GLOMERULAR DISEASES - Antonio V. Cayco,MD
advertisement

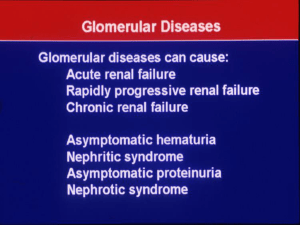
GLOMERULAR DISEASES Antonio V. Cayco, MD Section of Nephrology OBJECTIVES Introduction Approach to Glomerular Diseases • Syndrome Diagnosis • Clinical Diagnosis • Histologic Diagnosis • Clinicopathologic Correlation General Principles of Management CAUSES OF ESRD IN THE PHILIPPINES: Renal Registry Data, PSN, 2003 Cause/Etiology (%) ESRD Cases Diabetes mellitus 33 Glomerulonephritis 25 Hypertension 19 Afferent arteriole Parietal EC Capillary loop Endothelium Macula densa Mesangium JG cells Urinary space Efferent arteriole Visceral EC Mesangium Normal Glomerulus Normal glomerulus PATHOLOGY Definition of Terms • Glomerulopathy vs. Glomerulonephritis • Primary vs. Secondary • Diffuse vs. Focal • Global vs. Segmental • Fibrosis vs. Sclerosis • Membranous vs. Proliferative • Endocapillary vs. Extracapillary Fibrosis – increase in the deposition of collagen fibers Sclerosis – increase in the amount of homogenous nonfibrillar extracellular material Sclerosis Segmental – lesion involves < 50% of the glomerulus Sclerosis Global – lesion involves > 50% of the glomerulus Sclerosis Diffuse Global Glomerulosclerosis Focal – lesion seen in less than 50% of glomeruli Diffuse – lesion seen in more than 50% of glomeruli Mesangial cells Normal glomerulus Proliferation – increase in the glomerular cell number Mesangial cells Mesangial proliferativeGN Endocapillary proliferation Extracapillary proliferation Normal glomerulus Membranous – expansion and thickening of the glomerular basement membrane (GBM) by immune deposits Primary Mechanisms of Glomerular Injury Mechanism of Injury Renal Insults/ Defects Glomerular Disease Immunologic Immunoglobulin Immune-complex GN Cell-mediated injury Pauci-immune GN Cytokine Primary FSGS Complement activation MPGN Type II Hyperglycemia DM Nephropathy Fabry’s disease/ sialidosis FSGS Metabolic Hemodynamic Systemic hypertension Intraglomerular hypertension HTN Nephrosclerosis Secondary FSGS Primary Mechanisms of Glomerular Injury Mechanism Renal Insults/ Defects of Injury Glomerular Disease Toxic E. coli-derived verotoxin Thrombotic microangiopathy Therapeutic drugs (NSAIDs) Minimal change disease Recreational Drugs (Heroin) FSGS Deposition Amyloid fibrils Amyloid nephropathy Infectious HIV HIV Nephropathy Subacute Endocarditis Immune complex GN Inherited Genetic defect for 5 chain of Alport’s Syndrome type IV collagen Abnormally thin basement membrane Thin basement membrane disease Immunologic Glomerular Injury Humoral Antibody-Mediated Injury • Autoantibodies against intrinsic antigens (example: Goodpasture’s syndrome) • Autoantibodies against extrinsic “trapped antigens (example: Postinfectious GN) • Trapping of circulating immune complexes (example: Cryoglobulinemic GN) Cellular Mediated Injury GN Loss of nephrons Glomerular hyperfiltration Glomerular HTN Non-selective prtoteinuria Glomerular sclerosis Tubulointerstitial inflammation Ischemia Tubulointerstitial atrophy/fibrosis Two Final Common Pathways in Glomerular Injury OBJECTIVES Introduction Approach to Glomerular Diseases • Syndrome Diagnosis • Clinical Diagnosis • Histologic Diagnosis • Clinicopathologic Correlation General Principles of Management Approach to Glomerular Diseases • • • • Syndrome Diagnosis Clinical Diagnosis Histologic Diagnosis Clinicopathologic Correlation Syndrome Diagnosis History Physical Examination Ancillary Laboratory Tests • Chemistry • Serology • Urinalysis Syndromes in Glomerular Diseases Syndrome Clues to Diagnosis Common Findings Rapidly Progressive Renal Failure (RPRF) Anuria Oliguria Decline in GFR over weeks Hematuria, RBC casts, Azotemia, Oliguria, Edema, HTN HTN, Hematuria, Proteinuria, Pyuria Nephritic Syndrome Proteinuria, Syndromes in Glomerular Diseases Syndrome Clues to Diagnosis Common Findings Nephrotic Syndrome Proteinuria > 3.5 gms Hypoalbuminemia Hyperlipidemia Lipiduria Casts Edema Asymptomatic Isolated hematuria urinary Isolated proteinuria abnormality (AUA) Approach to Glomerular Diseases • • • • Syndrome Diagnosis Clinical Diagnosis Histologic Diagnosis Clinicopathologic Correlation C-ANCA: Cytoplasmic Antineutrophil Cytoplasmic Antibodies C-ANCA •Antibodies against Proteinase 3 •Associated with Wegener’s ggranulomatosis P-ANCA: Perinuclear