PowerPoint_Format
advertisement

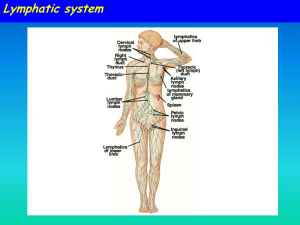
The Single Ventricle Karim Rafaat, M.D. The title “single ventricle” includes those lesions designated as both HLHS HRHS HLHS is far more common, and the strategy for palliation of both lesions similar, so I will not mention HRHS HLHS - History First described in 1952 by Lev as the pathologic complex “hypoplasia of the aortic tract”, included cases of: hypoplasia of the aorta and VSD hypoplasia of the aorta with aortic stenosis or atresia, with or without mitral stenosis or atresia In 1958, Noonan and Nadas termed these lesions as “hypoplastic left heart syndrome”. Embryology The embryologic cause is not fully understood. It probably results from a limitation of either LV inflow or outflow, such as the development of severe AS early Decreased antegrade flow through LV most common cause is mitral atresia decreased division of cardiac myocytes Genetics Familial inheritance: Autosomal recessive and multifactorial inheritance have both been postulated. Sibling recurrence risk: 0.5% Sibling recurrence for all other cardiac malformations: 2.2% Definable genetic disorder (28%): Turner Syndrome Noonan Syndrome Trisomy 13, 18, 21, or other microdeletion syndromes Epidemiology Uniformly lethal prior to 1980 Each year, approximately 1000 infants with HLHS are born in the US. Prevalence: 1 per 6000-7000 live births. In pathologic series, it accounts for 1.4-3.8% of congenital heart disease. Third most common cause of critical CHD in the newborn. 23% of all neonatal mortality from CHD Male predominance: 57-70%. Anatomy Underdevelopment of the left side of the heart atresia of the aortic or mitral orifice hypoplasia of the ascending aorta. The left ventricle may be small and nonfunctional or totally atretic Pulmonary venous return from LA to RA through a large PFO or ASD Systemic venous blood mixes with pulmonary venous blood in the RA and RV RV ejects blood into a large MPA Systemic circulation is supplied in parallel with pulmonary circulation through a PDA Multiple obstructions to systemic flow Aortic valve atresia Arch hypoplasia Place systemic flow at risk Blood flow to the coronary and cerebral circulations is retrograde Usually little or no flow through aortic valve Postnatal decline in PVR places systemic, and especially the ductal dependant and retrogradely supplied coronary and cerebral vascular beds at risk for hypoperfusion secondary to pulmonary run-off Pathophysiology Relative Qp and Qs determined via resistances of respective vascular beds Ventricle must supply both Qp and Qs Single right ventricle has at least twice the volume load of an in series ventricle Significantly volume overloaded The aim of initial management is to optimize Qp and Qs in a manner that provides adequate end organ oxygen delivery without overloading the single ventricle Remember my last lecture? This balancing act is only temporizing and serves to allow pt to survive to definitive treatment Treatment options Supportive care Only option up to 25 years ago Is still main option of treatment in many countries Staged reconstruction Stage I Norwood Procedure Stage II Bi-directional Glenn or Hemi-Fontan Stage III Fontan Procedure Transplant Goals of Surgery Unobstructed systemic blood flow To maximize oxygen delivery and minimize ventricular hypertrophy Limited pulmonary blood flow To minimize ventricular volume load and the risk of pulmonary hypertension Unobstructed pulmonary venous return To minimize secondary pulmonary artery hypertension Minimize likelihood of pulmonary artery distortion Avoid dysrhythmias All these goals, achieved in a timely fashion, circumvent the major risk factors for poor outcome post-Fontan: Ventricular hypertrophy causing diastolic dysfunction Elevated PVR or pulmonary artery pressure AV valve regurgitation Ventricular systolic dysfunction The reasons why the above hurt the post-fontan heart will be discussed later Stage I – Norwood palliation The goal of the Norwood is to stabilize and balance the parallel circuit, protect the pulmonary vascular bed and preserve ventricular function Adequate oxygen delivery allows for the growth necessary for a hemi-fontan or BDG to be performed Native ascending and transverse aortic arch is incorporated into a neoaorta Neo-aorta created by augmenting native arch with autologous pulmonary homograft Neo-aorta is attached to the proximal pulmonary artery trunk Neo-aorta provides systemic outflow Important that the neo-aorta is free of obstruction Obstruction is poorly tolerated by the single ventricle and is associated with increased interstage mortality Distal MPA is closed Pulmonary flow is provided by a restrictive shunt from the right innominate artery to the RPA Modified BTS Post-Norwood Anatomy Post-Norwood issues The hope is that now RBTS + Rp = Rs So the circulations are balanced and volume work is minimized Meaning for a given required Qs, total Q can be less as the ratio is more favorable But…… The ventricle has just been through hypothermic cardiopulmonary bypass with myocardial ischemia/arrest Vascular endothelium of the systemic and pulmonary circulations have also been subjected to bypass and injury Combined effect is a systemic inflammatory and adrenergic stress response The ventricle can also exhibit a low cardiac output syndrome in the first 12-24 hours post op All vascular beds show signs of endothelial dysfunction Evidenced by increased resistance This may tip the balance of flow towards the pulmonary circulation Systemic oxygen demands may be unable to be met by the post-op ventricle Leading to anaerobic metabolism, acidosis and worsening function LCOS Low Cardiac Output Low systemic cardiac output can be due to Globally decreased ventricular function Elevated Qp:Qs AV valve regurgitation How to discern between the above? Echocardiography