56_eposter - Stanley Radiology
advertisement
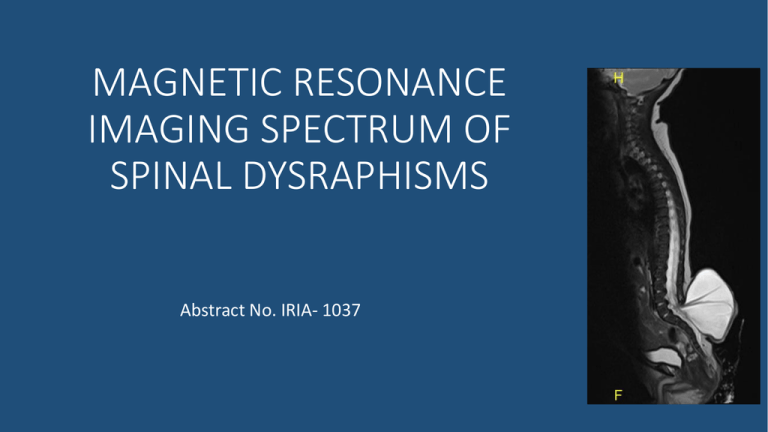
MAGNETIC RESONANCE IMAGING SPECTRUM OF SPINAL DYSRAPHISMS Abstract No. IRIA- 1037 INTRODUCTION MRI plays an important role in characterising spinal dysraphisms because of excellent soft tissue contrast and the ability to detect fat in the lesion. T2 weighted images provide excellent contrast between the subarachnoid spaces and neural tissue while evaluating spinal dysraphisms. AIM • To study the MRI characteristics of spinal dysraphisms and to categorize the lesions using non-contrast enhanced Magnetic resonance imaging. 2 MRI MATERIALS AND METHODS 3 14 2 had only simple skin dimple SPINAL DYSRAPHISM ON MRI CLOSED 11 RESULTS CLINICAL SUSPICION OF SPINAL DYSRAPHISM 12 OPEN 1 MENINGOMYELOCELE SUBCUTANEOUS MASS PRESENT ABSENT 2 2 LIPOMYELOCELES 1 LIPOMENINGOMYELOCELE DISORDER OF SECONDARY NEURULATION 1 INTRADURAL LIPOMA 1 FILAR LIPOMA 8 DISORDER OF NOTOCHORDAL INTEGRATION 1 CAUDAL AGENESIS 1 DIASTEMATOMYELIA 2 SEGMENTATION ANOMALY 1 DORSAL DERMAL SINUS 1 NEUROENTERIC CYST 3 6 EMBRYOLOGICAL CLASSIFICATION OF SPINAL DYSRAPHISMS PRIMARY NEURULATION 4 T E R M I N O L O G Y 5 MENINGO-MYELOCELE = 1C # % 1A $ # * 1B T2 Sagittal image of spine (A) of a 1 day old baby and Axial T2 weighted image at lumbar spine (C) shows neural placode (#) extending above skin surface due to expansion of underlying subarachnoid space (=), which is characteristic of myelomeningocele. T2 Sagittal image of brain (B) showing thinned out corpus callosum, tectal beaking (%), elongated 4th ventricle and tonsillar herniation ($) suggestive of Chiari 2 malformation 6 Also note the cervical syrinx(*) LIPOMYELOCELE 2A 2D 2B 2C T2 (2A) and T1 weighted (2B) sagittal images showing fat intensity lesion forming a subcutaneous mass in the back with intra-spinal extension and a large intra-dural component T2 axial ( 2C) image and schematic diagram (2D) showing the lipoma-placode interface within the spinal canal suggestive of a lipomyelocele 7 LIPOMYELOCELE 2G 2H 2E 2F T2 sagittal image (2E) and STIR (2F) image showing herniation of neural tissue which is in contact with fatty tissue forming a subcutaneous mass T2 axial image (2G) shows the lipoma-placode interface within the spinal canal. Also note the posterior neural arch defect T2 coronal image (2H) showing associated left hydronephrosis 8 INTRADURAL LIPOMA 3A 3C 3D * L5 3B T2 axial image (3D) showing the intradural location with No spinal dysraphism or subcutaneous mass T2 (3A) and T1 (3B) weighted sagittal images of the lumbar spine showing Fat intensity lesion intradurally. There is associated tethered cord (conus ending at L5 veretebral level Coronal STIR image (3C) the lesion showing fat suppression (*) 9 DORSAL DERMAL SINUS 4C 4A 4B L4 4D ^ Sagittal T2 weighted (4A) and T1 weighted (4B) image showing a dorsal dermal sinus extending from the skin upto the posterior meninges. Associated tethered cord (conus at lower border of L4). No fat intensity within spinal canal 4CSchematic diagram of dorsal dermal sinus with intradural dermoid. 