The Other CRRT-PD - Pediatric Continuous Renal Replacement
advertisement

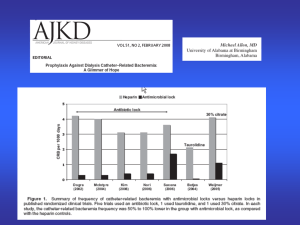
The Other CRRT: Peritoneal Dialysis Mignon McCulloch Associate Professor Paediatric Nephrology/Critical Care Acknowledgements Thanks to Stuart and Tim Including all forms of CRRT Disclosures Passionate about PD Access for children with AKI in poorly resourced areas London Evelina Children’s Hospital London UK Evelina Children’s Hospital Andrew Durward Personal Communication PICU 8818 Admissions 413 deaths Mortality 4.7% 20 Beds Staffing: 7 Consultants 20 Fellows 150 Nurses Training in nurses: CVVH 30% trained PD in 100% nurses Evelina Children’s Hospital PICU 2002 – 2009 Nos of Cases CVVH PD 119 188 139 Cardiac Age in months 30 7.8 Med 0.22 Weight in kg -- 5.3 Med 3.3 Mortality 30% 17% Red Cross Children’s Hospital Cape Town SA Red Cross Children’s Hospital(RXH) University of Cape Town Experience Increasing incidence in association with multiorgan failure in paediatric ICU’s 1 200 – 1 400 admissions per year Acute medical cases Cardiac cases Burns Head injuries Other Mortality 8% Dialysis 3.5% AKI ??? 600/yr 250/yr 50/yr 50/yr Rest Causes of Acute Renal Failure Sepsis 46(22%) Post-cardiac surgery 36(17%) Undiagnosed chronic renal disease Gastroenteritis 21(10%) Haemolytic uraemic syndrome 19(9%) Necrotizing enterocolitis 15(7%) 19(9%) Causes of Acute Renal Failure Leukaemia/Lymphoma 14(6%) Myocarditis 11(5%) Rapidly progressive nephritis 10(5%) Trauma/Burns 8(4%) Toxin ingestion 7(3%) Kwashiorkor** 6(3%) Practicalities of PD Quick – really quick – 20 mins K+ 9! Bed-side insertion by Paeds Nephrologist/Intensivist/Surgeons (Surgeons as backup) Cook/Peel Away Tenckhoff/Formal Tenckhoff Empty Bladder Sedation + Local Anaesthetic Practicalities of PD Prescription Dialysis fluid Dianeal(Lactate buffered) or Bicarb based Cycles 10-20ml/kg increase as tolerated 10/30-90/20mins Manual or Cycling Home choice > 3kg Adapted to ventilatory requirements Manual Dialysis with Fluid Warmer Perit Dial Int 2001 Flynn et al (Brophy & Bunchman) Time period Nos of patients Complication Rate Commonest problem Survival RXH Flynn (USA) 2 yrs 10 yrs 68 63 25% 25% Catheter blockage 61% Catheter malfunction 51% Acute Peritoneal Dialysis January 1999 to January 2004 TOTAL NUMBER OF PATIENTS Male: Female Age at dialysis: < 3 months 3 months - 1yr 1 – 6 years 6 – 12 years > 12 years 212 102:110 79(38%) 45(21%) 38(18%) 30(14%) 20(9%) Acute PD Long term outcome Survival following Acute PD 130(61% ) Chronic PD required following Acute PD 26(12%) Total nos of patients requiring CVVHD (PD not possible) 20(9%) Survival following CVVHD 11(55%) Peritoneal Dialysis as a Form of CRRT for Infants in a Developing Country McCulloch M, Argent A. Red Cross Children’s Hospital University of Cape Town Specific Paeds Management Issues Very Low Birth Weight Infants Koralkar R et al. Ped Research 2011;69:4:354-8 AKI reduces survival in infants <1500g Very low glomerular filtration rate Independent risk factor Mild exposure – high degree of injury High rates of infection Nephrotoxic drugs Premature infants <1000g Increase SCr of 1.0mg/dL(88.5umol/l) Doubles the odds of death Small infants < 5kg 25 of these patients were < 5kg 15/25 Infants (60%) survived Age range from 2 - 138 days Male:Female 2:1 Diagnosis of Infants Surviving Dialysis INFECTIVE CAUSES Septicaemia Diarrhoea Fungal sepsis SURGICAL CAUSES Necrotising Enterocolitis Cardiac Surgery - TGA’s Abdominal Surgery DRUGS 13/15 patients received large doses of Furosemide e.g. 5mg/kg/dose pre-dialysis 10/13 patients were on Dopamine infusions at time of dialysis 2 patients received Adrenaline infusions in addition 7/14 patients were on an Aminoglycoside antibiotic (amikacin/gentamicin) pre - dialysis Weight of Infants surviving Dialysis 7 6 5 4 3 2 1 0 <1kg 1-2kg 2-3kg 3-4kg 4-5kg Advantages of Acute PD Catheters No bleeding complications 2/15 catheters blocked - day 3 & 4 on dialysis Replaced 1 catheter by “re-wiring” Duration Of Dialysis 120-144hrs 96-120hrs 72-96hrs 48-72hrs 24-48hrs 