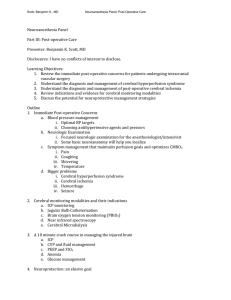
SAH & TCD -Dr.Nikhil Cerebral arterial anatomy SUBARACHNOID HAEMORRHAGE • not into the brain parenchyma • incidence of SAH is around 6/100,000 • F/M 1.24 : 1. Age 40-60yrs • mortality is 50%, of which 15% die before reaching hospital, with up to 30% of survivors having residual deficit-producing dependency. PATHOLOGY • saccular (berry) aneurysms (85%), • non-aneurysmal perimesencephalic haemorrhage (10%) • arterial dissection, cerebral or dural AVMs, mycotic aneurysm, pituitary apoplexy, vascular lesions at the top of the spinal cord and cocaine abuse • bifurcations in the circle of Willis • congenital weakness in the tunica media, • Sudden hypertension plays a role in causing rupture, RARE CLINICAL PRESENTATION • ‘thunderclap’ headache developing in seconds f/b • period of depressed consciousness for less than 1 hour in 50% of patients, with focal neurology in about 30% of patients • Meningism – neck stiffness, photophobia, vomiting and a positive Kernig’s sign,brudzinki sign – is common in those patients with higher GCS • Atypical features – Seizures, acute encephalopathy Focal physical findings in SAH CT IMAGING first diagnostic tool Blood-hyperdense excluding other pathologies Sensitivity -98.7% <6hrs -85.7%@24hrs -50%@7days Pattern of hemorrhage • false-positive - severe generalised oedema resulting in venous congestion in the subarachnoid space. • false-negative 2%. Small amounts of blood may not be detected, Lumbar puncture TIMING – ATLEAST 12 HOURS AFTER RUPTURE suspicion of SAH is high despite a negative CT LOOK FOR 1) RBC2) xanthochromia presence of RBCs>2,000 × 106 in the fourth tube Oxyhemoglobin- bilirubin – xanthochromia Spectrophotometry-Oxyhemoglobin of traumatic tap Vs bilirubin of SAH exclude infection CT ANGIOGRAPHY Alternative to LP after a negative non-contrast CT When Lumbar puncture C/I post-test probability of disease of < 1%( below which no further investigation is required) sensitivity of CTA is 92.3% for aneurysms < 4mm MR ANGIO 95% sensitive aneurysms > 3 mm atypical cases long delay DSAngiography DSA is the diagnostic tool of choice in cases where CTA is still inconclusive ED Management • ABC and EVD (High grade acute SAH) • Intubation - low GCS/protect the airway • stabilization of hemodynamics/risk for neurocardiogenic stunning • next priorities -reduce SBP and reverse anticoagulation to mitigate the risk of aneurysm rerupture • BP control : SBP< 160 / MAP < 110 mm Hg Labetalol /Nicardipine/hydralazine • Pain control/Antiepileptics – poor Neurological exam or high SAH • Disease Severity Scoring • Admission/transfer to high volume centre Nicardipine 5mg/h IVmay increase by 2.5 mg/h q5– 15 minutes (min); Max: 15 mg/h), labetalol (start 20 mg IV ,40–80 mg iv q 10 min; Max 300 mg/total dose; clevidipine (start 1–2 mg/h IV double rate q 90 sec; max:32 mg/h) hydralazine -setting of bradycardia Nitroprusside and nitroglycerin should be avoided(vasodilatory and inc ICP) phenytoin (load 10–20mg/kg IV max: 50mg/min), fosphenytoin (10–20 (PE)/kg IV; over 30 min; max: 150mg PE/min) and levetiracetam (15–20mg/kg over 30 min). Fentanyl/paracetemal 1967 HESS & hunt scale Higher grades - associated with increased surgical risk for the repair of ruptured intracranial aneurysms 1975 Glasgow Coma Scale (GCS) 1988 - World Federation of Neurosurgical Societies (WFNS) 1980 – fisher CT GRADING scale Modified fisher scale Over the last 30 years, it has become clear that the greater the amount of blood within the basal cisterns, the greater the risk of vasospasm. Ogilvy & carter grading – OUTCOME PREDICTION age>50/ HHS 4,5/ fs 3,4 /size>10mm COMPLICATIONS REBLEEDING - 9%–17% first few hours/ AHA- “For patients with an unavoidable