Newburger sickle
advertisement
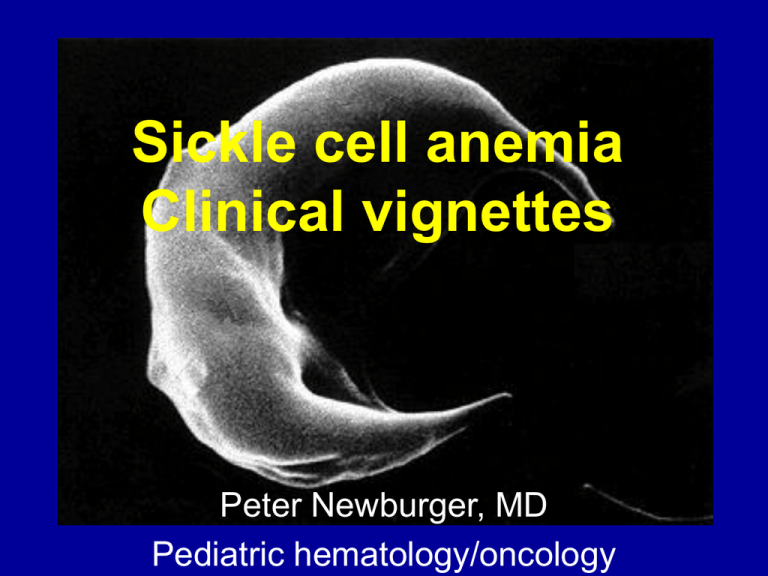
Sickle cell anemia Clinical vignettes Peter Newburger, MD Pediatric hematology/oncology Sickle cell anemia From http://fig.cox.miami.edu/~cmallery/150/gene/mol_gen.htm Sickle Cell Epidemiology bS : Single a.a. substitution Glutamic acid Valine Most common single gene disorder in African Americans 1/375 affected (homozygous) 1/12 are heterozygous carriers (~8%) Also affects other ethnicities: India, Middle East, Hispanic SICKLE CELL SYNDROMES • Molecular pathology postulated by Pauling in the late 1940s • Mutation known for 50 years • Unfinished tasks – Explaining the clinical disorder based on the molecular defect – Rational and targeted treatments – still few despite detailed knowledge of the molecular defect Molecular Pathophysiology Intracellular [Hb] ~30 - 35 g/dL Deoxygenation allows interaction of bS subunits via abnormal hydrophobic regions (valines) Non-covalent bond with other bS in the RBC Formation of 14 stranded helical fiber Delay time ≈ k / C15 The time that elapses between the deoxygenation of hemoglobin S and the formation of polymer is inversely proportional to the intracellular concentration (C) of deoxyhemoglobin, raised to the 15th power Polymerization phase is sensitive to: • O2 concentration • Hgb concentration • pH • Ionic strength (At salt concentrations spanning the physiologic range, solubility increases with ionic strength, but decreases markedly at high ionic strength.) Bunn HF. NEJM 1997 337 (11) Cellular Pathophysiology of Sickle Cell syndromes Polymerization leads to: Distortion of Cell shape Damage to RBC Membrane Abnormal permeability Irreversible sickling Impairment of RBC flow = Infarction Decreased red cell number = Anemia Anemia • • • • • Most common feature of sickle cell disease Often ignored as pathologic Moderate to severe in almost all patients Degree of anemia reflects clinical severity Episodic acute anemia Sickle complications • Vaso-occlusive crisis • Cerebrovascular disease • Splenic sequestration • Sepsis due to functional asplenia • Acute chest syndrome Patient vignettes 18 month old girl presents to the ER crying inconsolably, with fever and swollen, tender hands. A 3 year old boy presents to the ER with a 12-hour history of fever to 38°C. He is slightly irritable but looks well. Despite IV antiobiotics, his fever continues to rise, his blood pressure falls, and his extremities become cold, with purple discoloration. Functional asplenia Functional Asplenia Sepsis Prevention: the most effective drug for sickle cell is… Volume 314:1593-1599. June 19, 1986. Number 25 Prophylaxis with oral penicillin in children with sickle cell anemia. A randomized trial MH Gaston, JI Verter, G Woods, C Pegelow, J Kelleher, G Presbury, H Zarkowsky, E Vichinsky, R Iyer, JS Lobel, and et al. PROPS I Prophylactic Penicillin Study Multicenter randomized double-blind placebo-controlled trial “Prophylactic therapy with oral penicillin by four months of age decreases the morbidity and mortality associated with pneumococcal septicemia.” Vaccination: Important for adult sickle cell and all splenectomized patients!! “Catch-up” vaccination if Prevnar series not complete A fourteen year old girl with sickle cell disease comes to clinic because her left side is weak. She is immediately transferred to the ICU for exchange transfusion. CT scan of stoke Cerebral blood vessels Sickle Cell Disease: Cross Section of Internal Carotid Artery Intimal hyperplasia Normal Age at 1st stoke in sickle syndromes Stroke Prevention Most clinical strokes occur in children with increased cerebral blood vessel flow velocities Flow measured by transcranial Doppler ultrasound STOP Trial - red cell transfusions reduce the risk of stroke in children with TCD > 200 cm/sec Transcranial Doppler U/S Long term treatment of sickle cell disease • Hydroxyurea • Hematopoietic stem cell transplantation • Gene therapy Hydroxyurea Hydroxyurea decreases crises in patients with severe sickle cell disease. In 299 adults with severe sickle cell anemia: • Hydroxyurea provided ~50% decrease in: – frequency of hospitalization – incidence of pain, acute chest syndrome, and blood transfusions • In good responders: – – – – hemolysis and leukocyte counts fell hemoglobin concentrations increased Hb F increased from 5 % to 9% overall Hb F increased to 18 % in top quartile of responders N Engl J Med 1995;332:1317-22 Stem Cell Transplantation – Stroke risk – Acute chest syndrome risk – Inexorable accrual of chronic end organ damage (including CHF, pulmonary hypertension, iron overload) Complications of sickle cell – Transplant-related mortality – Infertility – Secondary malignancy – Graft vs. host disease Complications of transplantation Gene therapy Ely and Rainer NEJM 1997;336:1364