File - Patty Sponseller, CMD
advertisement

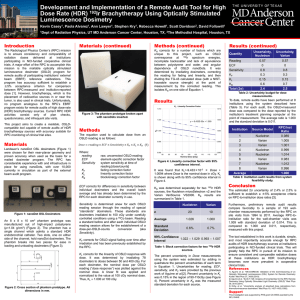
Gynecological Treatment Planning Patty Sponseller, CMD Cervical Cancer Simulation Patient supine Lower extremities immobilized indexed to table Table indexing documented on device Simulation Radiopaque gold seed markers at cervix and distal vaginal DZ. No standard EBRT fields. Block based on 3D imaging Treat AP/PA or 4 field pelvis Patient simulated supine with CT planning. Rectal and vaginal marker Field arrangement depends on body habitus Field Borders Superior = L4/5 Inferior = 3 cm below gold seed most inferior involvement (often at obturator foramen) Lateral = 2 cm lateral to pelvic brim Posterior = Include entire sacrum Anterior = 1 cm anterior to sym pubis AP Pelvis Lateral Pelvis AP/PA DD 4 Field Pelvis Tx inguinal nodes Stage IIIA Increased Lower Border for flash Common iliac nodes involved superior border to L3-4 Increase sup Border about 4cm RT for para-aortic nodes Superior border T12-1 If conformal fields block kidneys Laterally encompass transverse processes IMRT for para-aortics better to spare both kidneys and sm bowel Purple is 50% isoline Doses Doses vary with staging From IA post hysterectomy with Brachytherapy To IIIB-IVA WP (50-54Gy) Brachy boost and Para-aortic LN IMRT (4560 Gy) Midline Block When midline block used If 4 fld pt TX with AP/PA Avoids excess dose to areas adjacent to implant Reduces dose to bladder and rectum After 54Gy boost to 60 Gy Dose What is the dose under the 5% transmission block? Calculate dose here Dose to point under block Primary transmission through the block is only 5% Dose under the block is about 20% of the dose in the open portion Due to the internal scatter from the open field areas Endometrical Cancers Uterine Carcinomas Leimyosarcoma, Endometrial Stromal Sarcomas Adenosarcoma Uterine Sarcoma Simulation Patient supine with lower extremities immobilized Empty rectum and full bladder Whole Pelvis RT Borders Superior = L5-S1 Inferior = below obturator canal and including upper 1/2 -2.3 vagina Lateral = 2 cm lat pelvic brim Posterior = split sacrum to S3 Anterior = pubic symphysis *Consider IMRT with careful target delineation Dose Prescriptions Post-op WP 1.8 Gy 45-50.4 Gy followed with VC (vaginal cuff) boost Pre-op WP 1.8 Gy to 45 Gy with T&O Paraaortic to 45-50 Gy with enlarged unresect LN boost to 60 Gy (IMRT) Ovarian Cancer Simulation Supine, lower extremity immobilization Image entire peritoneal cavity Treat open field AP/PA Borders (historical) sup = above diaphragm Inf = below obturator foramen Lat = outside peritoneum RT primarily reserved for palliative DZ Brachytherapy Teletherapy (linear accelerator RT) is treatment at a distance 100 cm Brachytherapy comes from the Greek word brachy which means short Radiation is placed near to in the tumor High dose of radiation delivered with rapid fall off Radiation used is an Isotope Atoms having nuclei with the same # of protons and different # of neutrons Atom decays giving off radiation Brachytherapy HDR Uses a 10 Curie source of Iriduim 192 HL = 74.22 days Complicated gamma spectrum ave energy .38 MeV high activity Deliver dose in temporary placed catheters, applicators or needles placed in a patient Source embedded in a wire http://www.varian.com/us/oncology/brachytherapy/hdr_brachytherapy.html HDR Treatment Unit Robot Catheter is attached to applicator then to channel on the unit Wire with source goes to preplanned positions in the applicator “dwell positions” to deliver correct amount of radiation Units are made by different vendors Nucletron Applicator placement Placed with or without sedation Depending on type of applicator Patient then imaged on Simulator or CT sim Plan created on TPS Before TX applicator position then verified with conebeam or portal imaging Gynecological cancers 2 basic types of HDR implants Tandem and Ring Miami vaginal cylinder Tandem and Oviods (shielded colpostats) Vaginal Cylinder Deliver dose to the vaginal cuff or vaginal wall Dose is calculated at a distance from the surface of the applicator Not much dose to the rectum or bladder 6 Gy line GOG Definitiion Points A Points B Point B is 5 cm represent medial parametrium/lateral cervix, the approximate point at which the ureter and uterine artery cross. lateral to the center of the pelvis at the same level as point A and approximates the region of the obturator nodes or lateral parametrium http://imaging.ubmmedica.com/cancernetwork/cmhb11/11_20 _Fig_2.gif ICRU report #38 Rectum- 5mm posterior to posterior vaginal wall (as identified by vaginal packing) and bisecting ovoids superiorly and inferiorly Bladder- Posterior most point of a 7cc Foley balloon (with contrast) on lateral film and bisecting on AP film T&R or T&O Dose calculated to Points “A” 2cmsup and lat to the cervical os (vaginal fornices) Point B 3cm lateral to A approx 1/3-1/4 dose to A Calc bladder and rectal doses or DVH Radiopaque packing to minimize dose to bladder and rectum Dwell positons Lateral T & O Bladder and rectal Dose Characteristic Dose Distribution “Pear” shaped dose distribution Middle portion of implant DD from tandem Inferior DD round out to treat cervical fornices Verification Before treatment room survey Verify correct channel to applicator Verify CORRECT catheter length Patient identity by 2 means After delivery first person to enter the room carries the survey meter! Before TX “Dry Run” Before the Ir source leaves the robot housing a dummy source is sent through the applicators This checks for any errors and patency with the catheters and verify positions http://chapter.aapm.org/GLC/media/2011/tollenaar.pdf Verify your activity! A= Aoe-( 0.693t/T1/2 ) t = days since calibration of initial activity T ½ = Half life of isotope Ao = Initial activity A = Activity on you plan Safety when working with Radionuclides Keep time spent as short as possible Increase distance away from the source (not a good idea to use the HDR delivery robot as an arm rest) Shielding- the safest place working around the HDR unit is behind the source! Reportable Errors and Medical Events Wrong dose of more than 10% with a radioactive source Wrong patient Wrong source Leaking source or non-removed source National Regulatory Commission (NRC) or Agreement State NRC sub-division of Dept of Energy Regulates radioactive material and establishes reporting procedures NRC and state agree to transfer authority of radioactive materials to the state called and “agreement state” NRC then regulates only federal facilities State regulates PET scanners, Linacs, and naturally producing and cyclotron produced radionuclides States that are not agreement states Montana, Idaho, Wyoming, South Dakota, Missouri, West Virginia, Virginia, Pennsylvania, Delaware, New Jersey, Rhode Island, Vermont, Michigan, Indiana, District of Columbia, Alaska, Hawaii Indiana Incident http://chapter.aapm.org/GLC/media/2 011/tollenaar.pdf