delay in obliteration of aneurysm, a significant risk of rebleeding, and no compelling medical contraindications, short term (< 72 hours) therapy with tranexamic acid or aminocaproic acid is reasonable to reduce the risk of early aneurysm rebleeding” (Class IIa recommendation;level of evidence B) • ε-aminocaproic acid: 4 g IV loading followed by 1 g/h continuous IV infusion. Stop the infusion prior to obliteration of the aneurysm ACUTE HYDROCEPHALUS -15-20% first 24 hours/ characterised by a drop in the GCS /sunset eyes /ventricular drain . • Syndrome of the Trephined (Sinking Skin Flap Syndrome) paradoxical herniation after CSF diversion DELAYED CEREBRAL ISCHAEMIA 30% onset of focal neurological deficit, a drop in GCS by 2 or more points, cerebral infarction that occurs typically 4–12 days post SAH unrelated to aneurysm treatment or other causes hydrocephalus, cerebral oedema or metabolic disorder PARENCHYMAL HAEMATOMA 30% worse prognosis mass effect - evacuation and simultaneous clipping Definitive treatment • Multidisciplinary Neurosurgeon/Interventionali st/Neurointensivist • Coiling vs Clipping – Patient age, aneurysm morphology and location, comorbidities ISAT trial lower rate of dependence,mortality and seizures in coiling group. However, non complete obliteration and rebleed higher. Overall, coiling preferred to clipping when feasible. ICU Management : Neurologic complications ?(A-comm) - coiling - ICU - ICP of 50 to 55 mm Hg / MAP of 100 mm Hg Antishivering first battle -against elevated ICP – stepwise approach methods negative impact on the CPP Skin counterwarming IV magnesium EVD/Surgical Decompression Buspirone, IV dexmedetomidine Step 1: Sedation with Short-Acting Agents IV meperidine IV propofol: 1 to 2 mg/kg initial bolus, maintenance 5 to 50 μg/kg/min IV propofol IV clonidine IV midazolam: Load 0.01 to 0.05 mg/kg ,maintenance 0.02 to 0.2 μg/kg/h IV fentanyl: IV bolus 25 to 100 μg, followed by maintenance 1 to 3 μg/kg/h Step 2: Hyperventilation and Order Osmotic Agents Hyperventilation-refractory ICP crisis and brain herniation/Target end-tidal PCO2, 30 mm Hg Mannitol: 1 to 1.5 g/kg,q6h Hypertonic saline (HTS): Avoid serum Na > 155 mEq/L. Step 3: Barbiturate Coma Pentobarbital: Load 10 mg/kg IV infusion over 1 hour, maintenance 1 to 3 mg/kg/h Step 4: Therapeutic Hypothermia 32-34°C CPP Optimization • ICP, 40 mm Hg; MAP, 90 mm Hg; a CPP, 50 mm Hg, ?icp/start vasopressor • systemic hypotension + high ICP + low CPP ?icp/start vasopressor • Systemic hypotension and uncontrolled ICP Worst combination MAP- 100 ICP-15= CPP > 85 Pbto2 < 15 mm Hg, and the LPR is > 50? Improve brain oxygenation reduce brain metabolic stress Delayed cerebral ischemia • Defined as any neurological deterioration ( focal or global ) presumed secondary to cerebral ischemia that persists for more than an hour and cannot be explained by any local/systemic complication. • Diagnosis of exclusion – Hydrocephalus/Seizures/Sedation/Metabolic • ~ 30% of patients • Pathophysiology • Risk for vasospasm increases with thickness, density, location and persistence of subarachnoid blood • Poor clinical grade, h/o LOC, smoking, cocaine, hyperglycemia, SIRS, hydrocephalus increase risk of delayed cerebral ischemia. DCI - Management • Prophylaxis : Nimodipine 60 mg q 4 hrly. Euvolemia • Monitoring : Clinical checks q 2hrly : CT @ 24 hrs after securing aneurysm, 3-5 and 7-10 days : TCD – Mean Cerebral blood flow velocity < 120 cm/s – No vasospasm > 200 cm/s – Vasospasm Rise > 50 cm/s in 24-48 hrs – High risk LindeGaard Ratio > 3 –Vasospasm : CTA/DSA : EEG/Brain tissue O2 monitoring • Vasospasm Watch Period-typically bleed days 4 to 14, but can occur as late as day 21 patient does not have any signs (clinical, TCD, CTA/P, or cEEG findings) of vasospasm Euvolemic Maintain normal BP Normal CO and index WHAT IF SIGNS + Hypervolemic Hypertensive Hyperdynamic cardiac perf. Avoid anemia Hgb < 7. • Avoid low PAWP < 10. • Avoid low GEDVI < 680 mL/m2. • Avoid high SVV and PPV > 13%. • Avoid low SVI < 40 mL/m2. • Avoid low UO< 0.5 mL/kg/h. MAP, 60 to 90 mm Hg CO, 5 to 8 L/min • CI, 3 to 5 L/min/m2 Invasive therapeutic options for symptomatic vasospasm Intraarterial (IA) therapy-papaverine, nicardipine, verapamil, milrinone and nitroglycerin :positive effect may not last long Balloon angioplasty :SAFETY Intrathecal Infusion and Basal Cistern Implants of Calcium Channel Blockers:nicardipine Intra-aortic Balloon Counterpulsation Therapy : neurogenic stunned myocardium /allow continuation of triple-H therapy • NeuroFlo Device:acute phase of ischemic brain injury. SENTIS ? Mg, ? Statins , ? Endothelin antagonists Systemic complications and management • Cardiopulmonary • Fever • Thromboembolism : SCD , UFH after securing aneurysm. • Glucose abnormalities : Target 80-180 mg/dL • Hemoglobin : 8-10 g/Dl • Hyponatremia : SIADH vs Salt wasting . Neurogenic Stunned Myocardium • takotsubo cardiomyopathy/broken-heart syndrome/contraction band necrosis syndrome/ Gebrochenes-Herz syndrome • stress is mediated by the brain -acute SAH with intense ICP elevation, inflammation, and sympathetic surge • not to be induced by coronary artery atherosclerosis or plaque rupture as in typical acute coronary syndrome (ACS). • Normal base, abnormal apex • triple-H therapy - >HARMFUL systemic hypotension forward/systolic failure with severely depressed EF new-onset heart failure nonspecific T-wave “cerebral T”or ST- abnormalities Point-of-care transcranial Doppler • 1982, Aaslid et al. introduced • Principle: Doppler shift (ΔF). Technique • 2 MHz ultrasound probe /4 MHz or more for extracranial vessels • Acoustic windows - transtemporal, transorbital, suboccipital and submandibular windows • Depth to the distance of the third ventricle • color Doppler box over the top half of the screen (near field) where the MCA is located, just lateral to the cerebral penducles • Insonate ACAs (anterior angulation, depth 6–7 cm), • Terminal ICAs (caudal angulation, 6–7 cm), and • PCAs (posterior angulation, 5.5–7.5 cm), In order to identify the intracranial arteries 1. Acoustic window through which the vessel is insonated 2. Depth of sample volume 3. Transducer orientation during insonation 4. Direction of blood flow with respect to the transducer 5. Relationship of the vessel to the junction of MCA,ACA,ICA 6. Response to dynamic manoeuvres (e.g., compression of the common carotid artery resulting in a temporary decrease in ipsilateral MCA velocity). GOSLINGS PI = PSV-EDV/MFV 0.5-1.19 PSV EDV MDV TAPV/MFV PI HR Duplex sonography refers to the use of TCD machine for study of flow velocities along with tissue imaging. power-motion mode Doppler (PMD) provide information about the complete length of an artery. SIMULATION Vasospasm • inverse relationship between cerebral blood vessel diameter and TCD mean velocities, we are able to quantify and subcategorize vasospasm Progressive increase of mean velocities during the early stages of SAH to predictive of vasospasm change in baseline mean velocity of 21 cm/s per 24 h in the first 3 days to be diagnostic of vasospasm Lindegaard Ratio helps differentiate between hyperemia versus the onset of true vasospasm Vasospasm: limitations • trans-orbital and trans-foraminal windows are less reliably insonated compared to the trans-temporal window • ACA and PCA are less sensitive and specific for vasospasm compared to the MCA. • basilar artery and vertebral artery with lower sensitivity and specificity • blood flow may be influenced by many factors (PaO2, PaCO2,blood viscosity, collateral flow) • operator experience is required Midline shift • Any amount of midline shift is considered abnormal, but poor neurological outcome can be associated witha clinically significant midline shift of as little as 0.5 cm If positive, MLS is away from the ipsilateral sid presence of hydrocephalus of the third ventricle does not have much bearing on the MLS measurement Intra-cranial pressure • rough estimate for ICP, to help rule-in high ICP, GOSLINGS PI • systolic velocity increases- diastolic flow becomes decreased/blunted • Recommendations ICP and CPP trends THAN ICP absolute values LIMITATIONS: PI affected by Paco2 and MAP NON PULSATILE FLOWS Cerebral circulatory arrest • step-wise changes in cerebral blood flow • decreasing or blunted diastolic flow, oscillating flow (diastolic flow reversal),sharp systolic peak flows, then finally, zero FLOW Cerebral circulatory arrest criteria by TCD Certain situations (i.e., presence of spinal reflexes, drug ingestions, and profound hypothermia/ shock) may lead to confounding with brain death determination if relying on clinical testing alone. If TCD rules in arrest by non-reassuring MCA flows, ancillary testing (4-vessel cerebral angiography, nuclear medicine radionuclide brain perfusion scan, CT or MR cerebral blood flow angiography) could be sought to formally confirm the diagnosis TCD evaluates cerebral circulatory arrest, not brainstem function. medical jurisdictions will not accept a TCD as its own ancillary test to confirm brain death save premature,unnecessary serial ancillary tests, until the diagnosis can be first confirmed on TCD MILRINONE LACTATE INJECTION • inotropic/vasodilator, improves diastolic function, not a beta-adrenergic agonist, no increased effect on myocardial oxygen consumption • Phosphodiesterase III inhibitor • LOADING DOSE 50 mcg/kg maintainence :0.2 mcg/kg/min to 0.7 mcg/kg/min • elimination half-life of 2.4 hours • excretion is via urine • contraindicated in patients who are hypersensitive Tachy arrythmias Hypotension Headaches NIMODEPINE • calcium channel blocker • oral dose is 60 mg (two 30 mg capsules) every 4 hours for 21 consecutive days , within 96 hours of SAH • orally or via a naso-gastric tube • hepatic cirrhosis - 30 mg capsules every 4 hours ( CLEARANCE ) ADVERSE EFFECTS Take home points SAH –more common in F>M 40-60ys age ,mortality >50% HTN,smoking ,alchol,cocaine are only modifiable risk factors saccular (berry) aneurysms (85%) Thunderclap headache + meningism +unconsciousness favour SAH CT IMAGING – FIRST DIAGNOSTIC TOOL 98.7% <6hrs Lumbar puncture TIMING – ATLEAST 12 HOURS AFTER RUPTURE DSA is the diagnostic tool of choice where CTA is still inconclusive HHS - increased surgical risk for the repair GCS & WFNS - long term outcome MFS – vasospasm REBLEEDING - 9%–17% first few hours/ tranexamic acid or aminocaproic acid ACUTE HYDROCEPHALUS -<24hRS – EVD ISAT trial - coiling preferred to clipping when feasible OPTIMIZE –icp/cpp/MAP/pbo2/LPR Vasospasm Watch Period-typically bleed days 4 to 14, but can occur as late as day 21 No prophylactic HHH therapy Hyponatremia : SIADH vs Salt wasting takotsubo cardiomyopathy - systemic hypotension + forward/systolic failure with severely depressed EF <40% • TCD -Principle: Doppler shift (ΔF). • TAPV/MFV –lindegard ratio –vasospasm vs hyperemia • Sensitivity and specificity more for MCA for detecting vasospasm • GOSLINGS PI = PSV-EDV/MFV –----- ICP • Lindegaard Ratio helps differentiate between hyperemia versus the onset of true vasospasm • Tcd – icp/mls/cerebral circulatory arrest • Nimodepine and milrinone shown promising results others need further trials for safety