1 st admission
advertisement

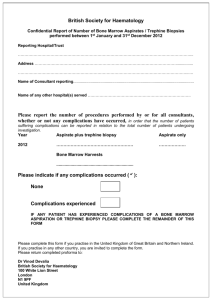
INTERHOSPITAL CONFERENCE 17 NOVEMBER 2009 10 years old boy Prolong fever, arthritis PATIENT DATA ผู้ป่วยเด็กชายไทย อายุ 10 ปี ทีอ่ ยู่ อาเภอเมือง จังหวัดกาฬสิ นธุ์ Chief complaint ไข้ สูง ปวดข้ อ 1 สั ปดาห์ ก่ อนมาโรงพยาบาล PRESENT ILLNESS 1 เดือนก่ อน มาด้ วยไข้ 7 วัน ปวดข้ อ ข้ อบวม SEM at LUPSB, liver 4cm below RCM Lt wrist, Lt knee and ankle then Rt ankle arthritis (migratory polyarthritis) INVESTIGATION 1 เดือนก่อน CBC: Hct 28.6%, Hb 9 g/dl, corrected WBC 9,600, N 37%, L 43%, M 18%, NRC 153/100 WBC, plt 117,000 MCV 72.9, MCH 22.9, MCHC 31.4, RDW 20.8 ESR 82 mm/hr, ANA-, ASO positive 1:1, RF -, CRP + 1:64, Melioid titer 1:40, H/C no growth, PPD CXR: mild cardiomegaly EKG: NSR, HR 120/min, QRS axis 750, PR 0.12 sec, QTc 0.38 sec, borderline LVH Echocardiogram: EF 76.8%, mild LV enlargement, trivial MR Dx: acute rheumatic fever: 1 major (poly arthritis), 2 minor ( fever, ESR, CRP), + evidence Strep infection (ASO+) Rx: cefotaxime x 8 d, amoxy+clavulanic acid x 6d, ASA gr V (90mkd) Severe joint pain, pain score= 10 : suspected malignancy/ JRA Brufen, tramol, MST, morphine syrup prn Prednisolone 2 MKD x 2 wk LDH 2,476 U/L uric acid 6.3 mg/dl, ESR 135 mm/hr, CRP 1:16, Coomb’s test –, ANA-, RF-, UA normal eye exam: no uveitis BMA: inadequate BM biopsy: fragment of cartilage, no bone marrow tissue seen Film bone survey: multiloculated cystic lesion at distal femur, no osteolytic lesion, suspected benign condition, No malignancy condition Bone scan: ? Ultrasound abdomen: hepatomegaly of Lt PRESENT ILLNESS 1 สั ปดาห์ ก่อนมาโรงพยาบาล มีไข้ สูง ส่ วนใหญ่ เป็ นไข้ กลางคืน ปวดเมื่อยต้ นขา 2 ข้ าง ปวดข้ อศอก ทั้ง 2 ข้ าง ข้ อมือ ข้ อนิว้ มือ ข้ อ เข่ าขวา ไม่ ไอ ไม่ หอบ ปวดศีรษะเล็กน้ อย ปัสสาวะอุจจาระปกติ ไม่ มีนา้ หนักลด รับประทานอาหารได้ 2 วัน ก่ อนมา ไข้ ตลอดวัน ปวดข้ อมากขึน ้ ปวดสะโพก 2 ข้ าง เดิน ลาบาก PAST HISTORY มีเลือดกาเดาไหลเป็ นๆหายๆ (ตั้งแต่ อายุ 3-4 ปี ปี ละ 3-4 ครั้ง) 7 เดือนก่ อน มาด้ วยไข้ 2 เดือน เบื่ออาหาร อ่ อนเพลีย ท้ องโตขึน ้ ซีดลง นา้ หนักลดลง 2 กิโลกรัม ใน 1 เดือน ตรวจร่ างกาย พบซีด ม้ ามโต 10 cm below LCM, CBC: pancytopenia BMA: erythroid hyperplasia, no blast BM biopsy: bony tissue with paucity number of hematopoietic cells without evidence of leukemia Lymph node biopsy at inguinal: reactive lymphoid hyperplasia PAST HISTORY CT abdomen: diffuse splenomegaly Splenectomy: diffuse sinusoidal hemangiomatosis with extramedullary hemopoeisis EBV Ig M +, IgG+, CMV IgM-, IgG+ Antibiotic 17 days Hb typing: Homozygous Hb E PAST HISTORY จากนั้นมา follow up ทุก 1 เดือน มีไข้ บางครั้ง เลือดกาเดาไหล เล็กน้ อย admit 1 ครั้ง เมื่อ 4 เดือนก่อน x 2 วัน Hct 29% WBC, platelet ปกติ ได้ รับ folic, MTV, zyrtec Family history มารดาเป็ นโรคหอบหืด มีญาติทางบิดาเป็ นโรคเลือด (ไม่ ทราบว่ าเป็ นโรคอะไร) ปฏิเสธประวัติมะเร็ งในครอบครั ว PHYSICAL EXAMINATION Vital signs: BT 39.70 C BP 110/70 mmHg PR 112/min RR 22/min BW 23 kg (P3-10) Ht 130 cm (P25) GA: A boy, fully consciousness, well co-operate HEENT: mild pale conjunctiva , anicteric sclera pharynx and tonsils: not injected Rt cervical lymph node 0.5 cm PHYSICAL EXAMINATION Heart : systolic ejection murmur gr II at LPSB Lungs : normal and equal breath sound, no adventitious sound Abdomen: soft, liver 3 cm below RCM Extremities: no edema Tender and swelling of bilateral elbow, wrist, 4th, 5th MCP, Lt 2nd, 5th MCP, Rt knee joint PROBLEM LISTS Prolong fever Polyarthritis Anemia Hepatomegaly SEM gr II S/P splenectomy Homozygous HbE DDX Infection: TB, virus (EBV, CMV), Bacteria, fungus