So Clinical Biochemistry is easy?
advertisement

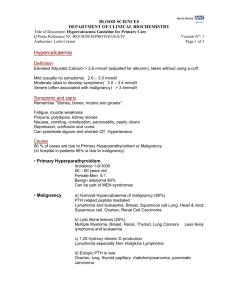
Interactive Cases Gordon Challand Royal Berkshire Hospital Format I will present some cases taken from the UK NEQAS Interpretative Comments scheme Participants will be asked a range of questions on each case (totally non-threatening!) Learning points will be summarised Case 1: low calcium A 16 year old man presenting to his Family Doctor. No clinical details are given on the request card. Serum results are Sodium 139 mmol/L; potassium 4.1 mmol/L Urea 2.1 mmol/L; creatinine 61 umol/L Albumin 40 g/L; adjusted calcium 1.33 mmol/L Bilirubin 8 umol/L; ALP 238 IU/L; ALT 20 IU/L The calcium result was analytically checked, and magnesium and phosphate were added Magnesium 0.71 mmol/L; phosphate 2.14 mmol/L Which of the 3 comments is the best? 1: Very low calcium. ? Contamination of sample. Please send repeat with clinical information 2: Results could be consistent with hypoparathyroidism or pseudo hypoparathyroidism. Suggest PTH analysis. Alk Phos appropriate for age 3: Results consistent with PTH deficiency (ALP may be normal for age). Suggest repeat calcium, albumin and phosphate; and check PTH and 25-hydroxy vitamin D at same time. Please give clinical details And which comment is the worst? Learning points: Case 1 Sample contamination with EDTA unlikely with a normal potassium and normal/raised alkaline phosphatase Calcium lower than expected for Vitamin D deficiency (but this possibility should be mentioned) Urgent referral to hospital Repeat adjusted calcium 1.28 mmol/L PTH elevated at 75.3 pmol/L On referral, classical clinical history and findings of pseudohypoparathyroidism Case 2: high calcium A 60 year old woman seeing her GP; clinical details are ‘raised calcium, cause?’ Sodium 136 mmol/L Potassium 4.0 mmol/L Urea 3.7 mmol/L Creatinine 57 umol/L Adjusted calcium 2.67 mmol/L Phosphate 1.12 mmol/L PTH 5.1 pmol/L (1.0-7.2 if normal calcium) TSH, LFTs within reference limits Case 2: likeliest diagnosis? Please choose a number to select what you consider to be the likeliest diagnosis 1: Familial hypocalciuric hypercalcaemia 2: Malignancy 3: Primary hyperparathyroidism 4: Hypercalcaemia secondary to thiazides 5: Any other condition Case 2: which of the 3 is the best comment? 1: Calcium remains high. Normal renal function. Primary hyperparathyroidism excluded. ?on diuretics. Malignancy should be excluded. ?haematology results 2: PTH inappropriate for calcium. ?primary hyperparathyroid. ?Fam hypocalciuric hypercalcaemia: please send paired fasting serum and urine 3: PTH inappropriately high for raised calcium. Possible primary hyperparathyroidism Raised calcium: diagnostic probabilities Calcium (mmol/L) % likelihood of:1HPTism malignancy Vit D toxicity 2.6 – 3.0 55 23 19 3.1 – 3.5 43 41 11 Learning points Malignancy is less common than hyperparathyroidism as a cause of hypercalcaemia in otherwise well patients Thiazides are a common cause of mild hypercalcaemia Primary hyperparathyroidism can be indistinguishable from FHH on the basis of serum calcium and PTH measurements alone Debate continues as to whether treatment is required for either FHH or primary hyperparathyroidism in asymptomatic patients Case 3: worried about acne A 19 year old woman presented to her GP. Clinical details were ‘worried about acne and lowish weight: eating well’. Serum results were Sodium 140 mmol/L Potassium 3.1 mmol/L Urea Creatinine 87 umol/L Glucose 4.5 mmol/L 7.4 mmol/L Bicarbonate 36 mmol/L Albumin 43 g/L Normal LFTs, TFTs EQAS participants’ comments included the following three. Which do you consider the most appropriate? 1: Hypokalaemic alkalosis: first consider vomiting, diuretic/laxative therapy/abuse. If hypertensive, consider investigate for mineralocorticoid excess. Euthyroid 2. Clinical picture and hypokalaemic alkalosis may suggest ectopic ACTH. Suggest referral to endocrinologist 3. Hypokalaemic alkalosis with mildly raised urea suggests possibility of recurrent vomiting, laxative or diuretic abuse Case 3: other diagnoses suggested by participants Cushing’s syndrome Leukaemia Bartter’s syndrome Stress Gitelman’s syndrome Pyloric stenosis Liddle’s syndrome Case 3: other investigations suggested by participants Urine potassium Androgen profile Magnesium Urine chloride 17-OH progesterone Oestradiol Renin/aldosterone ratio 09.00 and 24.00 cortisols etc Case 3: learning points Exclude common conditions first Diuretics are not easily available Aldosteronism is probably underdiagnosed Case 4: jaundiced A 54 year old man visited his GP. Clinical information was ‘jaundice’. Serum results were Sodium 144 mmol/L; potassium 3.6 mmol/L Urea 5.0 mmol/L; creatinine 87 umol/L Albumin 41 g/L; bilirubin 140 umol/L ALT 35 IU/L (7-56); Gamma-GT 35 IU/L (15-73) Alkaline phosphatase 58 IU/L (38-126) Which other test would be most appropriate? 