circi

C
RITICAL
I
LLNESS
R
ELATED
C
ORTICOSTEROID
I
NSUFFICIENCY
CIRCI
: Current Status 2013
Karyn L. Butler, MD, FACS, FCCM
Chief, Surgical Critical Care
Hartford Hospital
Associate Professor of Surgery
University of Connecticut
Hartford, CT
Background
1940’s:
‘Relative Adrenal Insufficiency”: activation of adrenal response, inadequate for magnitude of insult Pollak H. Lancet 1940
Adrenalectomised animals exposed to shock had high mortality
(Seyle et al.)
1980’s
Etomidate impairs cortisol synthesis
Increased mortality 28 to 77% in trauma patients (Watt et al.
Anesthesia 1984)
1990’s
Patients with MSOF improve after GC treatment ( Arch Surg 1993)
….Hydrocortisone did not improve survival or reversal of shock in patients with septic shock.
The etomidate debate is currently in clinical equipoise in which there is genuine uncertainty within the expert medical community.
Key questions
Terminology?
How is the diagnosis established?
When / How to treat?
Does therapy make a difference?
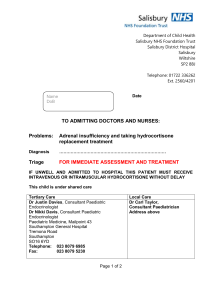
ADDISON’S DISEASE
RELATIVE ADRENAL
INSUFFICIENCY
CRITICAL ILLNESS
CORTICOSTEROID
INSUFFICIENCY
RAI CIRCI
ACCM Consensus
C ritical
I llness-
R elated
C orticosteroid
I nsufficiency
(
CIRCI
)
Absolute or Relative adrenal insufficiency should be avoided
Inadequate cellular corticosteroid activity for the severity of the patient’s illness
Dynamic / Reversible
Crit Care Med 2008
….the evidence to support its existence as a relevant clinical entity is currently not compelling….We therefore suggest that the terms “RAI” and “critical illness related corticosteroid insufficiency” be abandoned….
Key questions
Terminology?
How is the diagnosis established?
When / How to treat?
Does therapy make a difference?
Result of stress response?
CIRCI
Potentiate organ dysfunction?
The Stress Response
Activation of hypothalamic-pituitary-adrenal (HPA) axis essential to maintenance of cellular and organ homeostasis
HPA axis failure common in systemic inflammation
Incidence ~ 20%
60% in septic shock ( Anane et al Am J Resp Crit Care Med 2006)
“Adrenal failure”
CAP
Trauma
Head Injury
Burns
Liver Failure s/p Cardiac Surgery
Cortisol physiology
Cortisol physiology
Increases blood pressure
Increases sensitivity to vasopressor agents (increases transcription and expression of receptors)
Increases endothelial nitric oxide synthetase
(maintaining microvascular perfusion)
Reduces number and function of immune cells at sites of inflammation
Decreases the production of cytokine/ chemokines
Enhances macrophage migration inhibitory factor
Cortisol physiology
Major endogenous GC secreted by adrenal cortex
> 90% bound to CBG
Decreased CBG during acute illness free cortisol
Cortisol binds to intracellular receptors
Activates or represses gene transcription
Inhibit NF
B by increasing I
B transcription
Cortisol physiology
Cortisol binds to intracellular receptors
Activates or represses gene transcription
Inhibits NF
B by increasing I
B transcription
How to establish diagnosis?
Measure cortisol
Free vs. total
Timing (random vs. other)
Association with severity of illness
Gender differences
Measure provoked cortisol production
ACTH ‘stim’ test (low vs. high dose)
Threshold for mortality
?
How to establish diagnosis?
ACTH stimulation test
SHOULD NOT be used to identify those patients with septic shock or ARDS who should receive GC’s (2B)
Normal range of free cortisol is unclear
No test is able to measure GC resistance at the tissue level
Unclear what level of circulating cortisol is needed to overcome tissue resistance
ACCM consensus Crit Care Med 2008
Key questions
Terminology?
How is the diagnosis established?
