Parenteral/Enteral Nutrition in Neonates
advertisement
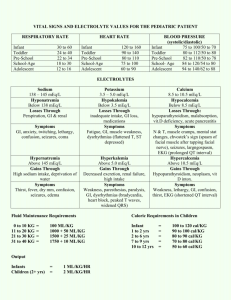
Parenteral and Enteral Nutrition in Neonates NICU Night Team Curriculum Objectives • Define basic nutritional requirements for neonatal growth • Describe specific nutritional problems faced by low birthweight and premature infants • Know components and advantages of breastmilk; indications for specific types of formulas • Determine components of TPN and be able to write fluid orders • Formulate an individualized plan for starting and advancing parenteral/enteral feeds Goals of Nutrition • To achieve a postnatal growth at a rate that approximates the intrauterine growth of a normal fetus at the same post-conceptional age • Provide balance in fluid homeostasis and electrolytes • Avoid imbalance in macro-nutrients • Provide micro-nutrients and vitamins Case A 26 week female is born precipitously to a healthy 20 year old G1P1 with an uncomplicated pregnancy. The baby is transferred to the NICU where a UAC and UVC are placed. You are getting ready to order fluids for this baby. What is your goal growth for this infant? What is this infant’s caloric requirement? What fluids do you order? Gastrointestinal Development • Fetal swallowing, motility in 2nd trimester – 18 week fetus swallows 18-50ml/kg/day – Term 300-700ml/day – Fetal swallowing regulates the volume of amniotic fluid and controls somatic growth of the GI tract • • • Intestines double in length from 25-40 weeks Functionally mature gut by 33-34 weeks Intestine in final anatomic position by 20 weeks • Premature Infant GI tract: – Delayed gastric emptying seen in preterm • Breast milk, glucose polymers, prone positioning facilitate gastric emptying – Total gut transit time in preterm 1-5 days – Stooling delayed until after 3 days – feeding volume ’s motility Growth – General Facts • Last trimester of pregnancy – Fat and glycogen storing – Iron reserves – Calcium and phosphoruos deposits • Premature babies more fluid (85%-95%), 10% protein, 0.1% fat. – No glycogen stores • The growth of VLBW infants lags considerably after birth Growth Goals • Weight: 20-30 g/day • Length: ~1cm/week • HC: 0.5cm/week – Correlates with brain growth and later development Caloric Requirements for Growth • Preterm goal: ~120kcal/kg/day • Term goal: ~110kcal/kg/day • Total Fluid of enteral feeds required to deliver adequate calories for growth is ~150cc/kg/day Total Parenteral Nutrition Determine fluid requirement (mL/kg/day) for first day of life Full-term infants: 60–80 mL/kg/day Late preterm and preterm infants (30–37 weeks): 80 mL/kg/day Very-preterm infants: 100–120 mL/kg/day Determine Glucose Infusion Rate (GIR) GIR: (% dextrose x IV rate ) ÷ (6 x wt in kg) Calculate GIR from known dextrose concentration (%). Example: An infant weighs 2 kg and is receiving 100 ml/kg/day of dextrose 15% solution. – – IV rate: 100 × 2 = 200 ml/day ÷ 24 = 8.3 ml/hr GIR: (15% x 8.3 x 0.1667) ÷ 2 = 10.3mg/kg/min (15% x 8.3 ) ÷ (6 x 2) = 10.3 mg/kg/min Total Parenteral Nutrition Protein and amino acids • Start with 2- 3 g/kg/day – • • • Increase 0.5–1.5 g/kg/day to a total of 3–4 mg/kg/day Goal for premature infants: 4g/kg/day Goal for term infants: 3g/kg/day Source: trophamine Calculate electrolytes to add to bag • DOL#1: dextrose in water with no eletrolutes is usually appropriate except in premies with low Ca stores who may require Ca DOL#2: add electrolytes to the bag based on estimated daily requirements and BMP • – Estimated Needs: • NaCl = 2-4 mEq/kg/day • KCl = 1-2 mEq/kg/day (NOTE: Do not supplement K until UOP >1cc/kg/hr, especially in premies) • CaGluconate =200-400mg/kg/day (NOTE: mg not mEq and Ca cannot be infused at >200mg/kg/day through a central line) Total Parentral Nutrition Other added nutrients • Lipids • Cystein • Phosphrous • Magnesium • Trace Minerals • MVI • Heparin Central TPN • • • • • • • • Easy