Neuropathic Pain
advertisement

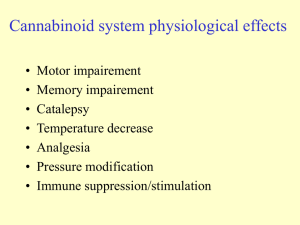
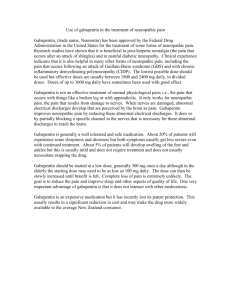
Neuropathic Pain in Advanced Illness Russell K. Portenoy, MD Chairman and Gerald J. and Dorothy R. Friedman Chair in Pain Medicine and Palliative Care Department of Pain Medicine and Palliative Care Beth Israel Medical Center Chief Medical Officer Continuum Hospice Care Professor of Neurology and Anesthesiology Albert Einstein College of Medicine Neuropathic Pain: Definitions • Pain believed to be sustained by aberrant • somatosensory processing in the peripheral or central nervous systems Pain related to damage or dysfunction of the nervous system Neuropathic Pain: Clinical Challenges • Multiple classifications – By medical diagnosis – By localization of neural injury – By inferred pathophysiology • Diverse phenomenologies within a diagnosis Neuropathic Pain: Clinical Challenges • Classification by medical diagnosis – Examples Chemotherapy-induced polyneuropathy Malignant plexopathy Post-stroke central pain syndrome Complex regional pain syndrome Neuropathic Pain: Clinical Challenges • Classification by neurological localization – – – – – Polyneuropathy Mononeuropathy (ies) Radiculopathy Myelopathy Encephalopathy Neuropathic Pain: Clinical Challenges • Classification by inferred pathophysiology – Based on inference about sets of mechanisms that may be sustaining the pain – Determined usually by phenomenology of the pain and the clinical examination – Best viewed as a construct that can guide treatment – In the future, should be replaced by “mechanismbased treatment” Neuropathic Pain: Clinical Challenges • Classification by inferred pathophysiology – Distinguishes pain with “peripheral generators” and pain with “central generators” Neuropathic Pain: Inferred Pathophysiologies Peripheral generator Mononeuropathy Neuroma Nerve sheath pain Central generator Polyneuropathy Deafferentation syndromes Axonopathy myelinopathy Sympatheticallymaintained pain Anesthesia dolorosa/ phantom pain Central pain Neuropathic Pain: Diverse Phenomenologies • Some patients report dysesthesia (“abnormal discomfort or pain”) – – – Burning, shooting, electrical Aftersensations Spontaneous or touch-evoked • But some patients report familiar pain (e.g. aching) Neuropathic Pain: Diverse Phenomenologies • Some patients report neurological phenomena – – – – Paresthesia (abnormal nonpainful sensations) Weakness, clumsiness Loss of sensation Focal autonomic dysregulation (swelling, skin changes, sweating abnormalities) • But some patients have pain alone Neuropathic Pain: Diverse Phenomenologies • Some patients have neurological signs – Allodynia, hyperalgesia – Hyperpathia – Other sensory abnormalities – Weakness, incoordination, reflex asymmetries – Focal autonomic or trophic changes • But some patients have normal exams Neuropathic Pain: Clinical Challenges • • • Multiple phenomenologies and disorders suggest overlapping sets of mechanisms For now….most treatment is based on limited data, intuition, trial-and-error, and best clinical judgment, guided by diagnosis, neurological localization and inferred mechanisms Goal in the future… “mechanism-based therapy” Neuropathic Pain: Mechanisms • Peripheral processes – Transduction dysfunction – Peripheral sensitization – Membrane excitability at primary afferents • Central process – Synaptic transmission dysfunction – Central sensitization – Reduced inhibition Therapeutic Strategy for Neuropathic Pain • Treat underlying cause, if possible and • appropriate Pharmacotherapy is the mainstay – First-line is still an opioid – Consider other systemic and topical analgesics • Many options, most extrapolated from noncancer pain • Relatively few RCTs and very few comparative trials • Other approaches is selected cases Dworkin RH, et al, Arch Neurol. 