Connective tissue disease: JRA, SLE Malignancy: acute leukemia, lymphoma IAHS LCH INVESTIGATION INVESTIGATION CBC: Hb 10.2 g/dL, Hct 31%, WBC corrected 4,900 N 45%, L 36%, M 18%, E 8%, NRC 91/100 WBC, Platelet 131,000 MCV 85.7 fl, MCH 28.2 pg, MCHC 32.9 g/dL BUN 5 mg/dL, Cr 0.4 mg/dL, Uric acid 3.4 mg/dL Na 139, K 3,8, Cl 97, CO2 29 mmol/L, Ca 8.9, Mg 2, P 4 mg/dL Albumin 2.4 g/dL, AST 54 U/L, ALT 37 U/L. ALP 520 U/L Hemoculture; no growth UA : pH 5.5 ,sp.gr. 1.025, wbc 1-2 , rbc 0-1 ESR : 75 mm/hr INVESTIGATION LDH 542 U/L Ferritin 3,840 ng/ ml B-HCG 1.11 mIU/ml, AFP 3.08 IU/ml ASO-, CRP-, Melioid 1:20 Bone marrow aspiration Multiple radiolucency lesions Ultrasound whole abdomen :diffuse hepatomegaly BMA: inadequate, rare nucleated cell, no blast Cytochemistry : numerous cell debris and very rare blood cell have been observed, no hematologic malignancy cell :Other cause of bone marrow destruction should be ruled out Flow cytometry: blast gate 2.63% of total event No evidence of hematologic malignancy 1st admission HISTOPATHOLOGY REPORT 1st admission Splenic hemagiomatosis (1st admission) Splenic hemagiomatosis (1st admission) Bone marrow biopsy: Bone marrow necrosis No malignancy cell Bone biopsy at Lt humerous: Bone marrow necrosis No malignancy cell BONE MARROW NECROSIS (BMN) Necrosis of myeloid tissue and medullary stroma in the large areas of hematopoietic bone marrow On BM biopsy: disruption of the normal bone marrow architecture with a considerable loss of fat space Aplastic anemia: only loss of myeloid tissue and no destruction of reticular structure Aseptic necrosis: no destruction of the spicular architecture Hypoxemia after failure of microcirculation: Inflammatory damage or mechanical obstruction : DIC, sickle cell disease or tumor cell plug Immune process Toxicity and the release of toxins, cytokines, or vasoactive substances from damaged cells : TNF Major complication: pancytopenia, embolic processes Repopulation of the bone marrow cavity can occur after BMN resolved IDENTIFIED UNDERLYING MALIGNANCY 90% Extensive search for neoplastic disease is justified whenever BMN is diagnosed 1st described by Wade and Stevenson, 1942 : Sickle cell disease, died of cerebral infarction Nies et al. 1965: define BMN in acute leukemia 34/ 316 (10.75%) postmortem Kiraly and Wheby.1976: 13/664 (2%) in BM specimens during 12 –year period Norgard, 1979. retrospectively reviewed 120/368 (32.5%), only 4 were diagnosed at initial GRADING Small necrotic lesions: <25% of the dimention of the biopsy (39%) Intermediate BMN < 50% (24%) Large BMN >75% (12%) Extensive: throughout the dimension of the specimen Pennaforte et al. 1986: extensive 4/1149 (0.3%) Maisel etal. 1988: severe BMN > 50% of dimension (3%) BMN IN CHILDREN Macfarlane and Tauro: 4/379 (1%) in ALL Pui et al: 7/1419 (0.5%) in cancer patients BONE MARROW NECROSIS (BMN) ANN M. JANSSENS ET AL. CANCER 2000 Clinicopathologic entity, rare condition Review 240 cases, 1980-1999 Inclusion 1. BMN diagnosed during life 2. necrosis > 50% of the diameter of biopsy specimen UNDERLYING DISEASE ASSOCIATION Malignancy 91% Hematologic malignancies 60% Acute leukemia 41%, lymphoma 15% ALL 18%, AML 13% Children 18/25 cases were ALL BMN developed before diagnosis: ALL 26/37 (AML 16/24) After induction chemotherapy 1/37 At recurrence 10/37 UNDERLYING DISEASE ASSOCIATION Solid tumors 30% Not found primary origin, even after extensive search 12/43 Non malignancy only 9%: sickle cell crisis, infection, drug, HUS, antiphospholipid