When / How to treat?
Does therapy make a difference?
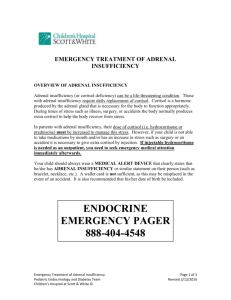
When / How to treat?
Hydrocortisone should be considered in patients with septic shock who have responded poorly to fluid resuscitation and vasopressors (2B)
Meta-analysis of 6 RCT
Hydrocortisone 200-300 mg/day
Greater shock reversal at day 7
No change in mortality
Methylprednisolone 1 mg/kg/day x 14 days for early severe ARDS (pO
2
/F
I
O
2
< 200)
ACCM consensus Crit Care Med 2008
When / How to treat?
Dose should be adequate to down-regulate the proinflammatory response without causing immune-paresis or interfering with wound healing
GC dose reduced slowly to avoid rebound inflammation
Dexamethasone
NOT indicated
Immediate and prolonged HPA axis suppression
ACCM consensus Crit Care Med 2008
When / How to treat?
1. IV hydrocortisone 200 mg/day if hemodynamically unstable despite fluid resuscitation and vasopressor support (2C)
2.
Do not use ACTH ‘stim’ test to identify who receives
GC therapy (2B)
3. Taper GC when vasopressors no longer required
(2D)
4. Do not use in sepsis if no shock (1D)
5. Continuous infusion (2D)
Key questions
Terminology?
How is the diagnosis established?
When / How to treat?
Does therapy make a difference?
Methylprednisolone infusion in early severe ARDS
Results of a Randomized Controlled Trial
Meduri GU, Golden E, Freire AX,
Umberger R et al.
Memphis Lung Research Program
Chest 2007; 131:954 - 963
Study design
Randomized, double blind, placebo controlled
Five ICU’s in Memphis
91 patients with severe early ARDS (<72h)
Randomized to MP x 28 days (1mg/kg/d) vs. placebo
Outcomes
Reduction in lung injury score
Successful extubation by day 7
Results
MP n=63, Placebo n= 28
Reduction of LIS: 69.8% vs. 35.7%; P=0.002
Extubation: 53.9% vs. 25%; P=0.01
MP: lower CRP levels, decreased MV LOS, decreased
ICU LOS
Mortality: 20.6% vs. 42.9%; P= 0.03
Conclusions
Down regulated SIRS
Improved pulmonary and extrapulmonary organ dysfunction
Reduced duration of MV and ICU length of stay
Associated with decreased mortality
Glucocorticoids and CPB
1966: “…it is conceivable that such
[glucocorticoid] administration before prolonged cardiopulmonary bypass in humans would be of value.”
–Moses ML et al. J Sur Res
Glucocorticoids and CPB
1966: High dose dexamethasone attenuates lysosomal enzyme release after CPB
Beneficial effects of methylprednisolone 15-30 mg/kg prior to CPB prevented pulmonary vascular and alveolar architectural changes (early 1970’s)
Initial studies from 1970’s to early 2000 not promising
Stress doses of hydrocortisone reduce severe systemic inflammatory response syndrome and improve early outcome in a risk group of patients after cardiac surgery
Kilger E, Weis F, Briegel J, Frey L et al.
University of Munich
Crit Care Med 2003; 31:1068 - 1074
Study design
Prospective noninterventional trial to identify patients at high risk for SIRS
Prospective randomized interventional trial of prophylactic hydrocortisone in target population
Exclusions:
Renal insufficiency Cr > 2 mg/dL
Insulin dependent diabetes mellitus
Body mass index > 30 kg/m 2
Risk Factors
Duration of CPB > 97 minutes
EF < 40%
CABG with 4 or more grafts
Planned valve + CABG
Methods
High risk patients randomized to:
Stress dose hydrocortisone: 100 mg bolus before anesthesia, continuous infusion 10 mg/hr tapered over 4 days
Placebo
Serum Il-6 levels before anesthesia and 6 hours after
CPB
Hemodynamic variables
Length of stay data
Conclusions
Preoperative risk stratification is pivotal to provide effective anti-inflammatory prophylactic treatment
Peri-operative continuous hydrocortisone reduces systemic inflammation
Study not powered to detect reduction in mortality rate at 30 days
Stress doses of hydrocortisone reduce chronic stress symptoms and improve health-related quality of life in high-risk patients after cardiac surgery: a randomized study
Weiss F, Kliger E, Roozendaal B. et al.
