Cardiovascular Disease in OB - UC San Diego Health Sciences
advertisement
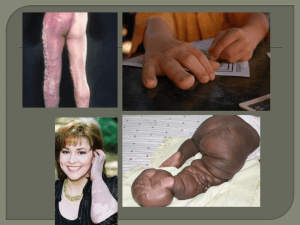
Cardiovascular disease in obstetrics Tom Archer, MD, MBA UCSD Anesthesia Heart Disease in Pregnancy (Developed World) • Less post-streptococcal rheumatic valve disease (MS, AS). • More repaired congenital heart disease. Maternal Outcome • Correlates with NYHA functional class. • How much can the patient do before she gets symptoms? • Let’s hear it for the history! Risk factors for maternal cardiac events • • • • • Poor NYHA class Cyanosis Myocardial dysfunction Prior arrhythmia Prior heart failure/stroke. Siu SC Circulation 2001;104;515-521 CV in pregnancy– Big Picture • Increase O2 demand Increased CO • Stable BP with increased CO means decreased SVR. • Slight increase in HR CV in pregnancy– Big Picture • Pregnancy will make stenotic lesions more symptomatic. • Patient may need interventional procedure (valvuloplasty) or termination of pregnancy. Pulmonary capillaries LV dilation / hypertrophy Tricuspid Aortic stenosis Pulmonic Mitral Aortic stenosis at rest Cardiac output not sufficient to cause critically high LV intracavitary pressure / LV failure. Resistance arterioles Pulmonary capillaries (edema) LV failure / ischemia Tricuspid Aortic Stenosis Pulmonic Mitral Aortic stenosis with increased cardiac output / arteriolar vasodilation: Decreased SVR Fall in systemic BP and / or increase in LV intracavitary pressure ischemia or LV failure. Resistance arterioles– decreased SVR CV in pregnancy– Big Picture • AI and MR are often well tolerated in pregnancy. Decreased SVR helps forward flow. Repaired Congenital Heart Disease Patients with no sx. SBE prophylaxis (amp/gent, vanco/gent) ?1% incidence of CHD in infant alert pediatrics Otherwise, “good to go” Small ASD, VSD or PDA • No IV bubbles (LR shunt can reverse). • Epidural LOR with saline, not air • Pain increased SVR increased LR shunt ?RV failure? • Slow onset epidural preferred. Avoid sudden drop in SVR which could cause RL shunt and maternal hypoxia. Small ASD, VSD or PDA • Memorize (and avoid) causes of pulmonary artery vasoconstriction: – Alveolar hypoxia – Hypothemia – Hypercarbia – Acidosis – Pain Increased PA pressure can convert LR shunt into RL. 30-50% of congenital heart patients will have an ASD as part of their disease complex. home.cc.umanitoba.ca/~soninr/PS.ht ml www.med.yale.edu/.../cardio/chd/e_a sd/index.html Coarctation of aorta • Uncorrected, is a very dangerous lesion in pregnancy. • Increased afterload for heart, decreased perfusion for uterus. • Risks: LV failure, aortic rupture, endoaortitis. • More common in males. www.mayoclinic.org/coarctation- Dilated collaterals in coarctation www-clinpharm.medschl.cam.ac.uk/.../index.html Descending thoracic aortic coarctation repaired with stent www.med.yale.edu/.../c_coarct_1815204/index.html Tetralogy of Fallot http://www.nhlbi.nih.gov/health/dci/Diseases/tof/tof_what.html Marcus JT Dong SJ. Smith ER. Tyberg JV. Changes in the radius of curvature of the ventricular septum at end diastole during pulmonary arterial and aortic constrictions in the dog. [Journal Article] Circulation. 86(4):1280-90, 1992 Oct. Tetralogy of Fallot • Patients with corrected TOF should have periodic echocardiograms. • Corrected TOF probably “good to go.” May have conduction abnormalities. • Uncorrected TOF needs careful hemodynamic management b/o potential shunts R > L or L > R. Uncorrected Tetralogy of Fallot • Two needs: – Maintain SVR to avoid increasing RL shunt. – Maintain RV filling pressure to maintain pulmonary perfusion (LUD and fluid boluses). Patent Ductus Arteriosus • Common in premature babies with increased pulmonary vascular resistance. • Can lead to cyanosis (RL shunt) or CHF (LR shunt). • RL shunt will cause cyanosis in LEs, with higher SpO2 in R arm. • Oximeter or arterial line on feet will pick up RL shunt and accidental ligation of the aorta. • Hoarseness can be d/t damage to recurrent laryngeal nerve at aortic arch. http://health.yahoo.com/media/mayoclinic/images/image_popup/r7_patentd uctus.jpg With PDA shunt can be RL or LR, depending on the pulmonary resistance. Shunt can be RL after birth, then reverse to LR as pulmonary resistance falls, then become RL again as Eisenmenger’s syndrome develops (long term pulmonary hypertension). www.rjmatthewsmd.com/Definitions/pop/22fig.htm Eisenmenger’s Syndrome • Increased pulmonary flow (LR shunt due to ASD, VSD or PDA) causes hypertrophy of pulmonary arteries pulmonary hypertension reversal of shunt to RL with cyanosis. • Need to correct LR shunt BEFORE it reverses. • Need to correct LR shunt despite normal ABGs. Eisenmenger’s syndrome with pulmonary artery hypertrophy. Patient is thin, cyanotic and may have