0-24hrs 0 1 2 3 4 OUTCOME 15/25(60%) Infants survived to come off dialysis Nil required long term dialysis 3 Subsequently demised - not related to dialysis: 1 Accidental extubation 1 Cerebral Palsy and developed septicaemia 1 year later 1 Shock & Dehydration due to excessive colostomy losses 3 months later Acute PD in PICU 1999-2009 Presented IPNA Aug 2010 New York Red Cross Children’s Hospital, Cape Town SA Total 406 cases/10years Wt range 900g – 70kg Age 1 day – 16yrs Diphtheria – Liver Transplant PD IN PICU Total Nos Neonates(<1mth) Infants(<1yr) Cardiac 406 85(21%) 221(54%) 95(23%) Overall Mortality Rate 70 60 50 30 Overall 42% 20 2009 2008 2007 2006 2005 2004 2003 2002 0 2001 10 2000 Rate % 40 Specific Mortality Rate 2009 2008 2007 2006 2005 2004 2003 2002 2001 Neonatal 53% Infant 53% Overall 42% 2000 80 70 60 50 40 30 20 10 0 Peritoneal Dialysis in neonates with inborn errors of metabolism: Is it really out of date? Neonatal Inborn Error of Metabolism If response to dietary and pharmacologic treatment poor or severe hyperammonemic coma Require rapid removal of neurotoxic metabolites Risk: Ammonia > 1355ug/dl(800umol/l) – 34% survival rate Coma > 2 - 3days Enns et al NEJM 2007 256:2282-92 Msall et al. N Eng J Med 310:1500-5 Extra-corporeal dialysis more effective >> PD Outcome primarily related to duration of neonatal hyperammonemic coma PD in IOM Ped Nephrol(2008) 23:163-8 7 Neonates ammonia > 1000ug/dL(588umol/l) Bed-side surgically inserted PD catheter No difficulties – mild leakage in 2 patients Baxter closed system 1.36% lactate buffered Added K+ and Antibiotics Fill volumes – 10-15ml/kg incr to 30ml/kg Dwell times 30-45mins PD in IOM Ped Nephrol(2008) 23:163-8 4 organic aciduria pts ammonia < 200umol/l 1 propionic aciduria ammonia < 362umol/l Average after 20hrs of PD + medical rx Catheter out day 5 – sepsis day 19 - death Mean time coma 14.5hrs 4/7 Survivors – 3 normal outcome + 1 delay Death 3/7 1 OTC – death after few hrs on dialysis 1 Sepsis after recovery of acute metabolic decompensation 1 survived acute neonatal hyperammonia PD in IOM Ped Nephrol(2008) 23:163-8 CVVH/D Vascular access – difficult in neonates Anti-coagulation PD maintains some effectiveness Applied in ALL neonatal units Less efficacious than extra-corporeal dialysis But can improve prognosis Rapid access – bridging procedure Small patient size Less severe hyperammonemia Quick and Easy Continuous Flow Peritoneal Dialysis Clin J Am Soc Nephrol. 2011 Feb;6(2):311-8 PD useful in hypotension, disturbed coagulation or difficult venous access Disadvantage – limited efficacy CFPD – 2 bed-side catheters + adapted CVVHF machine CFPD vs Conventional PD for 8-16 hours First report of CFPD in Paeds practice Clearances and UF significantly higher than PD Continuous Flow Peritoneal Dialysis Clin J Am Soc Nephrol. 2011 Feb;6(2):311-8 Mean UF Creatinine clearance PD 0.20ml/min/1.73m2 vs CFPD 1.8ml/min/1.73m2 PD 7.6ml/1.73m2 vs 28.8ml/1.73m2 2 Catheters vs Double lumen catheters Urea clearances 44-58ml/min(2xC) vs 14-20(DL) DL not available in paeds Continuous Flow Peritoneal Dialysis Clin J Am Soc Nephrol. 2011 Feb;6(2):311-8 Complications Catheter related – major complication rate <2% Pederson KR KI Supp 108:S81-86, 2008 Infection – closed system Intra-abdominal pressure – carefully monitored Clearances + UF Lower values than predicted adults: Low flow rate 100ml/1.73m2/min Re-circulation due to small patient Continuous Flow Peritoneal Dialysis Clin J Am Soc Nephrol. 2011 Feb;6(2):311-8 CFPD useful for ARF Ronco C Perit Dial Int 27:251-3, 2007 Especially in children Especially if small haemodynamically infant Developing and Developed countries Future Larger studies in Paeds Higher flow volumes Improved catheter technology Acute Kidney Injury:The Future is now The past of acute kidney injury was observation, and the present is intervention with renal replacement therapy, but perhaps the future is the use of biomarkers to identify AKI sooner and intervene early. Bunchman TE. Oct 2009. Nephrology Times 15-16. Thank you for your attention !