University of Zurich, University Munich, UCSF-Irvine
J Thorac Cardiovasc Surg 2006; 131:277-282
Background
High stress exposure
Increased catecholaminergic activity
Decreased HPA activity
Post-operative chronic stress symptoms (PTSD?)
Impairments in mental health
Decrease HRQL
Study design
36 High risk patients
EF < 35%
CPB > 97 minutes
Prospective, randomized, double blind trial
Randomized to stress dose hydrocortisone (4 days) or placebo
HRQL questionnaire 6 months post-op
Traumatic memories
Chronic stress symptoms
Results
Conclusions (6 months post-op)
Stress dose hydrocortisone in high-risk cardiac surgical patients:
Reduces peri-operative stress exposure
Decreases chronic stress symptoms
Improves Health-related quality of life
Cardiopulmonary and systemic effects of methylprednisolone in patients undergoing cardiac surgery
Liakopoulos OJ, Schmitto JD, Kazmaier S. et al.
University of Gottingen, Germany
Ann Thorac Surg 2007; 84:110-119
Study design
Elective CABG
Exclusion:
Emergency or concomitant cardiac surgical procedures
Age > 80 years
EF < 30%
AMI < 4 weeks
Renal dysfunction
Methylprednisolone 15 mg/kg 30 minutes before CPB
Main outcome measures
Hemodyanmic parameters
Cytokine, troponin and CRP levels
Mechanical ventilation, LOS
Conclusions
Glucocorticoid treatment before CPB:
Attenuates perioperative release of systemic and myocardial inflammatory mediators
Improves myocardial function
Potential cardioprotective effect in patients undergoing cardiac surgery
Surgical practice changed
Corticosteroids for the prevention of atrial fibrillation after cardiac surgery: a randomized controlled trial
Halonen J, Halonen P, J
ä rvinen O. et al.
Kuopio University Hospital, Finland
JAMA 2007; 297:1562-1567
Study design
3 University hospitals
241 patients (age 30-85 years)
Exclusion:
AF or flutter
Uncontrolled DM
Infection
Cr >2 mg/dL
Randomized to Hydrocortisone (100 mg) or placebo
First dose post- op, then q8h x 3 days
All patients received metoprolol according to HR
Sample size based on reduction of AF 30% to 15%
Outcome measures
Occurrence of AF during the first 84 hours after cardiac surgery
Study protocol discontinued after first episode of AF
Meta-analysis of RCT of primary outcome of AF (2 + present study)
Conclusions
Intravenous hydrocortisone reduced the relative risk of post-op AF by 37%
Meta-analysis confirmed beneficial effect of corticosteroid treatment over placebo
No serious complications associated with steroid use
Modifiable
Risk
Factor?
CIRCI
Marker of
Illness
Severity?
Summary
ACCM Consensus 2008
1.
2.
3.
4.
Hydrocortisone ( 200-300 mg/day ) for patients with septic shock despite fluid resuscitation and vasopressors (2B)
ACTH stimulation test
SHOULD
NOT be used to identify who should receive GC’s (2B)
GC dose reduced slowly to avoid rebound inflammation
Methylprednisolone 1 mg/kg/day x
14 days for early severe ARDS
(pO
2
/F
I
O
2
< 200)
1.
2.
3.
4.
5.
Surviving Sepsis 2012
IV hydrocortisone 200 mg/day if hemodynamically unstable despite fluid resuscitation and vasopressor support (2C)
Do not use ACTH ‘stim’ test to identify who receives GC therapy
(2B)
Taper GC when vasopressors no longer required (2D)
Do not use in sepsis if no shock
(1D)
Continuous infusion (2D)