Healthcare Executive*s Role in IT Decisions
advertisement
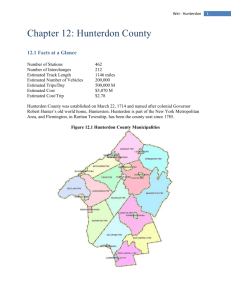
Healthcare Executive’s Role in IT Decisions November 11, 2013 Richard Wheatley, CIO Cape Regional Medical Center Glenn Mamary, VP/CIO Hunterdon Healthcare Healthcare IT Video http://www.youtube.com/watch?v=zzS-zX920nc Agenda • Medical Center Profiles: – Cape Regional Health System – Hunterdon Healthcare • State of Healthcare Information Technology • Current Challenges • Ensuring Success of IT Projects • IT Governance / Data Governance • Data Analytics • Pitfalls and Perils • Suggested Readings • Panel Discussion Capital Regional Health System Cape Regional Heath System • Cape Regional Medical Center – 242 Licensed Beds – Average Daily Census = 85 – Annual ED Visits = 45,000 – $110,000,000 Annual Revenue – Clinical affiliation with University of Penn Medicine – Seasonal volumes – Sole acute care provider in Cape May County, NJ – Highly competitive environment Cape Regional Heath System • Cape Regional Physician Associates – 40 providers – 8 Locations • Cape Regional Urgent Care • Cape VNA partnership with Central Jersey VNA • Health Information Exchange – New Jersey Southern Health Information Network Exchange (NJSHINE) – Inspira Health Network – Shore Medical Center Hunterdon Healthcare Hunterdon Healthcare • Hunterdon Medical Center – 178 Licensed Beds – $290,034,000 Annual Revenue – Comprehensive medical, diagnostic, surgical, behavioral health, rehabilitative and preventative services for inpatients and outpatients • Hunterdon Regional Community Health – Hunterdon Hospice – Visiting Health and Supportive Services • Hunterdon Wellness Centers – (Clinton & Whitehouse) 7 Hunterdon Healthcare About Hunterdon Healthcare • Hunterdon Healthcare Partners IDS – 25 Owned Practices (Multispecialty) – 25 Private Practices (Multispeciality) (23 Level 3 Patient Centered Medical Homes) • Accountable Care Organizations – Aetna – Blue Cross – Cigna • Health Information Exchange – Jersey Health Connect (Relay Health) – Medicity • Magnet Recognition • “100 Most Wired”, Hospital Health Network – 12 Years 8 ACO Requirements • • • • • • • • Effectively manage medications Organize problem list Track and manage diseases for individual patients Communicate and track referrals or consultations Document transitions of care Manage patient encounters across long periods of time Provide “dashboards” and summary of care or information Consolidate diagnostic information from a variety of providers ACO Requirements • Engage patients in self-health management activities • Stratify patient according to risk • Ensure use of best practice and evidence-based medicine across providers and the continuum of care • Communicate a multidisciplinary plan of care and ensure accountability • Coordinate services across a virtual care team Current Challenges Current Challenges Closing the Gap – How do we get there? State of Healthcare IT • Meaningful Use – Summary of Care Records (10% of all transitions of care) – Patient Portals (5% of unique patients) – CPOE driven by actual numbers of orders • (60% meds, 30% lab, 30% rad) • ICD10 Transition – Upgrading all EHR systems – Educating staff and clinicians – Computer Assisted Coding – Training – Testing • Multiple vendors • Interfaces • While testing MU – Moving parts State of Healthcare IT • • • • • • EMR Optimization and integration Accountable Care Organizations (ACOs) Health Information Exchanges (HIEs) Population Health Management Business Intelligence /Health Analytics Mobility Current Challenges • Financial – Maximize value of current technology investments – Collect, track, and understand data/information (including unstructured data) – Minimize cost related to building/maintaining interfaces, new “products” • Outreach/connectivity – Support and connect stakeholders across enterprise – Improve quality and cost-effectiveness of care – Manage information across disparate platforms • Long-term strategy – Future changes – technology/regulatory/consumer driven – Maintain a competitive advantage Current Challenges • • • • • Cost pressures Time pressures More IT-enabled initiative Greater expectations for value / ROI Stress on HIT industry – Staff retention (competition from vendors, consultants) • Rapid pace/potential for burn-out • Texting PHI • Data from external sources – Timeliness – Quality Health Information Exchanges • HIE is a way for health care providers across the state to share information electronically. HIE benefits both health care providers and patients by delivering the right information to the right place at the right time HIE Functionality • Access to lab results & clinical documents from other health systems’ inpatient & ancillary services via existing clinical systems • Allow electronic communication with other providers across the care community outside HHS • Enable the sharing of patient health summaries across the regional HIE and other state HIEs • Meaningful Use support • Patient Portal • Future images Ensuring Success of IT Projects • Healthcare Executive’s Role – Executive sponsorship – Ensure stakeholder participation/buy-in – Ensure