Nasal Polyps
advertisement

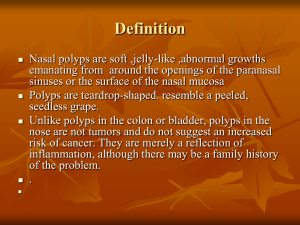
Nasal Polyps - Pathogenesis and Treatment Implications Bastaninejad, Shahin, MD, Assistant Professor of ORL-HNS, TUMS, A m i r ’ A l a m Hospital Importance NPs have been shown to have a significant detrimental effect on the quality of life, which is similar in severity to COPD Introduction • Nasal polyps appear as grape-like structures in the upper nasal cavity, originating from within the ostiomeatal complex • They consist of: loose connective tissue, oedema, inflammatory cells and some glands and capillaries, and are covered with varying types of epithelium, mostly respiratory pseudostratified columnar epithelium… • Eosinophils are the most common inflammatory cells in nasal polyps (80%), but Neutrophils, mast cells, plasma cells, lymphocytes and monocytes are also present, as well as fibroblasts • IL-5 is the predominant cytokine in nasal polyposis, reflecting activation and prolonged survival of eosinophils • In the general population, the prevalence of nasal polyps is 4% (2.2/1 MF Ratio) • The average age of onset is approximately 42 years • In patients with asthma, a prevalence of 7 to 15% has been noted whereas, in NSAID sensitivity, nasal polyps are found in 36 to 96% of patients Factors associated with NP • Allergy Only Kern state inhalant allergy as a risk factor for NP, but food allergy is significantly higher in NP patients (80%) • Asthma NPs are present in 13% in non-atopic asthma (skin prick test and total and specific IgE negative) and 5% in atopic asthma • Aspirin sensitivity In patients with aspirin sensitivity 36-96% have nasal polyps Factors associated with NP • Genetics NP are frequently found to run in families… HLA-A74 , HLA-DR7 • Environmental factors The role of environmental factors in the development of NP is Unclear Hypotheses regarding the underlying mechanisms • Chronic infection (Fungal/Bacterial) • Aspirin intolerance (Samter) • Aerodynamics alteration with trapping of polutions • Epithelial cell defects / Epithelial disruptions • Gene deletions (CFTR genes in CF) • Inhalant or food allergens (discussed in previous page) Chronic rhinosinusitis with and without nasal polyps Chronic Rhinosinusitis Nasal Polyps 20-33% of CRS The spectrum of sinus disease Nasal Polyps Rhinosinusitis PMN TH1 (INF-gama, IL-8) EOS TH17 TH2 (IL-4, IL-5) Histopathology • Frequent epithelial damage, a thickened basement membrane, and Edematous to sometimes fibrotic stromal tissue, with a reduced number of vessels and glands but virtually no neural structure • Among the inflammatory cells, Eosinophils are a prominent and characteristic feature in about 80% of polyps H&E staining . Immunoperoxidase staining Pathomechanism • Eosinophilic inflammation – IL-5 was found to be significantly increased in nasal polyps – Cytokine IL-5 Eos ECP (E. cationic protein) progression in pathology Pathomechanism • Extracellular matrix regulation – Eos TGF-β1&2 Fibroblast activity progression in pathology (increase in extra cellular matrix formation) Pathomechanism • Role of Staphylococcus aureus enterotoxins (SAE) – Multiclonal IgE antibody formation to SAE can be seen in nasal polyp tissue, but rarely in CRS – It is positive in about 30-50% of the patients with NP and in about 60-80% of nasal polyp subjects with asthma Nasal polyposis: aetiology and pathogenesis Epithelial damage (barrier dysfunction) chronic microbial trigger B T Hyper IgE Cytokines Polyclonal IgE Albumin Superantigens S. Aureus enterotoxins: disease modifiers Eosinophils ( apoptosis) IL-5 Chemokines Eotaxin ECP Demo for Pathogenesis polyps Mast cell eosinophil Arachydonic acid Cycloxygenase Prostaglandin 5 lipoxygenase Leukotrienes Histamine Interleukin Thanks from Dr. R. Cathcart for this demo cytokines B cell Differentials • • • • • • • • • • • • Encephalocoeles Gliomas Dermoid tumours Haemangiomas Papillomas / transitional cell papillomas Nasopharyngeal angiofibromas Rhabdomyosarcomas Lymphomas Neuroblastomas Sarcomas Chordomas Nasopharyngeal carcinomas Medical Treatments • Corticosteroids – reduce airway eosinophil infiltration by preventing their increased viability and activation • Directily • Or via reducing the secretion of chemotactic cytokines by nasal mucosa and polyp epithelial cells – Topical Cort.: effect on poly size and also on symptoms associated with NP such as nasal blockage, secretion and sneezing but the effect on the sense of smell is not high • Postoperative treatment with topical corticoidsteriods – Postoperative effect on recurrence rate of NP after polypectomy with intranasal steroids is well documented and the evidence level is Ib – But in patients who