Cervical Screening RCN Guidance for Good Practice, December 2006
advertisement
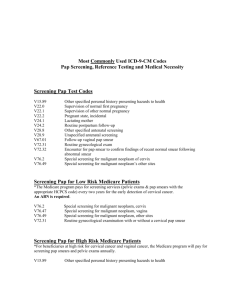
Taking a Cervical Sample Cervical Screening QARC Training School October 2012 Cervical Cancer Risk Factors • • • • • • • Never had a cervical screen Infection particularly HPV Smoking Contraception Pregnancy Sexual behaviour Immunosuppression Taking a Cervical Sample • A Screening test should be taken in such a way as to provide an adequate sample for assessment with the minimum of distress or discomfort. Cervical Screening RCN Guidance for Good Practice. December 2006 The environment • • • • • • Privacy Warmth Lighting Relaxed atmosphere Comfort Modesty blanket The equipment • • • • • • • • • • Specula (Disposable) Waste disposal Sampler (check condition of brush) Pot with Fixative solution (check the expiry date) Lubricant Ball point pen Forms (Open Exeter) Gloves (including latex free) Leaflets including ‘The Facts’ Good light source The woman • Welcome • Check identity – do not complete form before woman is present • Explanation • Information • Answer questions • Obtain informed consent Taking a history • Obtain and record relevant details • Any abnormal bleeding i.e. heavy periods, post coital, intermenstrual or post menopausal bleeding and/or unusual vaginal discharge • Consider if a cytology sample is still appropriate – or should direct referral to COLPOSCOPY be considered? Taking a history cont … • Check on contraception - is she taking COC, POP, Depo Provera, IUCD, Mirena, implant? • Is she on HRT/Tamoxifen? • If not using pre-populated form i.e Open Exeter or Ice, details of past screening hx/treatment/follow-up should be recorded Preparation of the form • Woman’s current full name, previous name, address with postcode, date of birth • NHS number • Name & address of GP and GP code • Personal sample taker code • Clinic number, if appropriate • Date of last sample • Past history of abnormal sample, and details • First day of last period • Abnormal bleeding • Use of hormones, IUCD etc • Clinical details, e.g post-natal status if less than 3/12 Labelling the sample • Pre-printed labels maybe used (but details must be clarified with patient and initialled) • Write clearly in ball point pen • Surname & Forenames • Date of birth • NHS Number To Print HMR from Open Exeter and view screening history Guidance for Practice Staff • • • • • • • • • • • • • • Adobe Reader has to be installed on your PC. You can download this for free by going to https://nww.adobe.com/products/acrobat/readstep2.html and following the instructions on screen Quick tip – do remember to enable pop up boxes otherwise you will not be able to print the form Go to:https://nww.openexeter.nhs.uk/nhsia/index.jsp Same password and log-in for Open Exeter In Application drop down box choose Patient Details Press CONTINUE box Select Patient by inputting her NHS Number if available. Otherwise input her surname, forename and date of birth Press SEARCH From the choice displayed in box situated top left hand corner of screen choose either HMR101 form – editable or HMR101 form – A5PDF (2009) Press CONTINUE box If you have chosen HMR101 form A5PDF(2009), the form you wish to print will be displayed on screen. You cannot make any amendments on screen to this form Press the printer icon at the top of the page You need to print the form at the top of a piece of A4 – remember to have the paper in portrait, not landscape Go to properties, Paper/Quality = A5, Effects = Print Doc on A5, Finishing = Portrait. This last instruction applies to the printer used at the screening department – depending on which printer you use, this could vary. It is essential to complete the following fields on the form when you have taken the sample: Source of sample Sample Taker Sample Taker code Implement used Specimen type Condition Clinical Data – 360 sweep, Cervix visualised and Date of this Test Choosing the speculum Points to consider : • Age of women • Build of women • Parity • A range of sizes should be available from virgin to Winterton Visualising and assessing the cervix • Positioning the woman • Inspecting the vulva • Locating the cervix by speculum or digital examination • What to do if you can’t find the cervix • Visualising the cervix • Assessing the cervix • Interpreting what is seen Choosing the sampler • A Cervex brush must be used • Consider using an Endocervical Brush IN ADDITION TO A CERVEX BRUSH if there is stenosis of the os, or to pick up glandular cells when following up a previous glandular abnormality • An endocervical brush should never be used on its own • Consider the state of the os • Look at the shape and contours of the os • The transformation zone • Any unusual features Sampling the cervix • Technique • Lubricants – use sparingly, if at all – water soluble single