate, Robaxifene • Muscle spasms may respond to ms relaxants Back Exercises • • • • • • • • • Ankle pump Heel slides Abdominal contraction Wall squats Heel raises Straight leg raises Knee to chest stretch Hamstring stretch Exercises with swiss ball Epidural steroid injection • Epidural space identified w loss of resistance tech or fluroscopy • 60-80 mg of triamcilone with 0.25% bupivacaine injected Intradiscal electrothermic therapy • IDET is done using fluoroscopy, a hollow needle containing flexible tube & heating element is inserted into spinal disc • The catheter placed in a circle in the annular layer of disc & slowly heated to 194 deg. • The heat is meant to destroy the nerve fibers & toughen the disc tissue, sealing any small tear Vertebroplasty • Under fluoroscopy, a hollow needle is inserted & a cement is injected to restore the vertebra Kyphoplasty • In kyphoplasty a ballon is inserted through the hollow needle into the fractured bone to restore the height & shape of the vertebra. • Once the ballon is removed, the cement mixture is injected. Kyphoplasty / Vertebroplasty Spondylolithesis Discectomy • A scope is inserted through a small cannula to inspect disc surface • Peri-annular fat is removed & small capillaries are cauterized • Small nerves in the annular fat can be removed with periannular tissue WHO Pain ladder GOAL: Freedom From Pain STEP 3 Pain Persists STEP 2 Pain Persists STEP 1 • Step 3: Opioids for moderate-to-severe pain +/- non-opioid +/adjuvant therapy • Step 2: Opioids for mild- to-moderate pain +/- non-opioid +/adjuvant therapy • Step 1: Non-opioid +/- adjuvant therapy WHO Pain Ladder • Step 1 Mild (pain rating 1-3) Non opioid + co-analgesics e.g. NSAID+TCA/membrane stabilizer/ms.relax. • Step 2 Moderate (pain rating 4-6) Opioid + Non opioid + co-analgesics Lorcet + NSAID+TCA/memb. Stab./ms. Relax. • Step 3 Severe ( pain rating 7-10) Pure opioids + non-opioids + co-analgesics e.g. Morphine SR + NSAID + above. Opioid combination products Drug Opioid Non-opioid Doses Lortab (vicodin) Hydrocodone 5 mg APAP 500 mg 1-2 q 4 hrs. Max. 8 tabs/day Lorcet Hydrocodone 10 mg APAP 650 mg 1 q 4 hrs. Max. 6 tabs/day Tylenol # 3 Codeine 30 mg APAP 300 mg 1-2 q 4 hrs. Max. 13 tabs/day Norco Hydrocodone 10 mg APAP 325 mg 1-2 q 4 hrs. Max. 12 tabs/day Percocet Oxycodone 5 mg APAP 325 mg 1-2 q 4 hrs. Max. 12 tabs/day Tylox 5/500 Oxycodone 5 mg APAP 500 mg 1-2 q 4-6 hrs. Max. 8 tabs/day Acetaminophen (Tylenol) • MoA: Cox-3 inhibter of PG in the CNS & peripheral pain impulse • Pain indication: Use alone for mild pain • Do not exceed 4 gms / day • Lorcet – 6 tabs/day= 60 mgs morphine • Lortab- 8 tabs / day=40 mgs morphine • Adverse effects: -Lightheadedness, dizziness, hepatotoxicity with high doses & chronic use NSAID’S • Indications: anti-inflammatory, antipyretic, analgesic • Acetylsalicylic acid ( ASA ) irreversibly inhibits platelet • Side effects: Reversible antiplatelet effect, minimal w/ non-acetylated salicylates ( eg Disalcid, Dolobid ) - GI ulceration, less w ibuprofen, etodolac, salsalate, nabumentone - Nephrotoxity – caution in CHF, dehydratation, elderly - Hepatotoxicity: caution in elderly & alcoholics - Avoid in asthmatics & nasal polyps Mechanism of Action – Phospholipids, released from cell membrane are cenverted to Arachidonic acid by phospholipase A2 – Arachidonic acid is acted by lipo-oxygenase to be converted to Leukotrienes – Cyclo-oxygenase acts on Arachidonic acid to form Prostaglandin endoperoxides which are converted to Prostaglandin G & by isomerase into Prostaglandin E2, Prostaglandin D2, & F2 alpha – Prostaglandin H is formed from prostaglandin endoperoxides & converted by Thromboxane to Thromboxane A2 & Thromboxane B2. – Prostacyclin synthetase converts prostaglandin endoperoxides to Prostacyclin ( PGI ) Co-analgesic Pain Medications • • • • • • • Antiepileptics Antidepressants Muscle Relaxants Anesthetics Corticosteroids Psychostimulants Substance P inhibitors • • • • Alpha-2 agonists Neuroleptics Antiarryhmics Benzodiazepines Antiepileptics • MOA: Block Na+ & Ca+ channels>>inhibits release of glutamate>> stabilizes neural memb. • Uses: Trigeminal neuralgia, peripheral neuropathies, herpetic neuralgia, phantom limb pain, migraines. • Aniepileptics: Gabapentin, Carbamazepines, topiramate, phenytoin, oxycarbamazepine, pregabalin • Comared to TCA’s: -equally efficacious in painful DN -some AED may be more expensive - differences in safty profile - synergy with AED plus TCA Gabapentin (Neurontin) • MOA: a 2-delta ca+ channel subunit modulator • Uses: Peripheral neuropathic pain, phantom limb pain, CRPS, post herptic & trigeminal neuralgia. • Doses: adjust for elderly & renal failure -range 300- 3600 mg /day divided in 3-4 doses • Somnolance, dizziness, constipation, fatigue, peripheral edema, difficulty concentrating Pregabalin (Lyrica) • MoA: a 2 delta