clubbing. www.radiofreeithaca.net/search/Hippocrates www.rjmatthewsmd.com/Definitions/po p/23jfig.htm tchin.org/portraits/angela-1.htm Pulmonary Hypertension (PH) • What’s the difference from Eisenmenger’s Syndrome? • Eisenmenger’s Syndrome has increased PVR (hypertrophic changes, incresaed muscularity) plus a RL hole in the heart (ASD, VSD or PDA). PH, Eisenmenger’s Syndrome, AS, MS and Coarctation of Aorta • Keep SVR up to avoid inc in CO and / or dec BP • Keep SVR up to avoid inc RL shunt Pulmonary hypertension— What causes it? Exactly how does it kill patients? What is the flow-limiting resistance in the entire circulation? • Normally it is NOT the pulmonary circulation or any of the heart valves. • Normally it is the systemic resistance arterioles (<0.1 mm in diameter) Pulmonary vascular resistance in normal lung • Normally, increased CO causes decreased Pulmonary Vascular Resistance via recruitment and distention of pulmonary capillaries. • Normally, PA pressure stays the same despite increased CO. Passive Influences on PVR: Capillary Recruitment and Distension http://www.lib.mcg.edu/edu/eshuphysio/program/section4/4ch4/s4ch4_19.htm http://www.pathguy.com/lectures/hipbp.gif Pulmonary hypertension • Acute pulmonary thromboembolism Pulmonary hypertension • Chronic pulmonary thromboembolism Pulmonary hypertension develops when pulmonary arteries develop abnormal resistance • When pulmonary vessels become high resistance (fibrosis, muscular hypertrophy) they can NOT dilate or recruit and PA pressure rises with increased CO. How does pulmonary hypertension kill patients? • By causing the interventricular septum to bow into the LV cavity, diminishing its capacity. • Cardiac output falls, BP falls, patient dies. How do we keep PH from killing patients? • Keep Pulmonary Vascular Resistance down. • Keep Systemic Vascular Resistance up. • Prevent increases in CO. • This same logic applies to any stenotic cardiac lesion, such as AS! Pulmonary hypertension • PA catheter for actual measurement of PA pressure and titration of pulmonary vasodilators. In MS, HOCM and AS • Keep HR down • “Slow and tight” for stenotic CV lesions. Pulmonary Hypertension • Specific drug Rx: – Inhaled O2 – Inhaled NO – IV, SQ, inhaled, oral: Epoprostenol = prostacyclin = Flo-Lan – Endothelin antagonist: Bosentan (Tracleer) – Oral sildenafil (Viagra). PH and Esiensmenger’s • High alveolar PAO2. • Avoid: pain, hypercarbia, hypothermia, acidosis • Maintain adequate SVR to avoid need to inc CO. Use phenylephrine, not ephedrine. RL shunts • Cyanosis not corrected by increased FIO2. • Watch out for IV bubbles brain or heart infarction. • Keep systemic vascular resistance up to avoid increased RL shunt. • Avoid infant crying and other things (alveolar hypoxia, hypothermia, acidosis, hypercarbia) which increase pulmonary vascular resistance. Compensated patient with POTENTIAL RL shunt. LA LV High SVR, Ao Minimal RL shunt PA RA RV Low pulmonary vascular resistance Normal, compensated patient with ASD, VSD or PDA-- high SVR and low pulmonary vascular resistance minimal RL shunt. Decompensated patient with REAL RL shunt. LA LV Decreased SVR desaturation Ao PA RA RV Increased pulmonary vascular resistance desaturation Decompensated patient with ASD, VSD or PDA-- Decreased SVR or increased pulmonary vascular resistance increased RL shunt and increased arterial desaturation. What lowers SVR? • Exercise • Spinal or epidural anesthesia. • Vasodilating anesthetics (sevoflurane, isoflurane, desflurane) • Sodium nitroprusside • Hydralazine • Oxytocin • Fever • Squatting RAISES SVR (Tetralogy of Fallot). Bolus CS. oxytocin Epidural (10 U in this example) dramatically lowers SVR and CO Repeat anesthesia. Delivery with usually increases. CO can increase because volume status is inc inadequate, HR and CO, oxytocin bolus with decrease aortocaval compression has been relieved, and oxytocin, by the uterus, causes autotransfusion. SVRcontracting and BP, increase in CO and SV. Ensemble of hemodynamic effects of oxytocin in 15 patients at C-section: Decrease in SVR Increase in CO: Anesthesiology 2008; 108:802–11 Copyright © 2008, the American Society of Anesthesiologists, Inc. Lippincott Williams & Wilkins, Inc. Hemodynamic Changes Associated with Spinal Anesthesia for Cesarean Delivery in Severe Preeclampsia Robert A. Dyer, F.C.A. (S.A.),* Jenna L. Piercy, F.C.A. (S.A.),† Anthony R. Reed, F.R.C.A.,† Carl J. Lombard, Ph.D.,‡ What raises pulmonary vascular resistance? • • • • • Alveolar hypoxia Acidosis Hypothermia Crying Pain (catecholamines) LR shunts • Volume overload to LV. Can cause CHF. • Can manage with reduction in systemic vascular resistance (vasodilating anesthetics). • Over time LR shunt can lead to Eisenmenger’s syndrome