transparency – Hold the organization accountable – Promote Project Management Office / Process – Data Governance Project Life Cycle • Identify need – What problem are you attempting to solve? – Develop Request For Proposal (RFP) – Goals and objectives – Define Scope / Milestones – Return on investment (ROI) • Hard • Soft – Measures of success – Beware of the “unsupported” system Project Life Cycle • Selection process – Committee/Participation Leadership • Build consensus • Neutralize/marginalize the “nay-say’ers” • All stakeholders • Timing of involvement – On-site demonstrations – Site visits / Reference checks • Like organizations where possible – Vendor fairs – Survey and score everything – Communicate, communicate, communicate Project Life Cycle • Selection process (continued) – The larger the organization, the more difficult it will be – This will always take longer than you anticipate – Ensure that selection is not an IT selection – Is rest of senior leadership on board? Project Life Cycle • Budget – Don’t rely solely on vendor estimates – Ensure that everyone (IT Steering committee, senior management) has input reviewed and approved – 3-5 year Total Cost of Ownership (TCO) • Remote computing versus in-house • Capital versus operating Project Life Cycle • Budget (Continued) – Software and hardware (servers, pc’s, WOW’s, tablets, etc…) – Vendor travel costs – Project staffing (temporary positions?) – Training and Education • Education for project staff • Hospital travel costs • Costs for back-fill of positions (“Super-user” and general staff) Project Life Cycle • Budget (continued) – Interface/Integration costs – There are always two sides of each interface – System activation • Additional/ backfill staff time • Additional vendor or third party resources – “Other” vendor costs – Don’t forget about Disaster Recovery! • Vendor Partnerships – Alpha / Beta Sites – Development partners Project Life Cycle • Project Governance – Project Steering Committee • Chaired by Executive Sponsor • Key stakeholders and decision makers • Vendor executives – Project leadership • In-house versus third party – Project team • IT Lead • Departmental Lead(s) • Vendor Lead(s) Information Technology Governance • Who? • Demand Management versus Capacity Management – Stopping the “Yes Machine” – Organizational Capacity versus IT Capacity • Focus on strategic initiatives • Outcomes focused – Examples • CPOE % • Order set usage • Quality indicators • Meaningful Use Information Technology Governance • Prioritization of projects – Patient safety – Quality – Strategic Initiative – Regulatory/Compliance (includes Meaningful Use and ICD10) – Optimization/Efficiency – Routine Information Technology Governance • Long term IT capital planning – You can plan for 5 years on many things • The life expectancy of hardware and infrastructure is somewhat predictable • Replace X% of PC’s, network switches, every year – It is difficult to plan on software replacements/upgrades • At the mercy of software suppliers • Business and outcomes driven Data Governance • Importance of data governance: – Data Integrity • Patient safety from an EMR • Accurate financial – Data integration and workflow – Data security – Data definitions used for data analytics Data Governance • Building a successful data governance strategy: – Executive sponsors from both senior management and the business units. – Management committee such as a steering committee or data stewardship council. – Data governance lead such as a data czar or chief steward. – Data stewards, the caretakers of the enterprise data assets. – Data owners, responsible for the creation of the data and the enforcement of enterprise business rules. www.accenture.com Data Governance • There should be a single set of data policies and procedures that ensure the integrity, consistency and sharing of the enterprise's data resources. Data policies might include adherence of data to business rules; enforcing authentication and access rights to data; compliance with laws and regulations; and protection of data assets. • In addition to data policies, organizations should employ data standards to outline the precise criteria, specifications and rules for the definition, creation, storage and usage of data within the enterprise www.accenture.com Hospital Scorecard 38 LOS Scorecard 39 Fall Risk Assessment 40 Patient Safety Indicators 41 Readmission Rates 42 Pitfalls and Perils • Innovation – “Bleeding edge” of technology – Chasing technology has risks – How to mitigate risk – Will the technology provide a competitive edge? • Buy versus build • In the end, it is less about the technology and more about the process. It’s all about the patient! • Sharing data and images across all of our systems – all “talk” to each other = information • Ability of patients to contribute to their care and interact with the EHRs • Sending and Receiving data with outside systems = better information Recommended Reading • AHA Online Store • CHG-Monograph-Consolidation, Clinical Integration & Transformation: Investing in Information Technology for an Accountable System of Care • Product Code: CHG - Mono42013