syndrome, DIC, hyperparathyroidism, anorexia nervosa, idiopathic etc. 16/22 documented infection: underlying malignancy were found later (early - 1 yr) Infection E.coli Streptococcus Staphylococcus Citrobacter freundii Salmonella Mucormycosis Q fever TB Parvovirus HIV Drug Sulphasalazine Sulphathiazol Sulphanamide Interferon-alpha G-CSF ATRA Hydroxyurea Fludarabine PRESENTATION Bone pain 75% Fever 68.5% Anemia 91% Thrombocytopenia 78% Leukoerythroblastic picture 51% Elevated LDH, alkaline phosphatase 50% Leukoerythroblastic picture primitive red cells (nucleated rbc or erythroblasts) primitive white blood cells (myelocytes) Cytology Bone marrow aspiration can be unsuccessful Multiple aspirates from different sites (sternal, posterior iliac crest, etc.) Serosanguineous, watery dark red or clear fluid Histology Combination of gelatinous transformation and necrosis of the myeloid tissue Background of gelatinous transformation surrounds cellular debris with indistinct cellular margins, pyknotic nuclei, and abnormal eosinophilic staining cytoplasm The hallmark of bone necrosis: loss of osteocytes, osteoblasts, and osteoclasts background of amorphous extracellular eosinophilic material that surrounds cells that disintegrate. shows cells that lose their normal staining characteristics. irregular or indistinct margins; the cytoplasm can shrink or vacuolate, and the nucleus shows pyknosis, karyorrhexis, and karyolysis Bone Marrow Scanning Technetium 99m sulfur colloid and indium chloride localize selectively to the reticuloendothelial elements of the marrow Dx BMN, residual BM activity, guided biopsy, recovery MRI: changes in bone marrow signal intensities Life-threatening complication: embolization of fat and necrotic bone marrow to pulmonary arteries PROGNOSIS Median survival of the hematologic malignancies :1 - 4 months, 69% died Childhood ALL: 13/18 alive Survival: 4 months- 6 years Solid tumor and BMN: widespread metastasis, short survival PROGRESSION OF THE PATIENT High grade fever Petechiae hemorrhage at face, periorbital Increased hepatomegaly Blood component therapy, antibiotic, pain management Consult for liver biopsy Repeat BMA and biopsy Plan MRI liver and bone Steroid Hepatomegaly CBC Hb Hct cWBC NRC N L M E other D1 5.1 15.9 8.8 130 50 35 10 5 D3 6.7 21 3.3 200 32 41 13 4band2, meta2,myelo1, atyp L5 D10 6.1 19.5 11.7 80 36 44 16 4 D15 6.9 21.3 4.1 21 60 30 5 2band2 atypl1 D16 5.7 17.4 3.9 19 41 55 2 atyp3 D17 8.2 24.3 4.9 44 42 52 3 band 2, atyp1 D24 7.4 21.6 10.8 31 42 38 9 band6, atyp 5 D25 9 26.8 7.8 48 38 40 10 band2, meta3, myelo1, atyp 4, blast2 D30 7.4 22 3.2 50 49 32 9 blast10 D31 6.8 20.2 9.2 52 41 47 10 atyp2 D35 5.6 17 15.1 42 38 10 blast8,atyp2 Plt 172 144 27 7 74 21 40 30 49 34 13 Developed massive GI bleeding treatment: LPB, Platelet, FFP, antibiotic Cardiac arrest: CPR x 30 min ABG pH PCO2 PO2 HCO3 ABE O2 sat 7.07 19.2 444 5.7 -22 100 PT INR PTT D-dimer 31.2 2.67 34.4 0.6 mg/L Bone marrow aspiration at sternum BM biopsy from 1. right ASIS: Abnormal blast cells infiltrate with focal necrosis and crush artifact 2. A small amount of marrow tissue from Lt ASIS: abnormal blast cells 3. Sternum: numerous blast cell infiltrate : precursor T lymphoblastic leukemia/ lymphoblastic lymphoma CD3+, CD20-, CD79a-, CD34-, MPO-, TdT+ Liver biopsy : precursor T lymphoblastic leukemia/ lymphoblastic lymphoma CD3+, CD20-, CD79a-, CD34-, MPO-, TdT+ THANK YOU Extensive search for neoplastic disease Multiple aspirates from different sites : biopsy site in which viable hematopoietic bone marrow