G-CSF in healthy donors: How should we dose by ug/kg or
advertisement

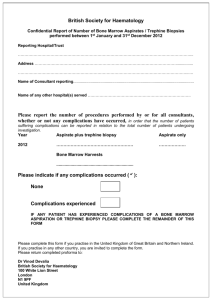
Disclosures of: Maciej Machaczka Dr. Maciej Machaczka has indicated he has the following affiliations: Company Research Support Employee Consultant Genzyme ✔ Actelion ✔ Shire HGT ✔ Stockholder Speakers Bureau Other The author declares that he has no conflicts of interest concerning his presentation entitled: Fine Needle Aspiration vs. Trephine Biopsy of Bone Marrow – Comparison of Utility in Diagnostics of Sporadic Cases of Gaucher Disease Type 1 – A Cytohistological Study FINE NEEDLE ASPIRATION VS. TREPHINE BIOPSY OF BONE MARROW – COMPARISON OF UTILITY IN DIAGNOSTICS OF SPORADIC CASES OF GAUCHER DISEASE TYPE 1 A CYTOHISTOLOGICAL STUDY Maciej Machaczka MD, PhD Senior Consultant and Research Scientist Department of Medicine and Hematology Center Karolinska, Karolinska Institutet and Karolinska University Hospital Huddinge, Stockholm, Sweden Bone marrow (BM) examination is generally no longer recommended for the sole purpose of Gaucher disease (GD) diagnosis Kilma Rossegar Bone Marrow Biopsy Needle • Common initial symptoms of GD type 1 such as thrombocytopenia or splenomegaly, often result in a referral of the patient to hematologist for diagnostics • In patients of Ashkenazi ancestry, the frequency of Gaucher disease is 1 in 800 while hematologic malignancies are much less frequent at 1 in 2,500 • In the non-Ashkenazi populations Gaucher disease is markedly less frequent (1 in 40,000) compared with hematologic malignancies • Among non-Jewish patients, initial symptoms of sporadic GD type 1 such as splenomegaly or thrombocytopenia, often lead to hematological diagnostics • Routine diagnostic measures include fine needle aspiration for the cytological assessment of bone marrow smears (BM-S) and trephine biopsy of bone marrow for the histological evaluation of bone marrow biopsies (BM-TB) • The results of the above mentioned examinations are often the first ones given the suspicion of GD in non-Jewish patients with a sporadic GD type, which should always be confirmed by enzymatic and genetic analysis • However, the choice of the bone marrow examination method in the sporadic cases of GD type 1 is often accidental, influenced by many different factors related both: - to the patient (e.g., concomitant symptoms, co-morbidities, local conditions at the examination site, etc) and - to the physician (e.g., local routines, personal experience, etc) Bone Marrow Aspiration Needle Bone Marrow Biopsy Needle • Trephine biopsy of BM was introduced in many countries into routine hematological diagnostics relatively recently (approx. for the last 20 years) and definitely at the time when BM examination (i.e., fine needle biopsy) was generally no longer recommended in GD • Thus, little is known about the comparison of accuracy of both methods in assessment of bone marrow involvement in GD, and further, about their utility in the diagnostics of sporadic cases of GD1 FINE NEEDLE ASPIRATION VERSUS TREPHINE BIOPSY OF BONE MARROW – COMPARISON OF UTILITY IN DIAGNOSTICS OF SPORADIC CASES OF GAUCHER DISEASE TYPE 1 – A CYTOHISTOLOGICAL STUDY • • • • • • • • Maciej Machaczka Sofie Regenthal Agnes Bulanda Krystyna Gałązka Grazina Kleinotienė Björn E. Wahlin Hans Hägglund Monika Klimkowska • The aim of the study was to compare the accuracy of cytological versus histological assessment of BM in patients with GD1 Material and Methods • BM-S (May-Grünwald Giemsa stain) and BM-TB (hematoxylin-eosin stain), previously obtained from 6 non-Jewish, sporadic GD1 patients (2 female and 4 male) for diagnostic purposes, were retrospectively analyzed • median age 65 years (range 21–84 years) • 3/6 pts were splenectomized • 5/6 pts carried at least one allele with a N370S (c.1226A>G) mutation in the GBA1 gene • BM samples were collected from an entry site on the posterior iliac crest of the patients in the prone position BM examination Bone marrow is collected from an entry site on the