2003;60:1524-1534. Finnerup NB, Otto M, McQuay HJ, Jensen TS, Sindrup SH. Pain. 2005;118(3):289-305. Pharmacotherapy of Neuropathic Pain • Opioids • “Adjuvant analgesics” • NSAIDs Opioids in Neuropathic Pain • NOT correct: “Neuropathic pain is ‘resistant’ • to opioids” Limited data suggest – Neuropathic pain is less responsive than nociceptive pain – Poorly responsive syndromes are more likely to be neuropathic • But opioids are clearly efficacious Opioids in Neuropathic Pain • Positive trials of oxycodone in DPN and PHN • Positive trial of methadone in mixed types of neuropathic pain • Positive trial of morphine in PHN • Positive trial of levorphanol in peripheral and central neuropathic pain Gimbel JS et al: Neurology. 2003;60:927-934. Watson CP, Babul N: Neurology. 1998;50:1837-1841. Morley JS et al: Palliat Med. 2003;7:576-587. Raja SN et al: Neurology. 2002;59:1015-1021. Rowbotham MC, et al: NEJM. 2003;348:1223-1232. Opioids in Neuropathic Pain • Positive systematic review of tramadol (5 trials) • Positive trial of morphine + gabapentin, and morphine alone, relative to gabapentin in patients with DPN or PHN Duhmke RM, et al. Cochrane Database Syst Rev. 2004:CD003726. Gilron I, et al: NEJM. 2005;352:1324-1334. Opioids in Neuropathic Pain: Conventional Practice • Opioids remain first-line for most patients with • moderate to severe neuropathic pain related to serious medical illness In most cases, the opioid regimen should optimized before addition of other drugs Pharmacotherapy of Neuropathic Pain • Opioids • “Adjuvant analgesics” • NSAIDs Adjuvant Analgesics • Traditional definition Drugs with indications other than pain which may be analgesic in specific circumstances • Numerous drugs in diverse classes, • some now specifically indicated for pain Use in neuropathic pain in the medically ill extrapolated from observations in other populations Adjuvant Analgesics • • • • • Multipurpose analgesics Drugs used for neuropathic pain Drugs used for bone pain Drugs used for bowel obstruction Drugs used for muscle spasm Multipurpose Adjuvant Analgesics • Multipurpose analgesics based on number and types of studies – – – – Corticosteroids Antidepressants Alpha-2 adrenergic agonists Topical therapies • In populations with serious or life-threatening illness – Corticosteroids most used for multiple purposes – With some exceptions, other drugs used for opioidrefractory neuropathic pain Adjuvant Analgesics for Neuropathic Pain • Initial Strategy – Treat etiology, if possible and appropriate, and titrate opioid – First-line drugs are corticosteroids, anticonvulsants, antidepressants, and topical agents • Corticosteroid depending on clinical setting • Then gabapentin or pregabalin, unless comorbid depression is present • If comorbid depression is present, consider desipramine, nortriptyline, or duloxetine • Always consider co-administered topical drug Adjuvant Analgesics for Neuropathic Pain • Initial Strategy – If first-line drug unsatisfactory, consider sequential trials of adjuvant analgesics, starting with other antidepressants or anticonvulsants – Then consider second-line and third-line drugs – Combination therapy is appropriate as long as each drug is demonstrably effective and tolerated Dworkin RH, et al, Pain, 2007;132:237-251. Finnerup NB, Otto M, McQuay HJ, Jensen TS, Sindrup SH. Pain. 2005;118(3):289-305. Corticosteroids • Multipurpose: Despite limited data, widely accepted as analgesic in Neuropathic pain Bone pain Capsular pain Lymphedema Headache Other conditions • High