Controversies in Heart Failure
Management
M.Birhan YILMAZ, MD, FESC
Cumhuriyet University School of Medicine
Department of Cardiology, Sivas, TURKEY
Heart Failure
-2% of the population,
->10% over 70 years
- no “healing”, irreversible
-high mortality,
-frequent rehospitalizations
- Extremely costly (in terms of hospitalization
and currently device related)
Potential areas of controversy
•
•
•
•
•
•
•
•
Diagnosis
Life style
Device related
HR reduction
Anticoagulation
Revascularization
Inotrope
AHF
Increased sensitivity at a cost of
compromised specificity
Diagnostic Controversy
The diagnosis of HF-PEF remains a particular challenge,
and the optimum approach incorporating symptoms, signs,
imaging, biomarkers, and other investigations is uncertain.
*Different disease or a
different phase of the
same disease spectrum
*Diastolic stress test
‘Artificial’ recommendations
ESC confessed
decided that the guidelines for HF probably
had been artificially giving recommendations for
lifestyle advice really on the basis of no good
evidence.
The exceptions, both class IA recommendations:
"Regular aerobic exercise is encouraged in patients
with heart failure to improve functional capacity and
symptoms," and patients are advised to enroll in a
"multidisciplinary-care management program" to
lower the risk of heart-failure hospitalization.
How much of salt?
Heart Failure Therapy
Post-MI
LV dysfunction
AIRE/SAVE
(ramipril/captopril)
Mild
CHF
Moderate
CHF
SOLVD Treatment
(enalapril)
CHARM/Val-HeFT
(candesartan/valsartan)
Severe
CHF
CONSENSUS
(enalapril)
US Carvedilol/MERIT/CIBIS
COPERNICUS
CAPRICORN
(carvedilol) (carvedilol/metoprolol/bisoprolol) (carvedilol)
EPHESUS
(eplerenone)
MADIT, MUSTT
(ICD)
EMPHASIS-HF
(eplerenone)
SCD-HeFT, MADIT-II
(ICD)
RALES
(spironolactone)
MIRACLE, COMPANION,
MUSTIC (CRT +/- ICD)
CARE-HF
Solved Controversy
Device Related Controversies
Randomized Controlled Trials on
Resynchronization therapy
•
•
•
•
•
•
•
•
•
•
MIRACLE
MUSTIC SR
MUSTIC AF
PATH CHF
MIRACLE ICD
CONTAC CD
COMPANION
PATH CHF II
MIRACLE ICD II
CARE HF
RAFT
CRT Improves
NYHA Class,
Quality of life score,
Exercise Capacity,
LV function,
Reverse remodeling,
Hospitalization,
Mortality
CRT in patient with Atrial
fibrillation
• 1/3 of the patients with HF are in AF
• 1/5 of the patients receiving CRT in
Europe
• Older, more co-morbidities, worse
prognosis
HF and AF
Prevalence by NYHA class
50%
45%
40%
35%
30%
50%
NYHA II
NYHA III
25%
20%
NYHA IV
15%
25%
10%
5%
NYHA I
10%
5%
0%
Atrial fibrillation (% )
Why does AF matter when
selecting for CRT?
• Loss of AF synchrony
• AV optimization not possible
• Excessive intrinsic ventricular rate
• High pacing rates needed to provide
biventricular capture, if possible at all!
How to improve CRT benefit on
AF patients
• Complete ventricular capture (>95%
pacing)- is mandatory in order to
maximize clinical benefit and improve
the prognosis
– Pharmacological therapy to slow ventricular
rate
– Ablation of AVN
– Pulmonary vein isolation
CRT-P versus CRT-D
• CRT-D is associated with
more device-related
complications (up to 10%)
Inappropriate shocks
CRT and reverse remodeling
Remodeling and arrhythmias
REVERSE
CRT –ON doesn’t
increase VT/VF
episodes
Remodeling is
associated with less
VT/VF episodes
CRT-P versus CRT-D
• The group of patients that benefit most is
the one with QRS ≥ 150 ms
• Anyone who undergoes CRT for the most
part is also indicated for an ICD if you look
at the crossover.
• So, why use a CRT-P?
Why use a CRT-P?
• People may like, at least in Europe, to see or
pursue a therapy that is less expensive,
compared with CRT-D, but that provided the
same quality of life as CRT-D
• Choice of a patient – “If I die suddenly, I die
suddenly, but I really don't like the shortness of
breath."
