Treatment rectovaginal endometriosis
advertisement

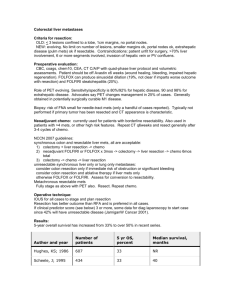
681445250 1 Preferred Treatment for Rectovaginal Endometriosis: Surgery versus Medical Therapy K.-W. Schweppe Frauenklinik Ammerland, Teaching Hospital of the University of Gצttingen, Westerstede, Germany Deep infiltrating, retroperitoneale endometriosis is considered as a special entity of endometriosis with respect to the histological characteristics. The nodules are containing glands, stroma,and muscle cells resembling adenomyotic foci (1,2). For the clinician the question is of importance, whether this endometriotic nodules react to hormonal therapy or surgery is the only option of choice as known from adenomyosis of the uterus. Material and Methods We performed a retrospective analysis of 78 cases treated in our clinic between 1988 and 1998 for rectovaginal endometriosis, of which we have follow up data between two and thirteen years, with a mean follow up period of 5,2 years. Four different treatment options were performed: 1.) Medical treatment with Danazol or GnRH-agonists for 6 months; 2.) permanent medical therapy i.e. low dose progestins or GnRH-agonists with add back medication -continuously or intermittent (3), 3.) primary surgical treatment, i.e. resection of the nodule with disc resection of the rectum, or rectum resection with anastomosis (4), and 4.) preoperative medical therapy with GnRH-agonists for reduction of the implants and the blood supply for 3 to 6 months followed by surgery. Results 24 patients were treated medically (8 with Danazol 600 mg/d and 16 with GnRH-agonists for 6 months); 22 reported reduction of symptoms and improvement of their quality of life despite of different side effects. But all claimed recurrence of the disease within 3 to 12 months after cessation of therapy. Of these group 16 were than put on GnRH-agonists with add back medication for permanent medical treatment; all responded again. Two were lost of follow up, two relapsed and had surgery but 14 are still on this therapy. Primary surgical treatment were performed in 19 cases and in the 6 women with recurrence after medical therapy. Resection of the tumor was sufficient in 4 cases, disc resection of the rectum was necessary in 9 cases and resection of the bowl with anastomosis was done in the remaining 12 patients. During the follow up period we observed 7 recurrences (2 after resection of the nodule, 3 after resection of the anterior wall of the bowl, and 2 after resection and anastomosis of the rectum). The last group of preoperative medication contains 35 patients; 6 of them received 6 months of danazol 600 mg/d, 9 patient were pre-treated with GnRH-agonists for 6 months (7 of them with add-back medication) and 20 were operated after 3 months of GnRH-Agonist medication. During the follow up period the following recurrences were observed: 1 of 3 cases with resection of the tumor only; 0 of 7 cases with resection of the nodule including resection of the anterior wall of the rectum; and 2 of 27 patients with bowl resection and anastomosis. Conclusion In case of rectovaginal endometriosis sufficient radical surgery is the preferred treatment. It is necessary to remove all nodules completely and preoperative medical treatment with GnRHAgonists seems to reduce the recurrence rates. Medical treatment is insufficient with a 100 percent recurrence rate. Permanent medication however is an alternative to surgery, if the patient accepts that treatment has to last until menopause. Literature 1. Nisolle M, Donnez J. Peritoneal endometriosis, ovarian endometriosis and adenomyotic nodules are three different entities. Fertil Steril 1997;68:585-96 681445250 2. 3. 4. Anaf A, Simon Ph, Fayt I, Noel J-C. Smooth muscles are frequent components of endometriotic lesions. Hum. Reprod 2000;15:767-71 Pierce SJ, Gazvani MR, Farquharson RG. Long-term use of gonadotropinreleasing hormone analogs and hormone replacement therapy in the management of endometriosis. Fertil Steril 2000;74:964-8 Redwine DB, Wright JT. Laparoscopic treatment of complete obliteration of the cul-de-sac associated with endometriosis: Long-term follow-up of en bloc resection. Fertil Steril 2001;76:358-65 2