Eating Disorders - Cystic Fibrosis Trust
advertisement
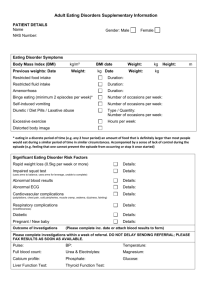
Nutrition and Body Image in Adolescents with CF Alison Morton Consultant Dietitian, St James’ Hospital, Leeds Dr Mandy Bryon Consultant Clinical Psychologist, GOSH Importance of Nutrition in CF Positive association between nutritional status and lung function (Zemel et al., 2002; Steinkamp et al, 2002; Peterson et al., 2003; Kastner-Cole et al., 2005; Pedreira et al., 2005) Positive association between survival and body weight, height and BMI (Kraemer et al., 1978; Corey et al., 1988; Beker et al., 2001; Sharma et al., 2001; Stern et al., 2008) Importance of Nutrition in CF Impact of poor nutritional status on health in CF Delayed puberty (Dodge, 1992; Johannesson et al., 1997; Arrigo et al., 2003; Umlawska et al., 2010) Decreased exercise tolerance (Marcotte et al., 1986; de Meer et al., 1999) Impaired respiratory muscle function (Zemel et al., 2000) Change in BMI at Leeds Adult Unit Importance of Nutrition in CF BMI and Acute Exacerbations Adults 100% 80% 60% 3+ 2 40% 1 20% 0 0% 15 17 19 21 23 25 27 29 31 33 BMI Data from Hebe Quinton CFF Patient Registry Association of Body Mass Index with Common Complications 50% Glucose Problems 40% 30% CFRD 20% Osteopenia/osteoporosis 10% 0% 15 17 19 21 23 25 27 29 31 33 Data from Hebe Quinton CFF Patient Registry 35 Age Distribution of Death 2011 Median age of death 26 years – adolescence is a time of vulnerability Optimising Nutrition in Adolescence is Essential… Optimising Nutrition in Adolescence is Essential… Energy & protein requirements greatest at time of peak growth 95% peak bone mass achieved by the end of the pubertal growth spurt BUT Adherence issues Independence and risk taking behaviour Peer pressure Body weight struggles and body image challenges Diagnostic Criteria for Eating Disorders Anorexia Nervosa Refusal to maintain minimal body weight Fear of weight gain or fatness Body shape/weight disturbance Amenorrhoea Bulimia Nervosa Recurrent binge eating Inappropriate behaviour to prevent weight gain Self-evaluation based on shape/weight CF-related Eating Attitudes and Behaviours Clinically observed in CF: Poor appetite even when free of infection (Durie & Pencharz, 1989) Avoidance of foods associated with gastro-intestinal symptoms or reduction of overall food intake (Murphy & Wooton, 1998) Manipulation of enzyme or insulin use (Bryon et al., 2008) Non-adherence to dietary supplements or recommendations (Gilchrist & Lenney, 2008) Pressure from others to eat (Abbott et al., 2000, 2007) Feeling full easily (Pumareiga et al., 1986) Denial of hunger (too ill to eat) (Pumariega et al., 1986) Idiosyncratic: fear of stomach pushing up into lungs, choking on food if eat too fast (Pumariega et al., 1986) Neil 15 years Neil aged 15 years lives with both parents. Father is diagnosed with a mental health problem. Neil complained a few years ago of hating his fat stomach and didn’t like having to eat high fat foods. Neil’s rate of weight increase slowed and it transpired that he had in mind a set weight that he would not go over (underweight for height). He recently became vegetarian and stopped Creon and vitamins for moral reasons. His weight gain is static. Maddie 17 years Lives with both parents and younger sister, not CF. Very well until aged 15, weight loss ++, Pa growth, IV’s. Refused to attend school, very shy. Hates how her body looks, very selective in food range, only drinks water. Very supportive and concerned parents. Difficult to engage Maddie in any consultation, speaks through mum. Group 1 Thinking about the two cases: What could be the signs that someone is having problems with body image and eating disturbance? What might contribute to the problem? Group 2: From your clinical experience what have you found to be helpful and unhelpful in cases like these? Beginning Approach Avoid judgment Avoid being the food police Avoid hyper focus on weight Think first before talking about specifics e.g. weight goals, specific energy targets, weight changes Questioning/Getting to Know Habits and Patterns Open ended questions about eating/mealtimes Typical routine for school/work, weekend, holidays What are their challenges and concerns with weight, food, body image? More Detailed Questioning Are you concerned about your weight? Are you concerned about your appearance? How do you handle these concerns? How much do you want to weigh? How often do you weigh yourself? Anything about your body you want to change? Do you take Creon as recommended? Do you have any difficulties buying/preparing food? Team Approach is Best Remain a team and use all members Act but be careful and mindful of approach Communication is essential CF teams have a lot of resources when expertise is pooled but… If eating disorders is suspected ask for expert help Conclusion The existence of eating disturbance and disturbed body image is of concern in adolescents and adults with CF These adolescents and adults have lower selfesteem than those without eating disturbance and are likely to have other stressors Consideration of team pressures on eating attitudes and behaviours Need for early identification and treatment of any disturbance – screening tool