posterior iliac crests of the donor in the prone position (on his or her abdomen) The skin is cleansed, and a local anesthetic (e.g., lidocaine) is injected to numb the area The posterior iliac crests (arrows) are common sites for bone marrow aspiration and biopsy BM examination Bone Marrow Aspiration Needle Bone marrow aspiration needles are smaller than needles used to obtain bone marrow biopsies 1 - T-Lok™ Biopsy Needle 2 - Extraction Cannula 3 - Marked Obturator / Probe T-Lok™ Bone Marrow Biopsy Needle Spicules obtained from the BM aspirate are smeared on glass slides Bone marrow aspiration Core biopsy obtained with BM biopsy needle Bone marrow biopsy BM examination After the procedure is complete, the patient is typically asked to lie flat for 5–10 minutes to provide pressure over the procedure site. After that, assuming no bleeding is observed, the patient can get up and go about their normal activities Material and Methods (2) • differential counts of BM-S were estimated in the ×40 objective of Olympus BX 40 microscope • each patient sample consisted of 2 slides where 500 nucleated cells were counted on each slide • assessment of the composition of BM-TB (i.e., proportion of hematopoietic tissue, Gaucher cells, fat tissue, and trabecular bone) was carried out using digital photographs analyzed on a computer utilizing the Gimp 2 software • photographic documentation of BM-S and BM-TB was made with a digital camera (Nikon DX m 1200F) in the Nikon Elipse E1000 microscope, using x40 objective for the BM-S and x2 respective x20 objectives for the BM-TB Results Results Cytological and histological picture of bone marrow taken through the aspiration and trephine biopsy. GD type 1 (hematoxylin-eosin staining) Results The results of cytological analyses of BM-S including identified GCs are showed in Table 1. The median number of GCs identified in one patient was 4 (range 1–18), and the median percentage of GCs was 0.4% (range 0.1–1.8%) Results (2) The proportions of hematopoiesis, GCs, fat tissue, and trabecular bone in the BM-TBs from the patients are presented in Table 2. The absolute proportion of GCs in BM-TB ranged from 22–36% (median value 28%). The proportion of GCs to hematopoietic tissue ranged from 34–54% (median value 47%) Results (3) • In all 6 patients, the the median proportion of identified GCs to hematopoietic tissue were much larger in the BMTB (range 34–54%) than in the BM-S (range 0.1–1.8%), and this difference was significant in Wilcoxon signedrank test (P=0.028) Conclusions • • • • The majority of the studied patients (4/6, 67%) had ≤6 GCs among 1,000 counted nucleated hematopoietic cells on BM-S Of note, routine differential counts of BM-S are usually performed on only 200 nucleated hematopoietic cells GCs are often tightly packed within the regions engaged by GCs in BM and thus are difficult to aspirate, which can explain our finding. Additional problems with aspiration of GCs can result from an increased reticulin fibrosis of the BM Our results indicate that fine needle aspiration of BM is an unreliable diagnostic method to detect GCs in sporadic cases of GD1. There is a serious risk of not diagnosing GD when using only fine needle aspiration Conclusions (2) • The sensitivity of trephine biopsy for detecting GCs in BM is high and, in our study, detected GCs burden was approx. 100 times higher compared with fine needle aspiration • However, trephine biopsy is a more advanced procedure, it should be performed by an experienced physician, and is not recommended for the sole diagnostic purpose in GD Conclusions (3) • Patients with unclear splenomegaly and/or thrombocytopenia, who display a negative result in BM-S assessment should proceed routinely to enzymatic diagnostics of GD (β-glucosidase and chitotriosidase activity assays) Thanks to collaborators at Karolinska Institutet and Karolinska University Hospital in Stockholm • • • • • Dr. Monika Klimkowska Prof. Jan Palmblad Prof. Per Svenningsson Dr. Björn Wahlin Assoc. Prof. Hans Hägglund