Biliary disease + Pancreatitis
advertisement
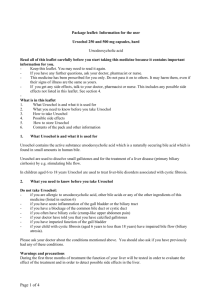
Biliary disease + pancreatitis for finals (and beyond) …the story of Mrs Harvey-Henry Dr Julian Dickmann General Surgery By the end of this session… You will be able - To recognise the common complications of gallstone disease - Understand the underlying pathophysiology - Start initial management and investigations - To initiate treatment. First doctor You are the F2 in general practice – Mrs HarveyHenry, a 44 year old restaurant critic comes to you with her private ultrasound report after a visit to the well woman clinic which showed “numerous gallstones”. She does not complain of any symptoms. She is very worried – what do you advise? Gallstones The commonest cause of emergency hospital admission with abdominal pain1 = common in exams 1- Kettunen et al. Emergency abdominal surgery in the elderly. Hepatogastroenterology. 1995;42:106–8. Pictures from BMJ Review (Gallstones) “Pathological” effects of gallstones WITHIN THE GALLBLADDER Silent 90% asymptomatic Second doctor You are the F1 in A+E – Mrs Harvey-Henry, presents to the emergency department with a 1h history of RUQ pain after dining at the Fat Duck. The pain has now subsided and she is very worried. What do you advise (examination unremarkable)? “Pathological” effects of gallstones WITHIN THE GALLBLADDER Biliary colic INTERMITTENT PAIN NOT SYSTEMICALLY UNWELL Biliary colic Clinical management & investigations Do not admit. Ultrasound as an outpatient. • Conservative – Analgesia – Anti-emetics • Medical – Ursodesoxycholic acid (not effective) • Surgical – Cholecystectomy (laparoscopic) Third doctor You are the F1 in A+E – Mrs Harvey-Henry, now complains of a 2 day history of RUQ pain, vomiting and feeling unwell. “Pathological” effects of gallstones WITHIN THE GALLBLADDER Acute cholecystitis Acute cholecystitis – pathogenesis obstruction of the cystic duct (gallstones / sludge) ↑ Intraluminal pressure supersaturation of cholesterol Inflammatory response (PG-I2/E2) ± secondary bacterial infection (E Coli, Klebsiella) in 20% Acute cholecystitis – diagnosis Murphy’s sign positive: inspiratory arrest by pain on palpation AND the absence of left sided arrest of inspiration Acute cholecystitis – investigations Blood tests Ultrasound Distended “thick walled” gallbladder Gallstones / Sludge Murphy’s sign – elicited with probe CT (CXR) Δ RLL Pneumonia Preparation for ultrasound abdomen: Fasting for 6h. Clear fluids until 2h. (+ full bladder for renal/gynae) Acute cholecystitis – management II • Conservative – Analgesia – Anti-emetics • Medical – IV Antibiotics (Tazocin ± Gentamicin) • Surgical – definite treatment – Laparoscopic / open cholecystectomy – High surgical risk + sepsis: percutaneous cholecystostomy Acute cholecystitis – management I Timing of surgery? 28.5% readmission rate (gallstone-related complications) on NHS waiting list (1) Either: Early urgent (<72h) or delayed-interval LC – Introduction of an “urgent cholecystectomy service” of readmission rate 19% to 3.6% (2) – Optimal time: 6-12 weeks after initial admission (3) (1) Cheruvu et al. Ann R Coll Surg Engl 2002 (2) Mercer et al. Br J Surg 2004 (3) Gurusamy et al. Br J Surg. 2010 Complications • Anaesthetic risk (PE, Pneunomia, MI) • Procedure-specific risks: – Conversion to open – Injury to CBD – Biliary leak causing biliary peritonitis – Post-op haemorrhage – Intra-abdominal abscess 4th doctor Mrs Harvey-Henry responds well to analgesia and antibiotics but a day you as the F1 notice that she is appears jaundiced (obviously you noticed this without looking at the bilirubin…). “Pathological” effects of gallstones Obstructive jaundice Oedema around the biliary tract Choledocolithiasis =stone in CBD Mirizzi’s syndrome (stone in Hartmann’s pouch compressing common hepatic duct) Choledocolithiasis Suspect if: JAUNDICE ± deranged liver function ± dilated CBD Management 1st – MRCP 2nd – Endoscopic retrograde cholangiopancreatography (ERCP) NB: no diagnostic test, treatment only (>90% success rate) (operative CBD exploration during cholecystecomy) Normal CBD diameter < 50 years – 6mm > 50 years – 8mm post-cholecystectomy >10mm Senturk et al. Eur J Radiol. 2012 Jan;81(1):39-42. 5th doctor On your on-call night shift, the a nurse on Willoughby ward bleeps you: Mrs HarveyHenry’s MEWS is 8 (systolic BP of 85, HR 120, RR 24, T 39.2). They are apologetic, but as she was in a side-room, they only noticed this at midnight. So you make your way up to the ward… Ascending cholangitis Bacterial infection (E. Coli) of the biliary tree Management: IV Fluids, Abx + urgent removal of obstruction (ERCP) 6th doctor Mrs Harvey-Henry is successfully resuscitated by yourself (ABC!) and there was a slot for an ERCP available first thing in the morning. Anything to consider? 7th doctor You get bleeped at 11pm. The nurses tell you that Mrs Harvey Henry needs more pain relief. Her pain is not adequately controlled on paracetamol, tramadol and hourly oramorph. Could you come and assess her? post-ERCP Pancreatis (PEP) 5% risk esp. multiple injections of contrast into pancreatic duct Acute Pancreatitis Pain severe epigastric central abdominal radiation to the back Aetiology Gallstones (50%) Alcohol (35%) Post-ERCP (5%) (the rest = 5%) Vomiting 8th doctor Your SHO and registrar are busy in theatres. You are on your own. Start initial investigations and management. Management • • • • Nil by mouth IV Access (green cannula) Bloods – FBC/U+Es/Amylase/CRP/G+S/Clotting For ANY surgical admission Aggressive fluid replacement – 1000ml Hartmann’s stat – 1000ml Hartmann’s 2h / 4h / 6h • • • • Catheterise – strict fluid balance Hourly observations Analgesia ABG ABGs… Investigations Modified Glasgow criteria – prognostic criteria Predicts severity of severe pancreatitis: ≥3 factors are over the first 48h indicate severe pancreatitis ITU involvement PaO2 <8kPA [ARDS] Age >55y Neutrophils WBC>15 Calcium <2mmol/l [lipid saponification] Renal functionUrea >16 [hypovoloaemia] Enzymes LDH >600, AST>200 [autolysis] Albumin <32g Sugar BM >10mmol/l [endocrine disturbance] LOOK FOR SIGNS OF (MULTI-) ORGAN FAILURE Questions? Covered in the handout: – Biliary malignancies (cholangiocarcinoma) – Chronic pancreatitis