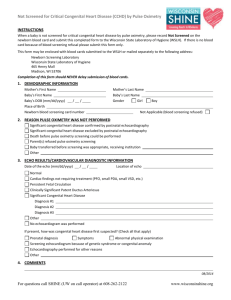
Newborn Screening for Critical Congenital Heart Defects
advertisement
Newborn Screening for Critical Congenital Heart Defects by Pulse Oximetry Fall CME Course 2012 Robert Jansen, MD St. Vincent Women’s Hospital Disclosures • I have no financial relationships to disclose • I will not discuss off label use or unapproved or investigational use of products or devices Indiana Senate Bill 0552 Passed February 2011 “Cora’s Law” •Per 16-41-17-2, effective January 1, 2012, all birthing facilities in Indiana will be required to perform pulse oximetry screening on all newborns to detect critical congenital heart defects (CCHDs). Perspective on Importance • In the United States: ♥ Nearly 40,000 infants/year with CHD ♥ 4,800 infants/year with CCHD ♥ Estimated as many as 200 infants/year die due to unrecognized CCHD ♥ Median age for these deaths is < 2 weeks Critical Congenital Heart Disease ♥ Outflow tract defects – – – – Tetralogy of Fallot D-Transposition of the Great Vessels Truncus Arteriosus Total Anomalous Pulmonary Venous Return ♥ Right –sided obstructive defects – Tricuspid atresia – Pulmonary atresia, intact septum ♥ Left-sided obstructive defects – Hypoplastic left heart Transitional Circulation ♥ Circulatory changes include: ♥ ♥ ♥ ♥ Increase in systemic vascular resistance Decrease in pulmonary vascular resistance Increase in left atrial pressure Closure of the ductus arteriosus and foramen ovale ♥ Increase in left ventricular stroke volume Perspective on Importance: Timing of Diagnosis of CCHD Endorsement of CCHD Screening CCHD screening endorsed by HHS Secretary Kathleen Sibelius September, 2011 AHA, ACC, AAP, and March of Dimes all endorse CCHD screening US CCHD Screening by States 9/2012 Screening Principles Incidence of Congenital Heart Disease ♥ According to the March of Dimes, CHD is the most common birth defect ♥ 8/1000 babies are born with CHD – 11.6/10,000 have one of the 7 CCHDs ♥ 4/1000 require treatment within the first year of life CHD: Morbidity and Mortality ♥ Failure to diagnose CCHD may lead to critical events, cardiogenic shock or death ♥ Neurological outcome poor with late diagnosis Prenatal Diagnosis of CCHD ♥ Prenatal Ultrasound – Usually provides a four-chamber view of the fetal heart – Variable in quality – Detect 15% (AR)-23% (CA), to possibly 50% (estimate of best capability) of CCHDs Detection of CHD by Physical Exam ♥ 44% of CHD detected by PE alone (Wren, Arch Dis Child Fetal Neonatal Ed 80:1999) ♥ 1/12 with murmur heard in the first day of life have CHD (Nadas’ Pediatic Cardiology) ♥ Findings associated with CCHD may not be present in the nursery The Cyanotic “Blind Spot” JS Hokanson, Neonatology Today, Dec. 2010 Reliability of Pulse Oximetry Screening for CCHD ♥ Meta-analysis of13 eligible studies with data for 229,421 newborn babies ♥ Overall sensitivity of pulse oximetry for detection of critical congenital heart defects was 76·5% (95% CI 67·7—83·5) ♥ Specificity was 99·9% (95% CI 99·7—99·9) ♥ False-positive rate of 0·14% (95% CI 0·06— 0·33) Thangaratinam et al. The Lancet, Early Online Publication, 2 May 2012 doi:10.1016/S01406736(12)60107-X Reliability of Pulse Oximetry Screening for CCHD ♥ The false-positive rate for detection of critical congenital heart defects was particularly low when newborn pulse oximetry was done after 24 h from birth compared to being done before 24 h (0·05% [0·02—0·12] vs 0·50 [0·29—0·86]; p=0·0017). Thangaratinam et al. The Lancet, Early Online Publication, 2 May 2012 doi:10.1016/S0140-6736(12)60107-X Feasibility of implementing pulse oximetry screening for congenital heart disease in a community hospital ♥ From January 2009 through May 2010, of 6841 eligible newborns, 6745 newborns (98.6%) were screened. ♥ Of the nine infants with positive pulse oximetry screens: – one had CCHD – four had CHD – four others were determined to have false positive screens ♥ Average screening time was 3.5 min (0 to 35 min). Bradshaw et al Journal of Perinatology advance online publication 26 January 2012; doi: 10.1038/jp.2011.179 Barriers to Screening ♥ Barriers identified for a total of 166 of the 6841 enrolled newborns eligible for screening (2.4%). – screening equipment (53.6% of the time) • Did not work • Problems with probe placement – staff (22.9%) • Too busy – infant (19.9%) • Infant crying or very active – family (3.6%) • Mom was in a rush – In 100% of cases where the barrier was staff-related, the infant was ultimately not screened. Barriers to Screening ♥ Time required to overcome barriers was documented in 34 infants successfully screened and averaged 5.1 min per infant (2 to 10 min). Costs of Screening ♥ Pulse oximeter probe ~ $30 ♥ Staff time – Doing screens – Reporting requirements ♥ “Down-stream” costs for failed screens – Echocardiograms – Transport Performing Pulse Oximetry Screening Screening in Your Nursery ♥ Pair screening with other standard-of-care newborn screening ♥ Consider conducting screening in a quiet area with parents present ♥ Conduct screening while the infant is awake and quiet ♥ Do not attempt pulse oximetry screening on an infant who is crying or cold Indiana Legislative Action •Infants who are in the NICU should receive pulse oximetry screening or an echocardiogram prior to discharge in order to be compliant with Indiana’s newborn screening law. All birthing facilities with NICUs are responsible for developing protocols in order to ensure that EVERY baby in the NICU is screened for CCHD. •The heelstick card itself will be modified in 2012 to include pulse oximetry data. Until that time, only children who fail or do not receive pulse oximetry newborn screening need to be reported to ISDH as part of the Pulse Oximetry Monthly Summary Report. The infant who fails the screening ♥ IF INFANT SYMPTOMATIC, TRANSFER TO NICU ♥ IF ECHO ABNORMAL, REFER TO NICU/PEDIATRIC CARDIOLOGY ♥ IF ECHO NORMAL AND INFANT ASYMPTOMATIC, CLINICAL ASSESSMENT/CONSULT WITH NEONATOLOGIST Important Note ♥ Passing the newborn pulse oximetry screening does not rule out all important congenital heart disease – The 1 week old infant in your office still may have congenital heart disease Findings at 1 Week Check Up ♥ In the 1st week of life concern for cardiac disease (tachypnea, cyanosis, poor pulses) requires immediate evaluation Because of the potential for a duct-dependent lesion Online Resources • CDC – http://www.cdc.gov/ncbddd/pediatricgenetics/CC HDscreening.html • Children’s National Medical Center – http://www.childrensnational.org/PulseOx • Congenital Heart Public Health Consortium – http://www.chphc.org • Indiana State Department of Health – http://www.in.gov/isdh/25347.htm