How Effective are
Antithrombotic Therapies in PPCI
Dr Adeel Shahzad
Dr Rod Stables (PI)
Liverpool Heart and Chest Hospital
Liverpool, UK
• Anti-thrombotic therapy in PPCI
• Selective (‘bailout’) use of GP IIb/IIIa antagonists (GPI)
• Increasingly the norm in routine practice
• Recommended by international guidelines
• ESC ACCF / AHA
• Anti-thrombotic therapy in PPCI
• Selective (‘bailout’) use of GP IIb/IIIa antagonists (GPI)
• Increasingly the norm in routine practice
• Recommended by key guidelines (ESC, ACCF / AHA)
• Bivalirudin + selective (7% - 15%) use of GPI
• Established anti-thrombotic treatment option
• Bleeding is associated with less favourable outcomes
• Increased GPI use - results in increased bleeding
• Observed for both bivalirudin and heparin
• Relative performance of bivalirudin and heparin -
• Cannot be reliably assessed with differential GPI use
• HEAT PPCI
• Bivalirudin + selective GPI v Heparin + selective GPI
• Bleeding is associated with less favourable outcomes
• Increased GPI use - results in increased bleeding
• Observed for both bivalirudin and heparin
• Relative performance of bivalirudin and heparin -
• Cannot be assessed reliably with differential GPI use
• HEAT PPCI
• Bivalirudin + ‘bailout’ GPI v Heparin + ‘bailout’ GPI
• Single centre RCT
• Trial recruitment: Feb 2012 - Nov 2013 22 months
• Bivalirudin v Unfractionated Heparin
• STEMI patients
• Randomised at presentation
• Acute phase management with Primary PCI
• Single centre RCT
• Trial recruitment: Feb 2012 - Nov 2013 22 months
• Bivalirudin v Unfractionated Heparin
• STEMI patients
• Randomised at presentation
• Acute phase management with Primary PCI
• Philosophy for clinical teams:
• Assess ‘Every Patient - Every Time’
Inclusion Criterion
• All STEMI patients activating PPCI pathway
Exclusion Criteria
• Active bleeding at presentation
• Factors precluding administration of oral A-P therapy
• Known intolerance / contraindication to trial medication
• Previous enrolment in this trial
• Dual oral anti-platelet therapy pre-procedure
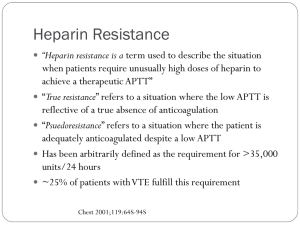
• Heparin:
70 units/kg body weight pre-procedure
• Bivalirudin: Bolus 0.75 mg/kg
Infusion 1.75 mg/kg/hr - procedure duration
• Dual oral anti-platelet therapy pre-procedure
• Heparin:
70 units/kg body weight pre-procedure
• Bivalirudin: Bolus 0.75 mg/kg
Infusion 1.75 mg/kg/hr - procedure duration
• GPI - Abciximab
• Selective (‘bailout’) use in both groups
• ESC guideline indications
At 28 days
Primary Efficacy Outcome Measure
• Major Adverse Cardiac Events (MACE) • All-cause mortality
• Cerebrovascular accident (CVA)
• Re-infarction
• Unplanned target lesion revascularisation (TLR)
At 28 days
Primary Efficacy Outcome Measure
• Major Adverse Cardiac Events (MACE)
Primary Safety Outcome Measure
• Major bleeding • Type 3-5 bleeding as per BARC definitions
• Data Monitoring and Safety Committee (DMSC)
• All key clinical events adjudicated
• Clinical Events Committee
• Blinded to the treatment allocation
• Use of a delayed consent strategy
• Full UK ethical approval
• Patients randomised and treated without discussion
