Primary spine tumors
advertisement
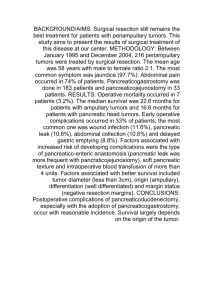
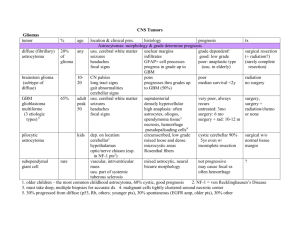
Primary Spinal Tumors (Soft tissue tumors) H. Louis Harkey Department of Neurosurgery University of Mississippi Jackson, MS Anatomical Classification of Spinal Cord Tumors • Extradural : Benign and malignant verteberal tumors, tumors near the spinal cord. • Intradural tumors – Extramedullary: nerve sheath and menengial – Intramedullary: glial and other Meningioma • Slow growing benign masses producing indolent symptoms • ~15% of all meningiomas are spinal • 5:1 female to male ratio • Typically intradural extramedullary but can be extadural • Most commonly thoracic in location, Cervical second most common Meningioma • Clinical presentation is indistinguishable from any other slow growing intraspinal mass • Deficits are often dramatically reversible • Treatment is resection by safest route • Total resection including dural attachment and/or cauterization of the adjacent dura = 1% recurrence rate • Subtotal resection has much higher risk of recurrence Schwannoma • Account for ~25% of intradural & ~50% of intradural, extramedullary tumors • 70% intradural, 15% dumbbell, 5% extradural • 0.3-0.4 cases/100,000 per year • Typically present in 4th and 5th decade • No male-female predilection • Present with radicular pain, weakness in lumbar tumors, long tract motor signs & urinary retention in cervical & thoracic Schwannoma • Benign tumors • Arise from Schwann cells of the sensory rootlets • Tumor only contains Schwann cells and causes symptoms by compressing neural elements • Can be removed via hemilaminectomy in most cases • Total resection is curative • Residual tumor should be followed long term • Long tract signs typically improve after resection Fewer Antoni B cells Neurofibroma & Neurofibromatosis • Commonly seen in NF-1 • Occur more frequently in the cervical spine in NF-1 • May be intradural, extradural or dumbell • Often multiple • Sometimes plexiform Neurofibroma • Benign • Fusiform expansion of the nerve (Schwann, perineural and neural cells) • Difficult to get complete resection because of the extra-foramenal extension and risk of functional loss Ganglioneuroma • Pathology – Ganglioneuroma (extradural, dumbbell) – Gangliocytoma – Ganglioglioma (intraduralintramedullary) • Most are benign though Gangliogliomas may become malignant • More often seen in patients < 30 • Male:female 3:2 Ganglioglioma • 10% of gangliogliomas are spinal, rest cranial • Most are paraspinal, may extend into canal • Arise from sympathetic NS • Rarely intramedullary • IM tumors do not have a plane T2 Contrast Ependymoma • Seen in adults, 15 to 40 • Male = Female • Presenting signs depend on location • Longer duration, more severe symptoms = less favorable functional outcome with surgery • Arise from ependymal lining of the central canal & from filum terminale • Sometimes associated with a syrinx Ependymoma • Arise from ependymal lining of the central canal, • Filum origin usually myxopapillary type • Very rarely malignant • Total resection is possible in the majority of tumors • The goal of surgery is complete resection with good functional outcome • Functional improvement common after resection • Progression free survival similar for total resection vs partial resection + RT Perivascular pseudorosettes Astrocytoma • Occur at any age, average age of dx is 35 to 40 • Accompanying syrinx in 40% • Occurs equally throughout cord • Presenting sign depend upon location Astrocytoma • Most are grade I or II • Complete surgical resection is impossible • RT recommended after dx • Outcomes similar for biopsy + RT and resection + RT • Low grade recurrent tumor can be treated with reresection Hemangioblastoma • Highly vascular tumors comprising 2% of spinal cord tumors • ¼ associated with von Hippel-Lindau, ¾ sporadic • 10 times less common than intracranial • Male predominance • Presents mid life Hemangioblastoma • Usually dorsal • Treatment is surgical resection • Sometimes multiple • Take feeding artery before draining vein • Grade I neoplasm • Differential renal cell CA (common in VHL) Cavernous Angioma • Vascular malformation • M = F, Female more likely to hemorrhage • More likely to present in 3rd & 4th decade Cavernous Angioma • Often dorsally located and comes to surface • Hemosiderin stained • Resection with second hemorrhage or progressive deficit • Thin walled abnormal vascular channels Lipoma • Typically associated with spinal dysrahpism • Presents like any space occupying lesion with progressive myelopathy • Onset of symptoms often associated with weight gain Lipoma • Treatment is surgical with debulking of the tumor and duraplasty • Must take care not to injure normal spinal cord.