Nelson – pedi cardiology MURMURS ONLY
advertisement
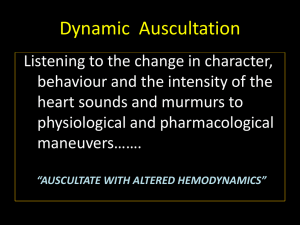
Pediatric cardiology JFK pediatric core curriculum MGH Center for Global Health Pediatric Global Health Leadership Fellowship Credits: Brett Nelson, MD, MPH Discussion • Cardiac evaluation • Auscultation • Distinguishing pathologic from innocent murmurs • Common innocent pediatric murmurs • Further work-up of a concerning murmur Initial cardiac evaluation • History: poor feeding, diaphoresis, FTT, family hx • Vital signs: height, weight, HR, RR • Inspection: dysmorphism, cyanosis, clubbing • Palpation: presence and quality of distal pulses; precordium for PMI and thrills; liver • Auscultation (further cardiac evaluation to follow…) Auscultation • Rate & regularity • Heart sounds – Focus particularly on intensity and quality of S2 and for presence of extra heart sounds (S3, S4) • Murmurs… • Clicks – Abnormal valvular sounds (e.g. ejection clicks in early systole, MVP in mid/late systole) • Rub – Associated with pericarditis; scratchy sound best heard at apex (may diminish if pericardial effusion becomes large) Auscultation Heart sounds • S1: closing of the AV valves – mitral then tricuspid • S2: closing of the semilunar valves – aortic then pulmonary • S3: ventricular overload – “TEN-NE-see”: S1, S2, s3 – <40yrs, pregnancy, MR/TR, CHF • S4: decreased LV compliance – “ken-TUCK-Y”: s4, S1, S2 – more likely than S3 to be pathologic (HTN, CAD, cardiomyopathy), although can be normal (athletes) Murmurs • Secondary to turbulent blood flow • Assess: – Intensity / loudness – Timing (systolic, diastolic, continuous) – Location of maximal intensity – Transmission / radiation – Quality (high-pitched, blowing, vibratory, harsh, soft) Murmurs: grading of intensity • I barely audible • II soft, but easily audible • III moderately loud without thrill; roughly as loud as S1/S2 • IV loud with a thrill • V audible with stethoscope barely on chest • VI audible with stethoscope off chest Murmurs: timing Maneuvers to dynamically evaluate murmurs • Inspiration typically increases murmurs originating from the right heart – Negative pressure temporarily increases venous return • Expiration typically increases murmurs originating from the left heart – Less LV restriction due to lower RV volumes • Increasing overall venous return (supine, squatting, legraise) can accentuate flow-type murmurs – Can also delay MVP click due to “tighter” chordae tendinae • Standing increases the murmur of hypertrophic cardiomyopathy (HOCM/IHSS) – Decreased venous return smaller LV volume closer apposition of LV walls Distinguishing pathologic from innocent murmurs Innocent murmurs • The prevalence of innocent murmurs in infants is as high as 60% – Versus: the incidence of congenital heart defect is 6 in 1000 (0.6%) • Innocent murmurs are usually… – early systolic – Grade I or II – poorly transmitted – Not associated with other findings Pathologic murmurs (1) • Murmurs that are… – Loud (Grade III+) – Diastolic – Abnormal heart sounds (e.g. S3/S4 gallop) – Long in duration – Systolic and associated with clicks – Louder upon standing Pathologic murmurs (2) • Murmurs that are associated with… – Abnormal or absent pulses – Unequal blood pressures – Cyanosis – Symptoms (e.g. syncope, chest pain) – Abnormal EKG / CXR – Syndromes, dysmorphism, other birth defects (e.g. CHARGE syndrome, DiGeorge, trisomy 21) Common innocent murmurs Still’s murmur • Most common innocent murmur, usually found between the ages of 3 and 6 • Thought to be due to turbulence in LV outflow or to vibration of fibrous tissue bands crossing LV lumen • Typically grade II-III, midsystolic, LLSB, and classically described as “vibratory” • Decreases with standing • Increases with fever, exercise, anemia Pulmonary flow murmur • Accounts for 15% of all innocent murmurs • Heard in infants and school-aged children • Due to turbulent flow at the origin of the right and left pulmonary arteries • Grade I-III, midsystolic ejection, heard at the ULSB, higher pitched than a Still’s murmur • Like Still’s, increases with fever, exercise, and anemia Peripheral pulmonary stenosis (PPS) of the newborn • Due to the physiologic relative stenosis of the right and left pulmonary arteries • Usually disappears by 1 year of age • Grade I-II, midsystolic ejection, heard at the ULSB with radiation to the axillae and back Venous hum • Seen in preschool-aged children • Due to turbulence in the jugular venous system • Continuous supraclavicular murmur heard throughout the cardiac cycle (usually right side > left side) • Disappears when the patient is supine, when the head is rotated, or with manual compression of the neck veins Supraclavicular arterial bruit • Due to turbulence in the major brachiocephalic arteries as these vessels arise from the aorta • High-pitched, systolic ejection murmur heard best in the right supraclavicular fossa • Decreases with raising of the chin, throwing back the shoulders, or firm pressure on the subclavian artery • Increases with slight pressure on the subclavian artery Further cardiac evaluation (as available) • Four-extremity blood pressures • Pre- and post-ductal pulse oximetry – O2 saturation <93% in the lower extremities is abnormal – Clinical cyanosis is not seen until saturation <88% • EKG • CXR • Cardiology referral and echocardiogram (definitive test) Resources 1. ** Online audio of heart sounds and murmurs ** http://depts.washington.edu/~physdx/heart/demo.html 2. 3. 4. 5. 6. 7. Patel J. “Evaluation of Pediatric Murmurs.” San Antonio, TX. http://www.texasnp.org/resources/2006_conference/PediatricMur murs%5B1%5D.ppt. McConnell ME, Adkins SB, Hannon DW. “Heart murmurs in pediatric patients: when do you refer?” American Family Physician. November 1999. http://www.aafp.org/afp/990800ap/558.html. How to distinguish between innocent and pathologic murmurs in childhood. Pediatric Clinics of North America. 1984 Park MK. Pediatric Cardiology For Practitioners. Bricker T. The Science and Practice of Pediatric Cardiology. Allen H. Moss & Adams: Heart Disease in Infants and Children.