dose regimen with rapid taper used for • very severe pain Low dose regimen continued indefinitely Anticonvulsants • Gabapentinoids – Work via voltage-gated calcium channel, modulating alpha-2-delta protein – Positive RCT’s Gabapentin: PHN/diabetic neuropathy, neuropathic cancer pain Pregabalin: PHN/diabetic neuropathy/fibromyalgia – NNT less favorable than TCAs, but first-line drug because of safety • Not hepatically metabolized • No drug-drug interactions • Side effects usually tolerable Backonja et al, JAMA. 1998;280:1831-1836. Rowbotham M, JAMA. 1998;280:1837-1842. Caraceni et al, J Clin Oncol, 2004;22:2909-2914. Anticonvulsants • Gabapentinoids – Pregabalin has more stable PK than gabapentin, with easier titration and faster onset of effect than gabapentin – Pregabalin has established positive effects on sleep and anxiety – Individual variation in the response to gabapentin and pregabalin Anticonvulsants • Other anticonvulsants have limited data • and are selected by trial and error Newer drugs have better safety profiles lamotrigine topiramate oxcarbazepine tiagabine levetiracetam zonisamide carbamazepine phenytoin valproate Antidepressants • Classes – Tricyclic antidepressants 3o amine drugs: amitriptyline, imipramine, doxepin 2o amine drugs: desipramine, nortriptyline – SNRIs: duloxetine, venlafaxine, minalcipran – SSRIs: paroxetine, citalopram, others – Others: bupropion Sindrup et al, Basic Clin Pharmacol Toxicol. 2005;96:399-409. Antidepressants • Analgesic efficacy – Studies suggest TCAs > SNRIs> SSRIs Of the tricyclics: 3o amine drugs (amitriptyline) > 2o amine drugs (imipramine) But not all drugs have been studied No comparative studies against duloxetine— now indicated for pain in diabetic neuropathy Of the SSRIs, limited data in support of paroxetine and citalopram Dworkin RH, et al, Arch Neurol. 2003;60:1524-1534. Finnerup NB, Otto M, McQuay HJ, Jensen TS, Sindrup SH. Pain. 2005;118(3):289-305. Antidepressants • Side effects – 3o amine drugs > 2o amine drug > SNRIs/SSRIs/bupropion – CNS, nausea, anticholinergic (TCAs), CV (TCAs), sexual (SSRIs, SNRIs) Dworkin RH, et al, Arch Neurol. 2003;60:1524-1534. Finnerup NB, Otto M, McQuay HJ, Jensen TS, Sindrup SH. Pain. 2005;118(3):289-305. Antidepressants • Based on safety and likelihood of efficacy, most reasonable choices would be 2o amine drugs or SNRIs – – – – – Desipramine Nortriptyline Duloxetine Venlafaxine Also consider bupropion Dworkin RH, et al, Arch Neurol. 2003;60:1524-1534. Finnerup NB, Otto M, McQuay HJ, Jensen TS, Sindrup SH. Pain. 2005;118(3):289-305. Topical Drugs for Neuropathic Pain • RCTs support benefit from diverse drugs classes in acute and chronic pain – Local anesthetics, including lidocaine 5% patch or gel – Capsaicin – Doxepin – NSAIDs, including diclofenac, ibuprofen and aspirin – Nitrates – Opioids Galer et al, Pain. 1999;80:533-538; Ellison et al, JCO. 1997;15:2974-2980; Mcleane, Br J Clin Pharm. 2000;49:574-579; Rowbotham et al, Ann Neurol. 1995;37”246-253; De Benedittis and Lorenzetti, Pain. 1996; 65:45-51. Topical Drugs for Neuropathic Pain • Other topical compounds used for pain – Ketamine – Gabapentin and other anticonvulsants – Other antidepressants Topical Drugs for Neuropathic Pain • Conventional use – Local anesthetics first Lidocaine 5% patch or gel Others – Capsaicin – Doxepin – NSAIDs, including diclofenac, ibuprofen and aspirin Sodium Channel Blockers • Oral mexiletine, tocainide, flecainide are analgesic in neuropathic pain • Efficacy of IV lidocaine supported by RCTs • High side effect liability from oral drugs— generally considered third-line • IV lidocaine is an option for severe neuropathic pain Oskarsson P et