• Subsequent informed consent in recovery phase
• Additional national approval -
• Use of data from patients who died before consent
1917 patients scheduled for emergency angiography
29 (1.5%) already randomised in the trial
59 (3.0%) met one or more other exclusion criteria
1829 eligible for recruitment
1917 patients scheduled for emergency angiography
29 (1.5%) already randomised in the trial
59 (3.0%) met one or more other exclusion criteria
1829 eligible for recruitment
1829 Randomised
Representative ‘Real-World’ Population
Assigned to Heparin 914
Received allocated Rx 900
Received no study drug 14
Treatment cross-over 0
LMWH pre-procedure 3
915 Assigned to Bivalirudin
907
7
1
4
Received allocated Rx
Received no study drug
Treatment cross-over
LMWH pre-procedure
Assigned to Heparin 914
Received allocated Rx 900
Received no study drug 14
Treatment cross-over 0
LMWH pre-procedure 3
Consent not available
7
in surviving patients
Included in analysis 907
915 Assigned to Bivalirudin
907
7
1
4
Received allocated Rx
Received no study drug
Treatment cross-over
LMWH pre-procedure
Consent not available
10
in surviving patients
905 Included in analysis
Characteristic
Bivalirudin
Heparin
Median age (years)
62.9
63.6
Female sex (%)
28.5
26.9
Caucasian race (%)
95.8
95.9
Diabetes mellitus (%)
12.6
15.1
Previous MI (%)
13.5
10.3
eGFR (ml/min/1.73m2)
80.0
80.0
Haemoglobin (g/dl)
13.6
13.7
Characteristic
Bivalirudin (%)
Heparin (%)
99.6
99.5
- Clopidogrel
11.8
10.0
- Prasugrel
27.3
27.6
- Ticagrelor
61.2
62.7
GPI use
13.5
15.5
Radial arterial access
80.3
82.0
PCI performed
83.0
81.6
P2Y12 use - Any
Characteristic
Bivalirudin (%)
Heparin (%)
Thrombectomy
59.1
57.6
Single vessel Tx
93.2
90.3
Any stent implant
92.8
92.2
DES implantation
79.8
79.9
TIMI III flow - post PCI
93.3
92.7
Bivalirudin
MACE
n
%
79
8.7 %
Heparin
v
%
n
5.7 %
52
Absolute risk increase = 3.0% (95% CI 0.6, 5.4)
Relative risk = 1.52
(95% CI 1.1 – 2.1)
P=0.01
Event curve shows first event experienced
Bivalirudin
n
%
Death
46
5.1 %
CVA
15
Reinfarction
Heparin
%
n
v
4.3 %
39
1.6%
v
1.2%
11
24
2.7%
v
0.9%
8
TLR
24
2.7%
v
0.7%
6
Any MACE
79
8.7 %
v
5.7 %
52
Bivalirudin
n
%
Death
46
5.1 %
CVA
15
Reinfarction
Heparin
%
n
v
4.3 %
39
1.6%
v
1.2%
11
24
2.7%
v
0.9%
8
TLR
24
2.7%
v
0.7%
6
Any MACE
79
8.7 %
v
5.7 %
52
Censored by the most significant event - in order displayed
Bivalirudin
n
%
Death
46
5.1 %
CVA
11
Reinfarction
Heparin
%
n
v
4.3 %
39
1.2%
v
0.6%
6
21
2.3%
v
0.8%
7
TLR
1
0.1%
v
0%
0
Any MACE
79
8.7 %
v
5.7 %
52
Censored by the most significant event - in order displayed
Bivalirudin
n
%
Death
46
5.1 %
CVA
11
Reinfarction
Heparin
%
n
v
4.3 %
39
1.2%
v
0.6%
6
21
2.3%
v
0.8%
7
TLR
1
0.1%
v
0%
0
Any MACE
79
8.7 %
v
5.7 %
52
ARC definite or probable stent thrombosis events
Bivalirudin
All Events
n
%
24
3.4 %
Relative risk = 3.91
Heparin
v
%
n
0.9 %
6
(95% CI 1.6 - 9.5)
P=0.001
ARC definite or probable stent thrombosis events
Bivalirudin
n
%
Definite
23
3.3 %
Probable
1
Acute
Subacute
Heparin
%
n
v
0.7 %
5
0.1 %
v
0.1 %
1
20
2.9 %
v
0.9 %
6
4
0.6%
v
0%
0
Major Bleed BARC grade 3-5
Bivalirudin
Major Bleed
n
%
32
3.5 %
Relative risk = 1.15
Heparin
v
%
n
3.1 %