undergone FESS operation did not show a positive effect of local corticostoroids over placebo (3mo-1yr2yr) • Systemic steroids : – Is effective in polyp reduction and nasal symptoms associated with NP, even on sense of smell – Oral corticosteroids for 10 days (20-40mg) there are reports with 21 days and also higher doses (up to 50mg) of prednisolone – The benefit of oral steroids, however, remains less definitive with little randomized data available and the risk of systemic effect from oral steroids use in severe cases • Antibiotics: – There is also increasing evidence in vitro of the anti-inflammatory effects of macrolides – The exact mechanism of action is not known, but it probably involves down regulation of the local host immune response as well as a downgrading of the virulence of the colonizing bacteria • Regimens (12wk also you can try 6wk): – Erythromycin Ethylsuccinate: 400 q6h up to 2wk, then 400 q12h up to 10wk – Clarithromycin: 500 q12h up to 2wk, then 500 daily up to 10wk – AZM 2011 lack of efficacy in treatment of CRS with or without NP • Antihistamines: – Cetirizine in a dose of 20 mg/day for three months, significantly reduced sneezing, rhinorrhoea and obstruction compared to placebo but with no effect on polyp size – So it is recommended in allergic patients with NP • Antileukotrienes: – There are a few case controlled trials indicate that antileukotriene beneficial effect on treatment nasal may have symptoms in patients with chronic/persistent rhinosinusitis and nasal polyposis • Capsaicin: – It is a neurotoxin that depletes substance P with some other neurokinins and neuropeptides, leading to long-lasting damage to unmyelinated axons – Tested in Eosinophilic non allergic non asthmatic NP – capsaicin significantly increased NSAV (nosesinuses air volume) and very significantly improved subjective and endoscopy scores, but did not significantly alter ECP • Method of Capsaicin delivery: – for 3 consecutive days patients received: 0.5 ml 30 mmol/L capsaicin solution sprayed into each nostril, and 100 mmol/L of capsaicin solution on days 4 and 5, respectively • Furosemide: – It exhibited an anti-inflammatory effect – Also it acts on Na/Cl transporter and reduce tissue edema, too – Passali (2003) RCT-n=177, post polypectomy furosemide vs. placebo vs. mometasone. Results after 5yr F/U: 17% recurrence with furosemide 30% recurrence with placebo 24% recurrence with mometasone • Method of furosemide delivery: – Furosemide diluted in physiological solution (2 ml of furosemide in 2 ml of saline) administered as nasal puffs (2 puffs per nostril a day, each puff corresponding to 50 micg) for 30 days. – Frist 2yrs: every other mounth (12/24mo) – Next 2yrs: 1mo on, 2mo off (8/24mo) – In 5th yr: 2mo in a year (2/12mo) Strength of evidence for treatment of CRS vs. NP Intervention Corticosteroids Chronic rhinosinusitis Topical Systemic Antibiotics Oral short term < 2w Oral long term (12w) Antimycotics Topical / Systemic Antihistamines Anti-leukotrienes Nasal saline douche Decongestants Allergen avoidance Nasal polyps A / A C C C D C D D / C D D D B C D D D Guideline in our country • INCS for undisclosed time ? • Macrolide administration for 6 to 12wks • Oral corticosteroids for 10-20 days (20-40mg) • Montelukast (10mg/day) • In allergic patients: Cetrizine 20mg/day for 3mo Scheme for experimental polyp treatment polyps Mast cell eosinophil 2 Arachydonic acid Cycloxygenase Prostaglandin cytokines 5 lipoxygenase 3 1 Leukotrienes Histamine 4 B cell Interleukin 5 Future therapies in nasal polyposis Anti-CCR3? Anti-IgE? Eotaxin Tacrolimus? IgE Anti-IL-5? Corticosteroids? Antibiotics? IL-5 Anti-LTs? ECP Anti-fungal? Surgical Treatments • Surgical treatments, including Polypectomy alone or in combination with FESS, rarely result in long term control of polyposis and are typically combined with medical treatment • When hyposmia is the primary symptom, no additional benefit seems to be gained from surgical treatment. If nasal obstruction is the main problem after steroid txy, surgical treatment is indicated • When to proceed with surgical therapy? – when medical therapy fails to control symptoms – when the patient is not suitable for oral steroids – when total nasal obstruction occurs – when there complications is persistent infection or • Simple polypectomy vs. FESS!? Dalziel (2003) - meta-analysis : FESS Simple Symptom improvement Recurrence 78-88% 43-84% 28% 35% 7% difference!! • When is it logical to perform FESS instead of a simple polypectomy operation? – Severe and extensive disease – Underlying diseases (Asthma, Samter, Allergic fungal, CF,…) – Revision cases when pathology is not localized Bastaninejad MD