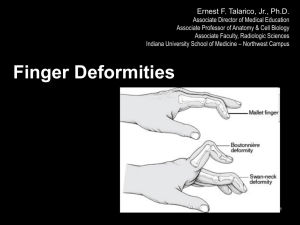
Swan Neck Deformity
advertisement

Swan Neck Deformity Swan neck deformity. The volar plate is torn, causing the joint to open abnormally under the pull of the extensor ligaments . Swan-Neck Deformity • Typically defined as: – proximal interphalangeal (PIP) joint hyperextension – with concurrent distal interphalangeal (DIP) joint flexion • Not necessarily unique to RA but rather an end result of muscle and tendon imbalance caused by RA. Swan-Neck Deformity • Not necessarily unique to RA but rather an end result of muscle and tendon imbalance caused by RA Nalebuff Classification 1989 • Type I - PIP joints flexible in all positions – No intrinsic tightness or functional loss • Type II - PIP joint flexion limited in certain positions – Intrinsic tightness – Limited PIP motion with extended MCP with ulnar deviation • Type III - PIP joint flexion limited in all positions – Near normal radiograph • Type IV - PIP joints stiff with poor radiographic appearance Pathophysiology • The intercalated joint collapse concept of Landsmeer means that collapse of a joint in one direction will result in deformity of the next distal joint in the opposite direction. – Z deformity Pathophysiology • In a normal finger, intrinsic muscles serve as: – flexors of the MCP joint – extensors of the PIP and DIP joints • By being located volar to the MCP joint axis and dorsal to the PIP and DIP joint axes Pathophysiology • Intrinsic tightness increases the flexor pull on the MCP joint and hyperextension of PIPJ • Weak flexor power aggravates this by being unable to pull the middle phalanx. – DIPJ and MCPJ hyperextension follows • Constant efforts to extend the finger against this pull then leads to stretching of the collateral ligaments and weakening of the volar plate at the PIPJ. Pathophysiology • the lateral bands are constrained in their dorsal position with the extensor apparatus migrating proximally – therefore upsetting the flexor-extensor balance, • The lateral bands in this position act to increase the pull of the central slip that attaches to the dorsal base of the middle phalanx. – Leading to hyperextension of PIPJ Pathophysiology • The increase of FPL tension resulting from hyperextension of the PIP joint leads to a reciprocal flexion of the DIP joint. • DIP mallet deformity also from: – Joint erosion – Extensor tendon attentuation or rupture • Progressive disease leads to joint destruction and fixed contracture. Hashemi-Nejad and Goddard (1994) -multidisciplinary approach is best -an affected joint will affect other joints -early synovectomy is worthwhile after a 6-month trial of non-operative treatment -tenosynovectomy decreases the risk of tendon rupture, -the wrist is the key in the RA hand -the thumb is a very important source of disability -silastic MCPJ arthroplasty is successful in reducing pain and improving function Feldon (1993) lists the aims of surgery in the RA hand: 1. 2. 3. 4. pain relief functional improvement preventing disease progression cosmetic improvement Note that the presence of a painless deformity with minimal function deficit is not an indication for surgery. Management • Millender and Nalebuff staging system (1975) is a good guideline for identifying treatment options in RA Principles • Prevention • Correct PIPJ hyperextension • Restore DIPJ extension Type1 – – – – – Silver ring splint to flex PIPJ Volar dermatodesis Correction of any MCPJ abnormality first Flexor tenosynovectomy (if synovitis is present) Flexor tenodesis - FDS slip through A2 pulley then looped back to itself – Retinacular ligament reconstruction – Release ulnar lateral band proximally and pass volar to PIPJ axis sheath Silver Ring Splint • Permit active PIP flexion and limit hyperextension of the PIP joint • DIP Fusion • Difficult and unreliable to restore the extensor apparatus at DIP level cause underlying RA disease will destroy the repair • Also secondary arthritis within DIP may make attempts to mobilise joint unwise • Dermadesis • Used to prevent PIP hyperextension bu creating a skin shortage volarly • Elliptical skin wedge (4-5mm at widest) is removed from volar aspect of PIP • Care not too disturb venous drainage or violate the flexor sheath • Skin closed with PIP in flexion • Only useful if done in conjunction with other procedures ie DIP fusion Flexor Tendon Tenodesis “sublimis sling” • Used as checkrein against hyperextension ie restoration of strong volar support • One slip of FDS is divided ~1.5cm proximal to PIP • This is then separated from its corresponding slip bit left attached distally • With joint at 20-30 degrees the detached slip is fixed proximally – Anchored to thickened margin of sheath, distal edge of A2 or Mitek • Nalebuff did simpler procedure whereby he passed split tendon around A1 pulley Reticular Ligament Reconstruction • Credited to Littler • Ulnar lateral band is freed from extensor mechanism proximally but left attached distally • Passed volar to Cleland’s fibres to bring it volar to axis of PIP • Band is sutured to the fibrous tendon sheath under enough tension to restore DIP extension and prevent hyperextension at PIP • However, in RA may have destruction of terminal tendon so no amount of tension applied to the relocated tendon will achieve DIP extension Type 2 • Looks like Type 1 but PIP movement is limited in certain positions related to position of MCPJ – MCPJ extended/radial deviation then limited passive PIP ROM – MCPJ flexed/ulnar deviated then PIP ROM increased • As MCPJ subluxates and the intrinsics get tight a secondary swan neck develops as a result of muscular imbalance • Not sufficient to restrict PIPJ hyperextension, intrinsics must be released plus MCPJ subluxation must be corrected +/- arthroplasty Intrinsic Release • Photo on camera • A rhomboid portion of the ulnar extensor aponeurosis is then resected • This procedure resects the lateral band through which the abnormally tight intrinsics have caused MP flexion and PIP hyperextension Type 3 • unlike type 1 & 2 have significant functional disability due to inability to grasp objects • Not joint destruction but restriction due to: – Extensor mechanism – Collateral ligaments – Skin • First goal is to restore passive ROM – – – – PIPJ manipulation Skin release Lateral band mobilisation Then correction of deformity after motion restored PIPJ Manipulation • MUA possible up to 80-90 degrees • Usually in conjunction with intrinsic release, arthroplasty or tenosynovectomy Skin Release • Dorsal skin may limit the amount of passive flexion that is achieved during manipulation • Tension minimised with an oblique incision just distal to the PIPJ – Allowing skin edges to spread – Closes 2-3 weeks by secondary intention – PHOTO 2112 Lateral Band Mobilisation • Lateral bands are displaced dorsally • Free lateral bands from central slip using 2 parallel incisions allows flexion without releasing lateral bands or lengthening central slip • PHOTO 2113 Type 4 • Patients with stiff PIPJ and radiographic evidence of advanced intra-articular changes require salvage procedure – Fusion or arthroplasty • PHOTO 2114