Antineutrophil Cytoplasmic Antibody P-ANCA •Antibodies against myeloperoxidase •Associated with a variety of vasculitides •Non-specific for Wegener’s granulomatosis Clinical Diagnosis Disease Renal Syndrome Clinical Features Diabetic nephropathy Nephrotic CRF Chronic course, (+) DM retinopathy, nl-sized kidneys, bland urine sediment Goodpasture’s syndrome Nephritic RPRF antiGBM-aby (+), cANCA (-), nl C3 Wegener’s Nephritic granulomatosis RPRF antiGBM-aby (-), cANCA (+), nl C3 Clinical Diagnosis Disease Renal Clinical Features Syndrome Lupus nephritis Nephritis RPRF antiGBM-aby (-), cANCA (-), low C3, ANA (+), (+) ACR criteria for the diagnosis of SLE Poststreptococcal Nephritis GN antiGBM-aby (-), cANCA (-), low C3, ASO (+), prior Streptococcal infection Approach to Glomerular Diseases • • • • Syndrome Diagnosis Clinical Diagnosis Histologic Diagnosis Clinicopathologic Correlation Indications for a Kidney Biopsy • Unexplained ARF • Unexplained RPRF • Adult nephrotic syndrome w/out systemic disease • Proteinuria < 2 g/d w/ deterioration of renal function • Proteinuria > 2 g/d • DM w/ acute onset of proteinuria and renal failure • DM with proteinuria but w/out retinopathy • Selected cases of Lupus nephritis Crescent Membrane thickening Mesangial expansion Cellular proliferation MPGN Deposits Splitting MPGN Normal glomerulus Fusion of foot processes Minimal Change Disease Sclerosis FSGS Foot process fusion FSGS Membranous Nephropathy Deposits Membranous GN Mesangial proliferation Mesangial IgA Deposits IgA Nephritis Approach to Glomerular Diseases • • • • Syndrome Diagnosis Clinical Diagnosis Histologic Diagnosis Clinicopathologic Correlation Clinicopathologic Correlation Syndrome Diagnosis Histologic Diagnosis Etiologic Diagnosis Nephritic Diffuse Immune complex GN (>70%)* Proliferative GN Pauci-immune GN (<30%)** Nephritic Nephrotic MembranoImmune complex GN* Proliferative GN Thrombotic microangiopathy RPRF Crescentic GN Isolated hematuria Mesangial IgA nephropathy Proliferative GN HSP Immune complex GN (45%)* Pauci-immune GN (45%)** Anti-GBM disease (10%) * SLE, Postinfectious GN, IE, Cryoglobulinemia ** Wegener’s granulomatosis, Microscopic PAN Clinicopathologic Correlation Syndrome Histologic Diagnosis Diagnosis Etiologic Diagnosis Nephrotic Minimal Change Disease (MCD) Idiopathic, drugs, heroin, HIV, lymphoma Nephrotic Focal Segmental Glomerulosclerosis (FSGS) Idiopathic, HIV, heroin, secondary forms from reduced nephron number Nephrotic Membranous Glomerulopathy Idiopathic, infections, drugs, autoimmune diseases, paraneoplastic syndrome Nephrotic CRF Nodular sclerosis DM nephropathy Chronic GN Wire Loop Cellular proliferation Lupus nephritis TRI Lupus Nephritis Postinfectious GN Postinfectious GN DM Nephropathy Collapsing FSGS Sclerosis Tubuloreticular Inclusion bodies Amyloid SAMPLE CASE • 28 year old female referred for acute onset of pedal edema X 1 week • No other associated signs and symptoms • Single; sexually active; silent past medical history; not on any medications; no history of IVDA • ROS: denies other symptoms • Well-nourished, not obese • BP = 120/80, clear BS • Grade III pedal edema SAMPLE CASE • Serum creatinine = 0.7 mg/dl (nl) • Albumin = 2 g/L (low); Cholesterol = 300 mg/dl (high); FBS = 100 mg/dl (nl) • CXR: normal; UTS of kidneys: normal • Urinalysis: +4 protein, 0-1 RBC/hpf, 0-1 WBC/hpf, no casts • 24-hour urine study: creatinine clearance of 98 cc/min and proteinuria of 4.5 g/day Approach to Glomerular Diseases • • • • Syndrome Diagnosis Clinical Diagnosis Histologic Diagnosis Clinicopathologic Correlation SAMPLE CASE What is the renal syndrome present? • Nephritic syndrome • Nephrotic Syndrome • Rapidly progressive renal failure • Asymptomaric urinary abnormality SAMPLE CASE Answer: Nephrotic syndrome • Edema • Hypoalbuminemia • Hyperlipidemia • Proteinuria > 3.5 g/day Approach to Glomerular Diseases • • • • Syndrome Diagnosis Clinical Diagnosis Histologic Diagnosis Clinicopathologic Correlation SAMPLE CASE Is it possible to make a clinical diagnosis? • Yes or No ? • If yes, what is your clinical diagnosis? • If no, is a kidney biopsy indicated? SAMPLE CASE Answer: No • No signs of systemic disease, ROS negative for other symptoms • PE normal except for edema • Normal FBS • Adult nephrotic syndrome – unlike children, no room