1: FBC 2: Conjugated bilirubin 3: Haptoglobin 4: LDH 5: Other Which of these 4 comments is most appropriate? 1: Check conjugated bilirubin and consider haemolysis. Could be biliary despite no elevation in Alk. Phos. and gamma-GT 2: ?massive IV haemolysis ?adverse transfusion reaction (E. coli unlikely with normal urea). Diffuse hepatocellular damage? 3: Hyperbilirubinaemia with no enzyme abnormality. Gilbert’s unlikely with a bilirubin of 140. Measure conjugated bilirubin. ?Haemolytic anaemia (HB/FBC) or idiosyncratic reaction to drug (check drug history) 4: Add conj bili before reporting. If low ‘bilirubin conjugation problem exacerbated by recent stress?’ If high ‘liver dysfunction due to drugs, virus or other cause?’ What is the likeliest cause of an isolated raised bilirubin? 1: Haemolytic disorder 2: Gilbert’s syndrome 3: Cholestasis 4: Other Case 4: further information A conjugated bilirubin was added which was low LDH was high Normal haemoglobin; decreased red cell count and haematocrit With this new information, what is the likeliest cause of the raised bilirubin? 1: Haemolytic disorder 2: Gilbert’s syndrome 3: Cholestasis 4: Other Case 4: further action The Duty Biochemist asked for a blood film to be examined This showed the presence of spherocytes and a diagnosis of hereditary spherocytosis was made Case 4: learning points It is important to measure conjugated bilirubin when the cause of a raised total bilirubin is not clear Unconjugated bilirubin is high in both haemolysis and Gilbert’s syndrome Gilbert’s syndrome is unlikely with such a high bilirubin Haematology can help! Case 5: renal diabetic disease A 36 year old woman seeing her GP. Clinical details were ‘renal diabetic disease’. Results were Serum creatinine 51 umol/L (62-133) Urine creatinine 7537 umol/L Urine flow 1.4 ml/min Creatinine clearance 214 ml/min (70-120) Case 5 comment assessment Mark each of the following 4 comments on a scale from 1 (inappropriate) through 2 (no added value) to 5 (highly appropriate) Case 5 comments More than complete urine collection? Pregnant? Although hyperfiltration can occur in the early stage of renal diabetic disease, this clearance seems too high to be credible. More than complete collection? Artefactually reduced serum creatinine? Hyperfiltration consistent with early diabetic renal disease. Suggest monitor urine albumin. Measure urine albumin to check diagnosis, as Cr clearance not consistent with RDD and is unusually high even if lady were pregnant. Is low Cr simply due to low muscle mass? Is urine volume correct? Case 5 learning points 24 hr urine creatinine output is a reasonable guide to adequacy of a 24 hour collection Hyperfiltration can occur in the early stages of renal diabetic disease For this patient, it is likely that there is both hyperfiltration and a more than complete urine collection It is important to monitor urine albumin in such patients The importance of a comment Some clinical activity has a background of ‘I do not know what is wrong with this patient: I will carry out tests which may suggest a diagnosis’ Some clinical activity has a background of ‘this is my provisional diagnosis: what evidence can I gather to prove it right?’ Compared with a conventional approach, the Clinical Biochemist has to make a conceptual switch: ‘here is some clinical information and a set of abnormalities: what could cause them?’ Taking account of both laboratory and patient variability, and giving our opinion on results has an irreplaceable role in patient care. The ‘bad’ comment Can often be classified as: Asinine, oBvious, Crass, Dogmatic, Erroneous, Foolhardy; or Gobbleygook Often ignores clinical information Often ignores the recipient of the report Often contains jargon or incomprehensible abbreviations A single foolhardy suggestion can ruin an otherwise good comment The ‘good’ comment In general, the comment scoring highest tends to suggest: The most probable diagnosis or diagnoses Add-on tests to distinguish between the diagnostic possibilities Shows good communication skills and avoids jargon and incomprehensible abbreviations Clinical Biochemistry is not easy! There is always more than one explanation for any given findings Connecting results to clinical information requires an enormous knowledge base and very considerable interpretational skills Our role is unique and of major importance. We often do not give ourselves enough credit for it! Thank you for listening