28
(95% CI 0.7 - 1.9)
P=0.59
Major Bleed BARC grade 3-5 Minor Bleed BARC grade 2
Bivalirudin
n
%
Minor Bleed
83
9.2 %
Major or Minor
113
12.5 %
Minor Bleed P=0.25
Heparin
%
n
v
10.8 %
98
v
13.5 %
122
Major or Minor P=0.54
• Single centre
• Potential impact minimised by:
• Meticulous trial conduct
• Unselected representative population
• Study treatments are iv drugs (no ‘skill’ component)
• Multiple operators
• Outcomes as expected by national norms
• Single centre
• Open label
• Potential impact minimised by:
• Complete follow-up - No ‘lost’ cases
• Outcome measures were overt clinical events
• Most MI events involved angiographic imaging
• Independent blinded adjudication
• Open label used in HORIZONS and EUROMAX
• A unique study with 100% recruitment of eligible patients
• A unique study with 100% recruitment of eligible patients
Use of heparin rather than bivalirudin
• Reduced rate of major adverse events (NNT = 33)
• Fewer stent thromboses and reinfarction events
• A unique study with 100% recruitment of eligible patients
Use of heparin rather than bivalirudin
• Reduced rate of major adverse events (NNT = 33)
• Fewer stent thromboses and reinfarction events
• Consistent effect across pre-specified subgroups
• A unique study with 100% recruitment of eligible patients
Use of heparin rather than bivalirudin
• Reduced rate of major adverse events (NNT = 33)
• Fewer stent thromboses and reinfarction events
• Consistent effect across pre-specified subgroups
• No increase in bleeding complications
• A unique study with 100% recruitment of eligible patients
Use of heparin rather than bivalirudin
• Reduced rate of major adverse events (NNT = 33)
• Fewer stent thromboses and reinfarction events
• Consistent effect across pre-specified subgroups
• No increase in bleeding complications
• Potential for substantial saving in drug costs
0
1
Subgroup
Relative Risk (95% CI)
All patients
P Value for
interaction
1.52 (1.09, 2.13)
Arterial access site
0.87
Radial
1.58 (1.01, 2.48)
Femoral
1.45 (0.70, 2.98)
Diabetes
0.35
Yes
2.22 (1.04, 4.76)
No
1.54 (1.04, 2.28)
Age
0.11
≥75
1.09 (0.68, 1.77)
<75
1.97 (1.23, 3.16)
Favours Bivalirudin
Favours Heparin
2
Subgroup
Relative Risk (95% CI)
P2Y12 agent used
P Value for
interaction
0.78
Clopidogrel
1.34 (0.54, 3.31)
Prasugrel
1.91 (0.87, 4.21)
Ticagrelor
1.41 (0.93, 2.14)
Left Ventricular Function Impaired
0.67
Yes
1.28 (0.84, 1.95)
No
1.63 (0.64, 4.16)
PCI attempted
0.88
Yes
1.55 (1.06, 2.28)
No
1.45 (0.71, 2.96)
Favours Bivalirudin
Favours Heparin
3
Event curve shows first major bleed experienced
4
Thrombocytopenia
(%) new onset <150
CKMB post procedure
Median (ng/dl)
Door-first device time
Median (mins)
Bivalirudin
Heparin
P value
8.3
7.3
0.49
97
106
0.55
29
29
0.33
5
Bivalirudin
Heparin
P value
Normal (EF >54%)
45.4%
43.9%
0.53
Mild (EF 45-54%)
25.2%
26.2%
0.65
Moderate (EF 36-44%)
20.1%
19.8%
0.88
Severe (EF <36%)
9.3%
10.1%
0.60
6
Common assumptions - based on historic connotations
• Smaller studies - often underpowered
• Potential subversion of randomisation
• Less robust trial procedures and documentation
• No adjudication of adverse events
7