al, Diabetes Care, 1997;20:1594-1597. Challapalli et al, Cochrane Database Sys Rev. 2005;CD003345. a-2 Adrenergic Agonists • Multipurpose analgesics but little evidence in the medically ill • In RCT, intrathecal clonidine worked for cancer-related neuropathic pain • Tizanidine usually better tolerated than clonidine • Consider tizanidine if muscle spasm is present Eisenach JC, et al, Pain. 1995;61:391-399. NMDA-Receptor Antagonists • NMDA receptor involved in neuropathic pain and opioid tolerance • Commercially-available drugs Ketamine Memantine Dextromethorphan Amantadine NMDA-Receptor Antagonists • 37 RCTs of ketamine plus opioids by single bolus or infusion show mixed but generally favorable results • 4 RCTs of co-administration to opioids in cancer pain: no conclusion possible • RCT of dextromethorphan positive in DPN and negative in PHN • Very limited positive data for memantine and amantadine; several negative RCTs of memantine Subramaniam K, Anesth Analg. 2004;99:482-495. Bell R, Cochrane Database Syst Rev. 2003;(1):CD003351. Nelson et al, Neurology. 1997;48:1212. NMDA-Receptor Antagonists • Conclusion: Limited data, conflicting • findings Ketamine is used in refractory pain Brief, hours-days, infusion by IV or SQ Oral use of injectable or compounded drug Co-administered benzodiazepine or neuroleptic to reduce risk of side effects • Ketamine is used for palliative sedation Cannabinoids • Strong preclinical support for analgesic efficacy of both CB1 and CB2 agonists • RCTs of THC in central pain • Recent positive RCTs of new formulation (THC plus cannabidiol) in central pain and in cancer pain • Empirical use of THC and nabilone as third-line agents Svendsen et al, BMJ. 2004;329:253. Berman et al, Pain. 2004;112:299-306. GABAergic Adjuvant Analgesics • Baclofen RCT in trigeminal neuralgia Intrathecal baclofen may relieve neuropathic pain apart from spasticity Used empirically for neuropathic pain as third-line agent • Benzodiazepines – Clonazepam used for neuropathic pain despite lack of data Fromm et al, Ann Neurol, 1984;15:240-244. Drugs for IT Administration • Ziconotide Selective N-type calcium channel blocker for use by subarachnoid infusion RCTs support analgesic efficacy • Local Anesthetics • Clonidine • Others Staats et al, JAMA. 2004;291:63. Pharmacotherapy of Neuropathic Pain • Opioids • “Adjuvant analgesics” • NSAIDs NSAIDs in Neuropathic Pain • Generally viewed to be inefficacious but… – Commonly used (e.g., 20% of patients with SCI pain) – Strong evidence of prostaglandin-mediated mechanisms in some preclinical models – Limited positive clinical trial – Conclusion: NSAIDs have a role Wlderstrom et al, Spinal Cord. 2003;41:600. Cohen et al, Arch Intern Med. 1987;147:1442. Non-Drug Strategies for Neuropathic Pain • Interventional • Rehabilitative approaches approaches – Injections – Neural blockade – Neuraxial analgesia – Spinal cord stimulation • Psychological approaches – Orthoses – PT/OT • Complementary and Alternative approaches – Acupuncture – Massage – others Neuropathic Pain in Advanced Illness • Conclusions and overall strategy – Neuropathic pain is common, diverse, poorly understood, newly studied, target of future mechanism-based therapy, now treated by trial-and-error based on limited data – Treatment part of the broader palliative plan of care Neuropathic Pain in Advanced Illness • Conclusions and overall strategy – Management strategy • Treat etiology, if possible • Use opioids • Add systemic and topical adjuvant analgesics • Have a first-line, second-line, third-line strategy for drug • Have a first-line and second-line strategy for non-drug approaches, including interventional pain treatments