for empiric steroid therapy • Kidney biopsy indicated Approach to Glomerular Diseases • • • • Syndrome Diagnosis Clinical Diagnosis Histologic Diagnosis Clinicopathologic Correlation Sclerosis Foot process fusion SAMPLE CASE Histologic Diagnosis: • Focal segmental glomerulosclerosis Approach to Glomerular Diseases • • • • Syndrome Diagnosis Clinical Diagnosis Histologic Diagnosis Clinicopathologic Correlation SAMPLE CASE • What are the possible causes of FSGS? • What additional test/s is/are needed? • Is this primary vs. secondary FSGS? Etiology of FSGS Idiopathic (Majority) Systemic Diseases or Drugs • HIV • Diabetes mellitus • Fabry’s disease • Sialidosis • Charcot Marie-Tooth Disease • Heroin Etiology of FSGS Congenital Oligonephropathies Acquired nephron loss • Surgical resection • Reflux nephropathy • Chronic GN/ renal disease Other adaptive responses • Sickle-cell nephropathy • Obesity with sleep apnea • Familial dysautonomia SAMPLE CASE • No signs of systemic diseases • No history or sign (normal kidneys on UTS) of nephron loss • Not obese • No history of IVDA/ heroin use • Sexually active – need to rule out HIV • HIV ELISA test ordered – negative • Final diagnosis: Idiopathic Primary FSGS OBJECTIVES Introduction Approach to Glomerular Diseases • Syndrome Diagnosis • Clinical Diagnosis • Histologic Diagnosis • Clinicopathologic Correlation General Principles of Management General Principles of Management • Disease-specific therapy for primary and secondary GN • Therapy to retard the progression of disease • Therapy to address complications Disease-specific therapy GN Loss of nephrons Glomerular hyperfiltration Glomerular HTN Non-selective prtoteinuria Glomerular sclerosis Tubulointerstitial inflammation Ischemia Tubulointerstitial atrophy/fibrosis Two Final Common Pathways in Glomerular Injury Disease-Specific Therapy for Primary (Idiopathic) GN Syndrome Disease Therapy Nephritic MPGN Aspirin plus dipyridamole Nephrotic MCD Steroids Nephrotic FSGS Steroids Nephrotic Membranous Steroids plus chlorambucil (Ponticelli protocol) Disease-Specific Therapy for Secondary GN Syndrome Disease Therapy Nephritic Poststreptococcal GN Penicillin; supportive RPRF Wegener’s granulomatosis Steroids plus PO cyclophosphamide RPRF Goodpasture’s syndrome Plasmapharesis Nephritic Lupus nephritis IV Steroids, IV cyclophosphamide Nephrotic Hep B membranous GN Interferon Nephrotic MCD due to NSAIDs Discontinue offending drug GN Loss of nephrons Glomerular hyperfiltration Measures to delay progression Glomerular HTN Non-selective prtoteinuria Glomerular sclerosis Tubulointerstitial inflammation Ischemia Tubulointerstitial atrophy/fibrosis Two Final Common Pathways in Glomerular Injury Renoprotective Strategies (Hebert, 2000) • • • • • • Control blood pressure (< 127/75). (1) Use of ACE-I for BP. (1) Control of blood glucose for diabetics.(1) Limit protein intake to 0.8 g/kg IBW/day.(1) Limit NaCl intake (2-3 g/day).(3) Control lipids using statins (HMG-CoA reductase inhibitor therapy). (2) • Avoid cigarette smoking. (2) • Avoid regular intake of NSAIDs.(3) ( ) Level of Recommendation Renoprotective Strategies (Hebert, 2000) • Control plasma homocysteine level using folic acid (2-15 mg/d). (3) • Control hyperinsulinemia (exercise and weight reduction). (3) • Use of antioxidants (Vit C and Vit E). (3) • Correct anemia (HgB 11-12). (2) • Avoid hypokalemia. (3) • Control hyperphosphatemia. (3) • Low dose ASA. (3) • Estrogen replacement for women. (3) ( ) Level of Recommendation Treatment of Complications • Diuretics to control edema. • ACE-I/AII-RBs to control BP. • Anticoagulants (warfarin) for hypercoagulable states. • Statins for hyperlipidemia • Measures to prevent osteoporosis for patients on steroids (Calcium, Vit D, biphosphonates). • Co-trimoxazole to prevent Pneumocystic pneumonia for patients on steroids SUMMARY Introduction Approach to Glomerular Diseases • Syndrome Diagnosis • Clinical Diagnosis • Histologic Diagnosis • Clinicopathologic Correlation General Principles of Management HUS Thrombi DM Nephropathy DM Nephropathy Membranous GN (Silver stain) Spikes Immunofluoresence- Membranous GN Mesangial proliferation Lupus Nephritis Lupus Nephritis Membrane thickening TRI Membranous Lupus GN Immunofluorescence- Postinfectious GN RPGN Immunofluoresence: Anti-GBM Disease