Drugs
advertisement

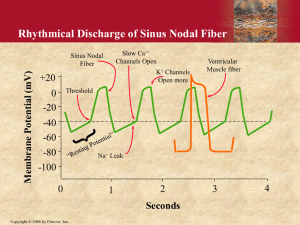
Interpretation And management of the ECG In Bradyarrhythmias And Heart Blocks DR.Tareq M.Al-Muflehi INTERVENTIONAL CARDIOLOGIST . Sinus Bradycardia. . Junctional rhythm. . Idioventricular rhythm. . Sinus node dysfunction or (sick sinus syndrom). . AV-blocks. . Heart block with acute MI. . Intraventricular conduction abnormalities(IVCAs). . MI in the presence of BBB. BLOOD SUPPLY OF THE CARDIAC CONDUCTION SYSTEM The blood supply to the sinoatrial node is from the sinus node artery which arises from the proximal RCA in 55% of the population and in 35% from the circumflex artery and in 10% from both RCA and CX. The AV-node receives its blood supply from the AV- nodal artery which arises from the PDA of RCA in 80% of population and 10% from circumflex artery and 10% from both arteries . Collateral blood supply from the LAD artery makes the AV- node somewhat less prone to ischemic damage than the sinoatrial node . The AV- nodal artery and the first septal perforator of the LAD artery offer dual blood supply to the atrioventricular (His) bundle and RBB . The anterior fascicle of the LBB receives blood from the other septal perforating branchs of the LAD . The posterior fascicle has a dual blood supply from the septal perforating branchs of the LAD and branchs of the PDA of RCA. Cardinal features of normal sinus rhythm . The P wave is upright in leads 1,2,3 and AVF . The P wave is negative in lead AVR . Each P wave is followed by a QRS complex . The heart rate is 60-100 beat\ min NSR Parameters • Rate 60 - 100 bpm • Regularity regular • P waves normal • PR interval 0.12 - 0.20 s • QRS duration 0.04 - 0.12 s Any deviation from above is sinus tachycardia, sinus bradycardia or an arrhythmia Pacemakers of the Heart • SA Node - Dominant pacemaker with an intrinsic rate of 60 - 100 beats/minute. • AV Node(Junctional) - Back-up pacemaker with an intrinsic rate of 40 60 beats/minute. • Ventricular cells - Back-up pacemaker with an intrinsic rate of 20 - 45 bpm. Normal Impulse Conduction Sinoatrial node AV node Bundle of His Bundle Branches Purkinje fibers Impulse Conduction & the ECG Sinoatrial node AV node Bundle of His Bundle Branches Purkinje fibers Sinus bradycardia Normal resting heart rate has been defined as 60-100 bpm. Bradicardia is defined as ventricular rate less than 60 bpm. It should be noted some otherwise healthy individuals have resting heart rate less than 60 bpm. The greatest variation is found in athletes primarily from increase parasympathetic tone. Sinus bradycardia exists when a P wave precedes each QRS complex. this QRS complex is usually narrow (less than 0.120 seconds ) because the impulse originates from a supraventricular focus . There are specific incidences in which, despite the supraventricular focus, the QRS is widened (greater than 0.12 seconds ) an example of this is a BBB (right or left ) in which the QRS is wide but each QRS complex is still considered by a P- wave . Sinus Bradycardia Etiology: SA node is depolarizing slower than normal, impulse is conducted normally (i.e. normal PR and QRS interval). Sinus bradycardia--etiologies Normal aging 15-25% Acute MI, esp. affecting inferior wall Hypothyroidism, infiltrative diseases (sarcoid, amyloid) Hypothermia, hypokalemia SLE, collagen vasc diseases Situational: micturation, coughing Drugs: beta-blockers, digitalis, calcium channel blockers, amiodarone, cimetidine, lithium History: Sinus bradycardia is most often asymptomatic. However, symptoms may include the following: Syncope Dizziness Lightheadedness Chest pain Shortness of breath Pertinent elements of the history include the following: Previous cardiac history (eg, myocardial infarction, congestive heart failure, valvular failure) Medications Toxic exposures Prior illnesses Physical: Cardiac auscultation and palpation of peripheral pulses reveal a slow, regular heart rate. The physical examination is generally nonspecific, although it may reveal the following signs: Decreased level of consciousness Cyanosis Peripheral edema Pulmonary vascular congestion Dyspnea Poor perfusion Syncope Lab Studies: Laboratory studies may be helpful if the cause of the bradycardia is thought to be related to electrolytes, drug, or toxins. Reasonable screening studies, especially if the patient is symptomatic and this is the initial presentation, include the following: Imaging Studies: Electrolytes Glucose Calcium Magnesium Thyroid function