• Remember the 10% of complications,
inappropriate shocks
Electricity in HF -charged
with sex discrimination
• CRT benefit favors women: MADITCRT
• Women with ICD get fewer shocks
• Women have better heart-failure
survival than men
MADIT-CRT -CRT benefit
favors women
End point
Women, n=453
Men, n=1365
Death or heart failure
0.31 (0.19-0.50), p<0.001
0.72 (0.57-0.92), p<0.01
Heart failure
0.30 (0.18-0.50), p<0.001
0.65 (0.50-0.84), p=0.001
Death
0.28 (0.10-0.79), p=0.02
1.05 (0.70-1.57), p=0.83
• 69% plunge in rate of death or heart failure in women
(p<0.001) far exceeded the 28% reduction (p<0.01) in
men.
• associated with consistently greater echocardiographic
evidence of reverse cardiac remodeling in women than
in men
Women have better heart-failure
survival than men MAGGIC study
Women with heart
failure have
better survival
than man,
irrespective of
age, etiology and
EF (patient data
from 31 studies in
41 949 patients ).
CRT controversy
Patients with NYHA Class III or ambulatory IV
Patients with NYHA Class II
Device with Huge Controversy
Does lowering heart rate improve
clinical outcomes in chronic HF?
• Systematic reviews have demonstrated that a
major contributor to the benefits of -blocker therapy
may be their rate-lowering effect – but they are
generally underused or underdosed!
• When ivabradine does become available, the
results of SHIFT will likely support the use of
ivabradine in patients with moderate to severe HF
on optimum medical therapy including -blockade
with LVEF 35% and resting heart rate 70 bpm.
HR reduction controversy
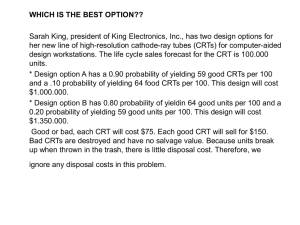
Anticoagulate in Heart Failure Do We Have an Answer?
• Warfarin vs Aspirin in Reduced Cardiac
Ejection Fraction (WARCEF trial)
Primary end point
Aspirin, n
(%/y)
Warfarin, n
(%/y)
Hazard ratio
(95% CI)
p
Death, ischemic stroke or
intracerebral hemorrhage
320 (7.93)
302 (7.47)
0.93 (0.79-1.10)
0.40
No significant difference seen in the primary end point between groups
-no difference in death rates between groups,
-intracerebral hemorrhage was very infrequent in both groups
-highly significant reduction in ischemic stroke among those on warfarin vs aspirin.
-Major hemorrhage was significantly higher with warfarin (GIT bleeding),
-no significant differences in intracerebral or intracranial hemorrhage
Anticoagulation in HF
• ASPIRIN - safer to use, easier to use,
patients tolerate it pretty well, there are no
food interactions, and it's inexpensive
• Newer oral anticoagulants now becoming
available—dabigatran and rivaroxaban, which
are already approved, and apixaban, which is
expected to be approved soon—might reopen
this question.
• However, it is important to keep in mind that
eGFR<30 ml/kg/min is a frequent exclusion
(though it is common in HF)
• Thrombo-embolism prophylaxis in patients with HF
and AF should be based on CHA2DS2-VASc
score Most patients with systolic HF will have a risk
score consistent with a firm indication for (score
≥2), or preference for, an oral anticoagulant (score
≥ 1), although bleeding risk must also be
considered
• Some new anticoagulant drugs such as the oral
direct thrombin inhibitors and oral factor Xa
inhibitors are contraindicated in severe renal
impairment (creatinine clearance ,30 mL/min).
Rate or Rhythm Control in HF-AF
• In patients with chronic HF, a rhythm-control strategy
including
• pharmacological or electrical cardioversion has not been
demonstrated
• to be superior to a rate-control strategy in reducing
mortality or morbidity.
Revascularization Controversy in HF
• STICH viability arm failed to
show any benefit of viability
testing (?)
Inotrope Controversy
• Dobutamine, Dopamine, Adrenaline, Levosimendan,
Omecamtiv mecarbil (cardiac myosin activator) etc….
• Several studies with controversial or neutral results
(even detrimental)
Controversies for VADs
VADs and biventricular
assist devices (bi-VADS)
received a class I level B
recommendation for use as
a bridge to heart
transplantation,
but a class IIa level B
"should be considered"
endorsement as
destination therapy in
'highly-selected patients'
Acute HF
Land of
Controversies