Ca+ channel subunit modulator • Pain uses: Diabetic & post herpetic neuropathic pain at doses 300-600 mgs/day divided 2-3 X. • Other neuropathic pain conditions, fibromyalgia, generalized anxiety disorder. • Compared to gabapentin: - Bioavailability remains 90% at all doses - Time to effective dose (150-300mg/day) is 1-3days - Class v schedules drug. Carbamazepine ( Tegretol) • MoA: Na+ & Ca+ channel blockade • Pain uses: trigeminal neuralgia, glossopharyngeal neuralgia, DPN • Dosing: 200-1000mg divided 2-3X (with food) • Side effects: N & V, dizziness, sedation, transient leukopenia, hepatic toxicity, thrombocytopenia, diplopia, hyponatremia, rash, Steven-Johnsons syndrome. Tricyclic antidepressants • MoA: inhibits re-uptake of NE, SE, antihistamine • Pain indications: Painful neuropathies, Phantom limb pain, migraine prevention • Dose: start low & adjust every 2- 3 days • Drug interactions - caution with other anticholinergics/serotonergics - CYP2D6 substrate ( all TCA’s) - CYP3A4 substrate ( Elavil ) Choice of A TCA • Amitriptyline ( Elavil) - most widely studied - more side effects- hang over effect. • Doxepin ( Sinequan ) - similar to Elavil, but shorter duration of sedation • Desipramine ( Norpramin ), Nortriptyline ( Pamelor) - may cause insomnia - less anticholinergic effect - Desipramine may cause orthostatic hypotension TCA – Side Effects Side effects • Blurred vision • Cognitine changes • Constipation • Dry mouth • Orthostatic hypotention • Sexual dysfunction • Tachcardia • Urinary retention • Desipramine • Nortriptyline • Doxapin • Amitriptyline Duloxetine ( Cymbalta ) • • • • MoA : Dual reuptake inhibitor ( NE & SE ) Indications : Neuropathic pain, depression Dosage : 30 mgs PO qd to 60 mgs PO bid Side effects : nausea, dry mouth, constipation decreased appetite, dizziness, insomnia • Drug interaction : CYPIA2 & 2D6 substrate – SSRI’s , quinidine, cimetidine, quinolenes, may increase duloxitine levels. - mod. Inhibitor of CYP2D6 – increases TCA’s, phenothiazine, type 1C antiarrythmias Muscle Relaxants • Heterogenous group of medications: - Spasticity from upper motor neuron syndrome - Muscular pain & / or spasm from peripheral musculoskeletal condition. - Dose : may dose 6-8 hrs ATC or give more hs if daytime drowsiness does not resolve ( e.g. Flexaril 10-30 mg po qhs ) Side effects:Drowsiness,dizziness,blurred vision Drug interaction: Other CNS depressants Muscle Relaxants • - Spasticity: Baclofen ( Lioresal ) Tizanidine ( Zanaflex) Dantrolene ( Dantrium ) Diazepam ( Valium ) • Muscular pain & spasm - Methcarbamol (Robaxin) - Cylobenzaprine(Flexaril) - Carisoprodal ( Soma ) - Baclofen ( Lioresal ) - Tizanidine ( Zanaflex ) Muscle Relaxants • - Spasticity: Baclofen ( Lioresal ) Tizanidine ( Zanaflex) Dantrolene ( Dantrium ) Diazepam ( Valium ) • Muscular pain & spasm - Methcarbamol (Robaxin) - Cylobenzaprine(Flexaril) - Carisoprodal ( Soma ) - Baclofen ( Lioresal ) - Tizanidine ( Zanaflex ) Baclofen ( Lioresal ) • • • • Baclofen ( Lioresal ) – gaba – b agonist Indications : Neuropathic pain, spasticity Side effects : less sedating, ms weakness With drawl syndrome: spasticity, hallucination, anxiety,seizure when doses 80 mgs/ day or intrathecal baclofen are stopped abruptly Flexeril ( Cyclobenzaprine ) • Indications : muscle spasms, neuropathic pain • Side effects : CNS & anticholinergic effect • Drug interactions : w/TCA’s additive anticholinergic side effects, CYPIA2 substrate Systemic / Topical anesth. • Lidocaine 5% patch apply to intact skin at most painful site, 1- 3 patches for 12 hrs • Indications : Post-herpetic neuralgia, post thoracotomy, mastectomy, pain syndrome. • Side effects : site irritation, dizziness, arrythmia’s • Lidocaine cream 5% apply to affected area 3-4 X / day for short term use. • Mexileteine 150 mg po bid adjust q 2-3 days upto 400 mgs / day - Indications : resistant neuropathic pain - Side effects : dizziness, tremor, GI upset, arrythmia’s Tramadol ( Ultram ) • MoA : mu – opioid receptors, NE & SE reuptake inhibitors • Mixed mild to moderate pain • Side effects: dizziness, nausea, constipation, somnolence, sweating, pruritus, sz, serotonergic syndrome • Maximum dose: 400 mg / day • 10-20% pt. lack CYP2D6 needed to form MI ( metabolite ) impact or efficacy & safety • Dose conversion: 50 mg = codeine 30 mg. Botulinum Toxin A ( Botox ) • MoA : direct antinociceptive effects, prolonged ms relaxation by inhibition of acetylcholine release at the neuromuscular junction • Indications : Blephrospasm, facial wrinkles, ms spasm • Duration of effect : 3 – 4 months • Side effects: Opioids • MoA : agonist on mu, kappa, & delta receptors • Methadone: also NMDA receptor antagonist & NE/SE reuptake inhibitor • Indications: Acute & ch Moderate to severe pain • For most type of pain with limited use in - Neuropathic pain - Spinal cord compression - Bone pain