Common assumptions - based on historic connotations
• Smaller studies - often underpowered
• Potential subversion of randomisation
• Less robust trial procedures and documentation
• No adjudication of adverse events
No active problems for HEAT PPCI
8
Issues related to the patient population
• Unselected: External referral to trial centre
• Near universal inclusion in trial
• Patients typical for UK population
• Predominantly Caucasian race
8
Issues related to the patient population
• Unselected: External referral to trial centre
• Near universal inclusion in trial
• Patients typical for UK population
• Predominantly Caucasian race
May affect generalisation to other populations
9
Issues related to clinical performance and outcomes
In HEAT PPCI • Randomised treatments are routine iv medications
• Established and standardised approach to
• Purchase and storage
• Administration and dosing
• Outcomes are not affected by practice pattern or ‘skill’
10
Issues related to clinical performance and outcomes
In HEAT PPCI • Randomised treatments are routine iv medications
• Established and standardised approach to
• Purchase and storage
• Administration and dosing
• Outcomes are not affected by practice pattern or ‘skill’
Minimal threat in HEAT PPCI
11
Issues related to clinical performance and outcomes
• Treatments administered in setting of a PPCI procedure
• Procedures performed by 14 different cardiologists
• Operator and institution outcomes as expected
• Match national and international norms for PPCI
12
Issues related to clinical performance and outcomes
• Treatments administered in setting of a PPCI procedure
• Procedures performed by 14 different cardiologists
• Operator and institution outcomes as expected
• Match national and international norms for PPCI
Minimal threat in HEAT PPCI
13
Registry and Trial
PPCI Outcomes
Mortality (%)
HORIZONS (30d)
2.6 %
EUROMAX (30d)
3.0 %
US CathPCI 2011 (In-Hosp)
5.7 %
UK BCIS 2012 (30d)
6.4 %
HEAT PPCI (28d)
4.7 %
14
• Comprehensive follow-up
• No ‘lost’ cases
15
• Comprehensive follow-up
• All primary efficacy and safety outcome measures • Overt clinical events with robust documentation
• MI events substantiated by imaging in almost all cases
16
• Comprehensive follow-up
• All primary efficacy and safety outcome measures
• Overt clinical events with robust documentation
• MI events substantiated by imaging in almost all cases
• Independent adjudication of events
• Blinded to patient identity and treatment allocation
17
• Comprehensive follow-up
• All primary efficacy and safety outcome measures
• Overt clinical events with robust documentation
• MI events substantiated by imaging in almost all cases
• Independent adjudication of events
• Open label norm - used in HORIZONS EUROMAX
18
• Estimated MACE rate = 7.5%
• Sample size 1800 patients
• Two-sided testing
• Allows superiority testing in favour of either agent
• Pre-specified boundaries for
• Non-Inferiority
Equivalence
• Calculations based on absolute event rate difference
19
• Assuming no observed treatment difference
‘Treatment A’ 7.5% = 7.5% ‘Treatment B’
• Event rate difference = 0%
• Calculate 95% CI for the rate difference