tests Toxicologic screen Routine imaging studies are rarely of value in the absence of specific indications. Other Tests: 12-lead ECG may be performed to confirm the diagnosis. Sinus Bradycardia HR< 60 bpm; every QRS narrow, preceded by p wave Can be normal in well-conditioned athletes HR can be<30 bpm in children, young adults during sleep, with up to 2 sec pauses Sinus bradycardia--treatment No treatment if asymptomatic Office: Evaluate medicine regimen—stop all drugs that may cause Bradycardia associated with MI will often resolve as MI is resolving; will not be the sole sxs of MI ER: Atropine if hemodynamic compromise, syncope, chest pain Pacing Junctional rhythm Junctional rhythm is another example of a supraventricular rhythm in which the QRS complex is usually narrow (less than 0.12 seconds ) and regular this is distinguished from sinus bradycardia on ECG because it is not associated with preceding Pwave, a junctional escape rate is usually 40- 60 bpm a junctional rhythm with a rate slower than 40 bpm is termed a junctional bradycardia and a rate faster than 60 bpm is termed an accelerated junctional rhythm or a junctional tachicardia . There are times when there are p waves evident on the ECG of patients who have a junctional rhythm but unlike normal sinus rhythm or sinus bradycardia thes P waves are not conducted in an anterograde fashion these are termed P waves and may appear before during or after the QRS complex depending on when the atrium is captured by the impules emanating from the AV junction As in sinus bradycardia, there are also times in which the QRS is widened because of right or left BBB. Junctional bradycardia Junctional bradycardia is treated in the same way as sinus bradycardia . Junctional bradyardia is a frequent accompaniment of reperfusion and indeed can be used as a marker of successful reperfusion. Therapy of junctional rhythm secondary to sinoatrial node, failure of AV-block is as the treatment of atrioventricular conduction disturbances. Accelerated Junctional Rhythm Etiology Accelerated junctional rhythm is seen in approximately 10% of patiens with MI more than half these patients have inferior MI and about on- third have anterior MI. Digitalis toxicity by itself does not seen to cause accelerated junctional rhythm, as evidence in persons with normal hearts who take accidental overdoses of digoxin. Concomitant heart disease is required to develop accelerated junctional rhythm. other causes of accelerated junctional rhythm are valve surgery, acute rheumatic fever, direct current cardioversion, cardiac cath, COPD, Amyliodosis and uremia with hyperkalemia. The distinguishing characteristic of accelerated junctional rhythm is the atrioventricular dissociation and changing PR interval. . The difference between accelerated Junctional rhythm and third- degree AV- block is the fact that the ventricular rate is faster than the atrial rate in accelerated junctioal rhythm and slower than the atrial rate in third- degree AVblock . Treatment Patients with accelerated junctional rhythm do not usually require therapy for the arrhythmia, although mangement of the underlying cause is indicated. Suppression of accelerated junctional rhythm maybe achieved by increasing the atrial rate with drugs (eg, Atropin, Adrenergics) or pacing. Digoxin - induced accelerated junctional rhythm is an indication to stop digoxin but does not usually require administration of digoxin _ specific fab fragments. Idioventricular rhythm Idioventricular rhythms are regular but unlike sinus bradycardia or junctional rhythm, they are always characterized by a wide QRS complex because their origin lies some where within the ventricles on ECG the rate is usually 20- 40 bpm except for accelerated idioventricular rhythm (rate greater than 40 bpm ). Idioventricular rhythm (IVR) IVR is usually too slow to maintain adequate cardiac output and treatment is more frequently needed. The patient depends on these complexes for survival. Suppressive treatment (e.g. lidocaine) may therefore lead to asystole . Atropine and pacing are usually required, as well as correction of the underlying cause (AMI , complete heart block , cardiac , tamponade , hemorrhage ) . CPR may be needed as well. Accelerated Idioventricular rhythm (AIVR) AIVR is a form of VT and occurs as a rule in patients with cardiac disease ( almost in IHD ). AMI and digitalis toxicity are the common precipitating events. (It is common 48h after MI). This rhythm