gas gangrene

GAS GANGRENE
Dr. Ehsanur Reza Shovan
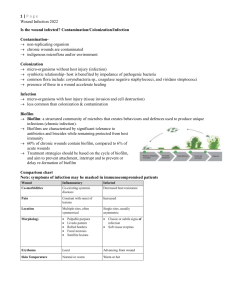
• It is a rapidly progressive, potentially fatal condition characterized by widespread necrosis of the muscles and subsequent soft-tissue destruction.
• This is a dreaded consequence of inadequately treated missile wounds, crushing injuries and highvoltage electrical injuries.
Causative agent
• Clostribium species – spore forming, Gram +ve c.septicum
c.novyi
c. Perfringens
(mostly)
• They are present in the soil and have also been isolated from the human gastrointestinal tract and female genital tract.
• Non-clostridial gasproducing organisms such as coliforms have also been isolated in 60–85% of cases of gas gangrene.
Spores germinate vegetative cells multiply
Carbohydrates
Fermentation
Anaerobic environment
PATHOGENESIS
Incubation period is
1-7 days
Gas production
In tissues
Distension of tissues
Toxemia and death Interfering
Blood supply
Ischemia/ gangrene
Pathogenesis
Bacteria enters the broken skin or wound
-
Spores are produced
The bacteria present in circulation system
- The toxins
(lecithinase) and enzyme are produced
-
The bacteria are grow and ferment the muscle carbohydrate the anaerobic tissue present
Examples of enzyme: colagenases, proteases and lipases
- These enzymes will kill other host cell and extend the anaerobic environment
Produce gases ( nitrogen, hydrogen sulphide and carbon dioxide )
Crepitant tissue
( destroyed tissue)
Epidemiology
– The persons at risk those with Diabetes Mellitus, blood vessel disease and colon cancer
– Contact with contaminated cloth and other foreign material
– Trauma or recent surgical wound
Symptoms
• High fever
• Shock
• Massive tissue destruction
• Blackening of skin
• Severe pain around a skin of wound
• Blisters with gas bubbles form near the infected area,
• the heartbeat and breathing become rapid.
Presentation
Crepitation in tissues, sickly sweet odor discharge, rapidly progressing necrosis, fever, hemolysis, toxemia, shock, renal failure, and death
Lab. Investigations
Culture and sensitivity
Storming fermentation
Lecithinase test
S
S
I
T
U
E
F
T
S
O
G
A
S
I
N
U
R
U
T
E
S
N
I
G
A
S
G
A
S
I
N
E
R
U
T
U
S
G
A
S
I
N
E
R
U
T
U
S
Prevention
• Cleaning the wound
• Avoid the contaminated material
• improve circulation in patients with poor circulation
• antitoxin
Prevention
(1) Do a thorough wound toilet.
(2) In high risk wounds give the patient penicillin 1.5 megaunits 4 hourly, or tetracycline
Treatment
• High doses of antibiotic : Penicillin
• The dead tissue is removed or limbs are amputated
• No vaccine
10 megaunits of benzyl penicillin daily for 5 days as four 6 hourly doses.
Or
Tetracycline 0.5 g intravenously or 1 g orally every 6 hours.
Clostridia not sensitive to metronidazole, some other anaerobic bacteria are, so give it.
EXPLORATION
Do this in a septic theatre, or even in the out-patient department, and not where clean cases go for operation.
AMPUTATION
Amputate under a tourniquet
Close the stump by delayed primary suture
Myonecrosis of right leg
Myonecrosis of left foot
Stump of above knee amputation
• Patients should be admitted to ICU and treated aggressively with careful monitoring.
• The role of HBO is not as clear as in necrotising fasciitis but it is recommended in severe cases if the facilities are available.
– increases the normal oxygen saturation in the infected wounds by 1000-fold leading to
• Bacteriocidal effect,
• Improves neutrophil function,
• Enhanced wound healing