ChemoRadCervix
Mary McCormack & Jonathan Ledermann
NCRI Gynae Clinical Studies Group
CRT standard of care for the past decade
Meta- analysis 18 RCT in CRT (Vale et al
2008)
-absolute survival benefit of 6% at 5 years
- all groups benefitted
7-10% stage I-II
3% stage III-IV
Overall survival with CRT 66% at 5years (Vale
2008) –
but DFS only 58%
However – in those with : positive LN large volume tumours advanced stage outcome remains poor
Downstage
Eradicate micrometastases
Impact on survival ?
Chemotherapy : short cycle interval
7% improvement in 5 year OS
(Tierney 2003)
Phase II single arm NCRI feasability study
Aim to assess
response rate
and
toxicity
of a
short course of dose dense weekly chemotherapy
prior to definitive chemoradiation in women with LACC
Dose dense schedulesenhanced cell kill ?
overcome accelerated repopulation ?
Greater dose intensity (v q 3-weekly)
Well tolerated in head & neck / ovarian cancer patients
Histologically confirmed FIGO stage Ib2- IVa
(
Squamous, Adenocarcinoma, Adenosquamous)
PS 0,1
Age >18,no upper limit providing deemed fit to receive CRT
Adequate renal,liver,BM function,normal ECG
Informed consen t
Weekly Paclitaxel (80mg/m 2 )
& Weeks 1-6
Carboplatin (AUC2)
Followed by radical ChemoRT Weeks 7-13
(cisplatin 40 mg/m 2 )
50 patients with LACC- (80% power , one sided test at 5% level to detect a response rate of at least 85%)
Toxicity rate >20% - trial to be stopped
46 patients recruited from 3 centres
Median age 43 (range 23-71)
Histology -72% SCC
-22% Adeno
- 6% Adenosq
FIGO stage
IB2 - 11%
II - 50% ( 3/23 +PALN)
III - 33% (3/15 +PALN)
Iva - 6%
NACT CRT
G3/4 Haematological
11%
G3/4 Non-haem tox –
11%
G3/4 Haematological
45%
G3/4 Non- haem tox
21%
96% (44/46 ) completed RT without delay
96% (42/44) completed brachytherapy
78% (36/46) had minimum 4 cycles weekly cisplatin
44 pts assessable for response
CR/PR - Post NACT 68% [95% CI 52-81%]
-12 Weeks post CRT 82% [95% CI 67-92%]
Positive PALN 6 pts- 5 completed all treatment
4/5 NED
Dose dense NACT with weekly C&P followed by radical CRT is feasible with acceptable toxicity
High response rate (68%) to short course of induction chemotherapy
NACT did not result in any disruption to CRT
89% completed CRT within 50 days and 78% completed at least 4 cycles of cisplatin
Survival at 2 years is 79%
(median FU 23.2 months)
This approach merits further investigation in a randomised phase 3 trial
Induction chemo (6 weeks) + CRT
FIGO 1B2- IVA
CRT alone
Include all those suitable & fit for CRT
Stratify according to node status
Stratify according to RT dose / institution
Record tumour vol in addition to FIGO stage
Collection of tissue for translational research
Substudy of functional imaging to assess response to IC - ?DCE- MRI
QOL assessment
Primary endpoint OS at 5 years
Secondary endpoints-
PFS
Toxicity
QOL
Pattern relapse
Relationship between functional imaging and outcome
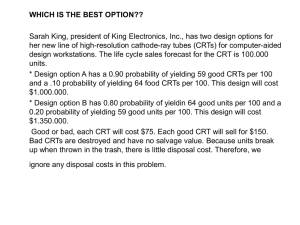
Sample size of 1100 provide 80% power to detect a 7% increase in 5 year OS ( 66 to 73%)
(HR 0.75 , 2 sided test at 5% level)
Assumes accrual over 4 years with 4 years FU
Upfront chemotherapy
Short course 6 weeks
Minimal toxicity
No disruption to CRT
Overall treatment time
13 weeks
Outback chemotherapy
4 cycles q3weeks
Haem/GI tox likely to be significant
Compliance likely to be poor
Overall treatment time
20 weeks
differences in expertise –radiology/ nodal staging
variations in RT dose & fractitionation
quality assurance for RT etc
Potential difficulties in delivering a protracted course of treatment & in FU
These need to be addressed as the participation of colleagues in developing world & Eastern Europe is essential