is also commonly seen when thrombolytics are given for an AMI, and if it occurs, thrombolytics should be continued. (It usually means successful reperfusion). The mechanism is believed to be secondary to an ectopic ventricular focus (usually in the reperfusion zone) that accelerates beyond the intrinsic sinus rate. The P- wave may come closer and closer to the QRS complex at the same time the shape of the QRS complex changes to its wide ventricular contour, and then disappears into it . It is usually regular, has a rate of 60- 120 bpm, and is of little clinical significance. Treatment for AIVR is rarly necessary. With severe symptoms or hemodynamic compromise, Atropine or a trial pacing can be used to stimulate the sinus rhythm to overdrive the ectopic focus. Treatment can also be considerd when AIVR occurs with VT. Suppression of the dysrhythmia can also be undertaken with the same drugs used to treat VT. . Sinus Bradycardia. . Junctional rhythm. . Idioventricular rhythm. . Sinus node dysfunction or (sick sinus syndrom). . AV-blocks. . Heart block with acute MI. . Intraventricular conduction abnormalities(IVCAs). . MI in the presence of BBB. SINUS NODE DYSFUNNCTION OR "SICK SINUS SYNDROME" sick sinus syndrom is a collective term that includes a range of SA node dysfunction that manifests in various different ways on ECG including : . Persistent inappropriate sinus bradycardia . . Intermittent sinus pause/ arrest. . sinoatrial exit block. . AV junctional (escape ) rhythm. . Tachy - brady syndrome. Sick Sinus Syndrome Patients are usually elderly and present with lightheadedness and/or syncope, but it can also manifest as angina, dyspnea, and palpitations. About 50% of people with SSS also display some degree of dysfunction of the AV node Sinus pause and sinus arrest are characterized by the failure of the SA node to form an impulse although sinus pause refers to a brief failure and sinus arrest refers to a more prolonged failure of the SA node, there are no universally accepted definitions to differentiate the two. Because of this, they are often used interchangeably to describe the same cardiac event. On ECG there is an absence of the P-QRS-T complex resulting in a pause of indeterminate length. The sinus node most often resumes pacemaker activity and a normal sinus rhythm is seen. In cases in witch it fails, however the escape rhythm seen is usually from the AV node. If the AV node fails, the next pacemaker to take would result in an idioventricular rhythm. If all of these fail to generate an ascape rhythm, the result is asystole . Mechanism of sinus node dysfunction includes decreased automaticity of sinus nodal tissue and sinatrial (SA) exit block. In SA exit block, rhythmic depolarization continues to occur , but the impulse is delayed or blocked in the perinodal tissue. Diagnosis by surface ECG is difficult because external leads do not directly record activity within the sinus node. Sinus bradycardia associated with sinus node dysfunction is a marked, persistent sinus bradycardia , with sinus rate less than 40 bpm and pauses of greater than 2s. A sinoatrial pause greater than 3s following carotid massage may indicate sick sinus syndrome. Sick Sinus Syndrome Sinus bradycardia (rate of ~43 bpm) with a sinus pause Sinoatrial (SA) blocks result when there is an abnormality between the conduction of the impulse from hearts normal pacemaker (SA node) to the surrounding atrium. AS with AV- block SA block is characterized as first, second and thirddegree, with second- degree blocks subclassified as type I and type II. Tachycardia-Bradycardia Syndrome Common variant of sick sinus syndrome severe bradycardia alternates with paroxysmal tachycardias, most often atrial fibrillation. There is usually a prolonged pause in the cardiac rhythm following cessation of the tachyarrhythmia. Tachycardia-Bradycardia Syndrome Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine, 7th ed., 2005. Abrupt termination of atrial flutter with variable AV block, followed by sinus arrest with a junctional escape beat. Etiologies of Sick Sinus Syndrome More Common Sinus node firbosis Atherosclerosis of the SA artery Congenital heart disease Excessive vagal tone Drugs Less Common Familial SSS (due to mutations in SCN5A) Infiltrative diseases Pericarditis Lyme disease Hypothyroidism Rheumatic fever Sick sinus syndrome--treatment Address and treat cardiac conditions Review med list, TSH Pacemaker for most is required THANK YOU