-2.4%
0%
+2.4%
20
• Assuming an observed treatment difference
‘Treatment A’ 5.5% = 8.0% ‘Treatment B’
• Event rate difference = 2.5%
• Calculate 95% CI for the rate difference
-2.3%
2.5%
+2.3%
21
-2.3%
2.5%
+2.3%
4% 3% 2% 1% 0%
Favours Treatment A
1% 2% 3% 4%
Favours Treatment B
Event Rate Difference
22
-2.3%
4% 3% 2% 1% 0%
Favours Treatment A
2.5%
+2.3%
1% 2% 3% 4%
Favours Treatment B
Event Rate Difference
25
Point estimate lies in zone ± 0.5% from zero difference
4% 3% 2% 1% 0%
Favours Treatment A
1% 2% 3% 4%
Favours Treatment B
Event Rate Difference
26
-2.4%
+2.4%
0.4%
-2.4%
+2.4%
0.4%
4% 3% 2% 1% 0%
Favours Treatment A
1% 2% 3% 4%
Favours Treatment B
Event Rate Difference
23
Point estimate better than (-0.5%)
4% 3% 2% 1% 0%
Favours Treatment A
1% 2% 3% 4%
Favours Treatment B
Event Rate Difference
24
Point estimate better than (-0.5%)
-2.4%
1%
+2.4%
4% 3% 2% 1% 0%
Favours Treatment A
1% 2% 3% 4%
Favours Treatment B
Event Rate Difference
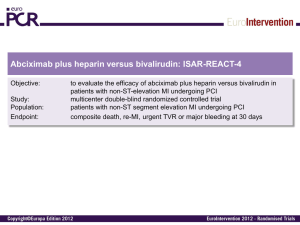
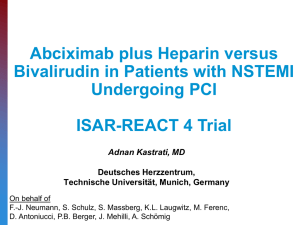
• Anti-thrombotic therapy in PPCI for STEMI
• Selective (‘bailout’) use of GP IIb/IIIa antagonists (GPI)
• Increasingly the norm in routine practice
• Recommended by key guidelines (ESC, ACCF / AHA)
• Bivalirudin + selective (7% - 15%) use of GPI
• Established anti-thrombotic treatment option
• Bivalirudin and heparin • Appear to have similar anti-ischaemic efficacy
• Similar impact on MACE events
HAS
REPLACE
REPLACE 2
ISAR REACT 4
ACUITY
ISAR REACT 3
HORIZONS
ISAR REACT 3A
EUROMAX
No difference in ischaemic outcomes
• Bivalirudin and heparin - similar impact on MACE events
• Use of GPI agents causes increased bleeding
• When used with heparin
Heparin
Heparin
EPIC
Placebo
GPI Universal
RESTORE
Placebo
GPI Universal
PRISM Plus
Placebo
GPI Universal
CAPTURE
Placebo
GPI Universal
↑ bleeding with ↑ GPI use
• Bivalirudin and heparin - similar impact on MACE events
• Use of GPI agents causes increased bleeding
• When used with heparin
• When used with bivalirudin
ACUITY
Bivalirudin
Bivalirudin
GPI Bailout
GPI Universal
9%
97 %
↑ bleeding with ↑ GPI use
• Bivalirudin and heparin - similar impact on MACE events
• Use of GPI agents causes increased bleeding
• With similar GPI use • Bivalirudin and heparin have similar bleeding rates
Bivalirudin
Heparin
GPI Universal
GPI Universal
ACUITY
97 %
97 %
REPLACE
72 %
71 %
No differences in bleeding
• Bivalirudin and heparin - similar impact on MACE events
• Use of GPI agents causes increased bleeding
• With similar GPI use • Bivalirudin and heparin have similar bleeding rates
• With differential GPI use • Bivalirudin and heparin have different bleeding rates
Bivalirudin
Heparin
GPI Bailout
GPI Universal
ACUITY
9%
97 %
ISAR REACT 4
0%
100 %
HORIZONS
7%
98 %
EUROMAX
9%
70 %
↑ bleeding with ↑ GPI use
• Bleeding is associated with less favourable outcomes
• Increased GPI use - results in increased bleeding
• Observed for both bivalirudin and heparin
• Relative performance of bivalirudin and heparin -
• Cannot be assessed reliably with differential GPI use
• HEAT PPCI
• Bivalirudin + selective GPI v Heparin + selective GPI