use sachet • 360 degree sample x 5 with cervex brush/cervex broom • 90 degree turn with endocervical brush if used • Adequate pressure (pencil like) • Transformation zone Practical tips for difficult samples • • • • • • • Ask woman to cough Clenched fists or pillow under buttocks Winterton speculum Condom or glove Digital examination Seek help – it’s ok to ask! Refer to Colposcopy Bi-manual examination • Bi-manual examination is NOT necessary when undertaking cervical screening and is not a prerequisite for the sample taker. Digital examination may only be necessary to assist in the location of the cervix, and not as a means of physical assessment that will aid diagnosis. Cervical Screening RCN Guidance for Good Practice, December 2006 • Further training must be undertaken prior to performing Bi-manual examination. The sample • A high cellular yield will be achieved with correct use of the Cervex brush • Rinse the Cervex brush into the Thin Prep vial using a vigorous swirling motion • Agitate the brush forcefully at least 10 times in the preservative liquid • Check the brush to ensure that no material is clinging to the fronds. • Screw the lid on until the black marks meet or just beyond • Ensure fluid level in vial is visible – do not completely obscure with the label • Ensure vial is correctly and clearly labelled Basic Sample Method • Insert longer central bristles into cervical os • Turn in clockwise direction pushing onto the cervix X 5 rotations • The lateral bristles will splay over the ectocervix Stenosed Os • MUST be used TOGETHER 1st then 2ND Endocervical Canal Sampling • AFTER Cervex Brush – insert endocervex brush until flange is at entrance to canal Rotate 1x90° in clockwise direction • Samples from BOTH brushes go into the same vial and should be clearly indicated on the form Wide Ectropian + • Use cervix brush first to sample • If required a second Cervix Brush can be used to sample the wide transformation zone – this should be collected by sweeping the transformation zone at least twice • Material sampled from both brushes should be put in the same vial and clearly indicated on the form Transformation Zone Post-menopausal Women • • • • • Difficult to sample Thinner squamous epithelium Atrophic changes Painful for the Patient SCJ difficult to visualise Ending the consultation The woman must understand • That a sample has been taken • How she will receive her result • A brief outline of the possible results and follow up • That help, support and written information are available • Double check details and completion of form and pot!!! Completion of the sample request form (HMR101) • On the sample form note if the sample is cervical or vault • Tick that you have visualised the cervix and taken a 360 degree sweep x 5 • Note the appearance of the cervix • Abnormal bleeding on taking the sample • Abnormal discharge • Use of additional sampler (endocervical brush) • Insert your Sample Taker Number (mandatory) • Sign own name and date form Documentation • Record in notes &/or computer • Visualisation of cervix & sampling of TZ • Date sample taken and by whom • Any pertinent comments related to the procedure or what you have seen • Audit General points for discussion • • • • • • • • • Cervical mucus and vaginal discharge High vaginal & chlamydia swabs Ectropion Lubrication Pregnancy Post menopausal samples Vault samples Inadequate samples Woman with special requirements Inadequate samples Specimens that are technically inadequate at screening: • Heavily blood stained specimen – insufficient cells seen • Insufficient cells present – possibly due to specimen contamination with lubricant • Insufficient cells present • Mostly endocervical cells (EC) present, insufficient squamous cells • Squamous cells only – insufficient EC cells for follow-up • Squamous cells obscured by polymorphs/debris Specimens that are inadequate due to Paperwork/Technical reasons • Unlabelled vial arrives with form • Vial contains brush head • Specimen leaked insufficient for processing • Sample taken more than 6 weeks prior to receipt in laboratory • No specimen received - Lab will contact sample taker - if sample with clear identifiers found, will screen as usual • Incorrectly labelled vial/partially incorrect identifying information - Lab will give sample taker opportunity to correct identifying information if appropriate Speciments that are inadequate due to Sample Taker id number issues • Sample takers must be aware of the necessity for training evidenced by valid sample taker id numbers and the sample taker must be identifiable on all samples screened. • Sample Taker id number absent - Sample takers will be asked to provide a valid sample taker number. If they are unable to do this, the matter will be referred to the local PCT. • Sample Taker id number not recognised