10 4D- T2 axial image showing the sinus tract (^) DISORDERS OF MIDLINE NOTOCHORDAL INTEGRATION neurenteric canal transiently connects the yolk sac to the amnion via the primitive knot which regresses during development of the embryo • Dorsal enteric fistula and Neurenteric cyst- Incomplete regression of neuro-enteric canal with abnormal communication between bowel and spinal canal • Diastematomyelia - when the persistent neuro-enteric canal splits the spinal cord into 2 hemicords DIASTEMATOMYELIA TYPE 1 WITH TETHERED CORD 5A Separation of the spinal cord into two hemicords is referred to as diastematomyelia. hemicords are usually symmetric AND Fuse back distally 5B L4 T2 axial image (5A) showing 2 hemicords with own dural sheath separated by a fibro-osseous septum. Type 1 diastematomyelia. Note the left hemicord syrinx. T2 sagittal image (5B)shows tethered cord PANG Type 1 - the two hemicords - individual dural and arachnoid covering separated by an osseous or cartilaginous septum PANG type 2- there is a single dural tube containing two hemicords, sometimes with an 12 intervening fibrous septum NEUROENTERIC CYST Present as a POSTERIOR MEDIASINAL CYSTIC MASS + VERTEBRAL ANOMALY 5B * 5C 5A T2 sagittal image (5A) shows a thoracic posterior mediastinal cystic mass, with associated anterior vertebral cleft (*) in T2 axial image (5B). Also note an incomplete diastematomyelia in a cranial axial section (5C) 13 Partial SACRAL AGENESIS TYPE 2 (TETHERED CORD) Caudal agenesis can be of two 6A 6B L4 types. In type 1, there is a high position and abrupt termination of the conus medullaris. In type 2, there is a low position and tethering of the conus medullaris( a/w thickened filum / lipoma) Figure (6A) showing absent distal sacral vertebral elements and coccyx. (6B) shows the conus terminating at upper border of L4 suggestive of tethered cord 14 COMPLEX DYSRAPHISM 7C Type 2 diastematomyelia at thoracic level with right hemicord syrinx 7A 7B L5 7D Vertebral segmentation anomalies Long segment syrinx Thickened filum terminale causing15 tethered cord. Associated Caudal agenesis CRANIORACHISCHISIS – ENCEPHALOMENINGOCELE WITH TETHERED DERMOID T2 coronal image (A) showing herniation of the right hemi-brainstem via a defect in the basi-sphenoid along with the right 7 and 8 cranial nerves. T2 axial (8B)and T1 axial (C) image shows associated meningocele. T1 axial image (a more caudal section) shows the fat intensity lesion 16 adhered to the encephalo-meningocele. CRANIORACHISCHISIS – ENCEPHALOMENINGOCELE WITH TETHERED DERMOID • Cranial dysraphism /Encephaloceles (1 / 40,000 LB) vs spinal dysraphism 1-3 / 1000 LB • Basal encephaloceles are rare (10% of encephaloceles) and they occur mostly in the fronto-ethmoidal area. (>90%) • So far in literature, no such case of brainstem herniation with meningocele via a lateral basal, basi-sphenoid bony defect has been described. • We hence report this as the first case in Literature. 17 CONCLUSION • MRI is an excellent imaging modality for characterizing spinal dysraphisms. • MRI is indicated even in obvious open neural tube defects, contrary to the conventional teaching, to look for associated Chiari malformation, syringomyelia etc. • MRI plays a role in the post-operative follow up of many lesions especially to assess ascent of cord post de-tethering. • It is important to diagnose closed spinal dysraphisms without subcutaneous masses where no clinical mass is seen, as neurological deficits can be arrested if diagnosed and treated early. 18 CLINICO-RADIOLOGICAL CLASSIFICATION OF SPINAL DYSRAPHISMS 19 REFERENCES • Congenital Spine and Spinal Cord Malformations—Pictorial Review Stephanie L. Rufener et.al. (2008) – AJR integrative imaging • MRI findings in occult spinal dysraphisms– S. Morrthy et.al (IJRI2003) • MR imaging in the tethered cord syndrome - Narasimhachan Raghavan et.al. (AJNR- 1989) • MRI in Infants and Children with Spinal Dysraphism -P D Barnes et.al (AJNR -1986) 20