to meet nutrition needs No limits on osmolarity Little risk of phlebitis Long term use May require general anesthesia Greater risk of infection Increased cost Greater risk of mechanical injury, air embolism, venous obstruction Peripheral TPN – Unable to meet needs for Ca/Phos needs – Maximum rate of Calcium gluconate is 200mg/kg/d – Maximum % dextrose is 12.5% – Short term use – Less risk for catheter related infections – Lower cost ? – Less risk of mechanical injury, air embolism, venous obstruction Total Parenteral Nutrition Enteral Nutrition • Breast milk is best! • The American Academy of Pediatrics (2005) recommends breastfeeding for the first year of life. • Started when an infant is clinically stable • Absence of food in the GI tract produces mucosal and villous atrophy and reduction of enzymes necessary for digestion and substrate absorption • Trophic hormones normally produced in the mouth, stomach, and gut in response to enteral feeding are diminished. • Breastmilk and standard infant formula have 20kcal/30cc (30cc=1oz) • Specialized formulas and fortifiers allow caloric content to be increased Breastmilk • • • • • • • • Preferred source of enteral nutrition Very well tolerated by most infants Improves gastric emptying time Matures the mucosal barrier Promotes earlier & appearance of IgA Vastly ’s incidence of NEC More significant induction of lactase activity compared to formula fed premies Composition: – – – – Varies with gestation Varies according to maternal diet Varies within a feeding( fat in last ½ fdg) Varies within the day( fat in PM over AM) Enteral Nutrition in the NICU • Term: – If clinically stable, start PO ad lib feeds and advance as tolerated • Preterm – Feeds are often initiated with breastmilk, Sim 20 or SSC 24 – Trophic tube feeds may be continuous or bolus and advanced gradually (10-20mL/kg/day) – Transition to bolus from continuous typically begins after achieving full feeds – PO feeds typically attempted around 32-34 weeks, when premies develop suck and swallow coordination – Premies are often supplemented with TPN as they work up on feeds – Goal discharge formula is Neosure 22 What to Feed? What to Feed? Practice Problems Baby boy B weighs 1.2 kg. The IV rate is 6.8 ml/hr, and the IV fluid contains the following: • 1.5 mEq of sodium per 100 ml • 1.9 mEq of potassium per 100 ml • 3.0 mEq of calcium per 100 ml • 1.2 mMol of phosphorus per 100 ml. Calculate the amount of sodium/kg/day, potassium/kg/day, calcium/kg/day, and phosphorus/kg/day that baby boy B is receiving. Answer: • • • • 2 mEq of sodium/kg/day 2.6 mEq of potassium/kg/day 4.1 mEq of calcium/kg/day 1.6 mMol of phosphorus/kg/day Practice Problems Baby boy C weighs 1.5 kg. Total IV fluids are to be calculated at 140 ml/kg/day. The infant is receiving central TPN. Lipids are 2 gram/kg/day. Write TPN orders (including dextrose concentration and IV rates) to give baby C a glucose infusion rate of 8 mg/kg/min. Write orders for 4 mEq/kg of sodium, 2 mEq/kg of potassium, 3.5 mEq of calcium, and 1.5 mMol of phosphorus to be added to every 100 ml of IV base solution. Answer: • • • • • • Lipids: 0.6 ml/hr PN fluids: dextrose 8.9% at 8.1 ml/hr Sodium: 3.1 mEq per 100 ml Potassium: 1.5 mEq per 100 ml Calcium: 2.7 mEq per 100 ml Phosphorus: 1.1 mMol per 100 ml References • • • • American Academy of Pediatrics, Section on Breastfeeding. (2005). Policy statement: Breastfeeding and the use of human milk. Pediatrics, 115(2), 496–506. Carlson, C, Shirland, S. Neonatal Parenteral and Enteral Nutrition, Resource Guide. National Association of Neonatal Nurse Practitioners Adamkin, D. Nutrition Management of the Very Low-birthweight Infant: I. Total Parenteral Nutrition and Minimal Enteral Nutrition. NeoReviews 2006;7;e602-e607 Hay, W. Strategies for Feeding the Preterm Infant. Neonatology. 2008 ; 94(4): 245–254. Thank you NNPs Carol and Terri!