Evaluates pump function and rules out AV valve regurg Arterial-venous oxygen saturation difference An A-V DO2 more than 40% suggests inadequate tissue delivery of oxygen and low systemic cardiac output OR…Lactate level plus base deficit Good echo function plus high A-V DO2 = Qp>Qs Treatment One must pay attention to both TOTAL CO and the Qp:Qs ratio The ratio can be altered by maneuvers discussed in my last talk Total CO can be increased by careful selection of vasoactive agents Want to avoid tachycardia and increasing afterload Milrinone Nesiritide Dopamine Hypoxemia Pulmonary Venous desaturation Atelectasis pulmonary edema pneumothorax Systemic venous desaturation Anemia Low cardiac output Decreased pulmonary blood flow Elevated PVR Pulmonary venous hypertension Pulmonary artery distortion Restrictive systemic to pulmonary shunt Gotta rule out the top two, then, think about echo or cath to rule out the anatomic causes Which need a surgeon…. Coronary circulation Single right ventricle coronary blood flow occurs predominantly in diastole Like an in series LV When pulmonary flow is supplied by a shunt from a systemic artery, increases in SVR lead to increased pulmonary flow, and increased diastolic pulmonary run-off This can lead to myocardial ischemia….and sudden death Which is why “Leaving a kid in Norwood physiology is like taking a walk through Watts at midnight” Dr. Cocalis The Wall of Wo Sudden death post Norwood Unpredictable and sudden Experienced centers report survival between 63-94%1 Inter-stage mortality of 10-15%2 Rapid fall in PVR, or increase in SVR Steal from coronary arteries lower pressure in pulmonary circulation throughout cardiac cycle The Journal of Thoracic and Cardiovascular Surgery 2003;126(2) 504-509 Arch Dis Child Fetal Neonatal Ed 2005;90:F97-102. • Bartram et al, Causes of Death after the Modified Norwood procedure: A study of 122 postmortem cases, Ann Thorac Surg, 1997 122 cases over 15 years The leading causes of death largely correctable surgical technical problems associated with perfusion of the lungs (36%), of the myocardium (27%), and of the systemic organs (14%). The proposed solution to surgical manipulation of the coronary arteries the pulmonary diastolic run-off through the modified BTS Is an RV to PA conduit First described by Norwood in 1981 Reintroduced by Japanese surgeon Sano in the late 1990’s The Sano modification Directly supplies pulmonary flow via the RV Aortic diastolic runoff does not occur Post-op diastolic BP is higher Coronary perfusion is improved Blood flows only during systole Reducing total pulmonary blood flow Improves Qp:Qs, thus protecting pulmonary vascular bed and decreases volume load on the RV, giving it a greater chance to return to normal size and function Less distortion of the pulmonary arteries than is seen with a BTS Improved growth of PA’s Trade off’s Ventriculotomy Increases potential for low cardiac output syndrome The damage to the ventricular wall may be offset by the better coronary perfusion….. Increased volume load secondary to reversed diastolic flow in a nonvalved conduit Possibility of shunt occlusion Concern of RV arrhythmias post ventriculotomy Not confirmed by present studies, though Januszewska et al, RV to PA shunt and modified BTS in preparation for hemi-Fontan procedure in children with HLHS, European Jour Cardiac Surg, 27, 2005 78 children – 27 underwent Norwood with BTS 51 underwent Sano modification Those who underwent Sano, at time of hemi-fontan Larger pulmonary arteries Which means lower resistance to the passive flow that will be supplying the lungs after the BDG or Fontan Less RVH Better diastolic function, and so lower filling pressures required Lower Qp:Qs (0.8 vs 1.27) Less pulmonary vascular remodeling and less ventricular volume load Pizzaro et al, Right Ventricle to Pulmonary Artery Conduit Improves Outcome after stage I Norwood for HLHS, Circulation, 2003; 108 Retrospective cohort review 36 RV to PA conduits 20 BTS Those with RV to PA conduits Higher diastolic BP Lower PaO2 Indicating lower Qp:Qs secondary to less diastolic run-off Less ventilatory manipulations were required for Qp:Qs management 33/36 survived to BDG vs 14/20 in the BTS group Other Considerations Risk for shunt occlusion Low sats lead to high Hct’s, which increases risk of thromboembolic complications Need to be well hydrated Shunt failure Slowly occurs as pt grows, but shunt does not Leads to slowly progessive cyanosis as oxygen consumption increases in a growing pt VENOUS ACCESS Any venous embolus may reach systemic vascular beds Watch for air bubbles, clots, meticulously…. Glenn Hughes – A Village Person Bidirectional? Stage II – Partial Cavopulmonary Anastomosis After stage I, there are two problems Cyanosis Excessive ventricular volume load The Fontan fixes both of the above, but must come after an intermediate step… Why? Reasons for a staged repair The fontan requires low PVR to allow for passive pulmonary flow PVR does not reach nadir until 6-8 months Furthermore, following the high Qp:Qs state of prenorwood, the pulmonary vasculature can be reactive Which is exacerbated by the stress of bypass The parallel circulation single ventricle is relatively hypertrophied and dilated secondary to volume overload Shifts Frank-Starling curve down and to the right Means the norwood ventricle is very volume sensitive A loss of ventricular filling secondary to increases in PVR would lead to critically decreased CO The solution is a staged procedure that allows for more gradual ventricular unloading and remodeling Also allows for adjustment of the upper body venous and lymphatic systems to deal with an increase in venous pressure prior to the Fontan Usually performed around 4-6 months of age Bidirectional Glenn The RV/PA or BT shunt is removed This volume unloads the ventricle Critical in improving outcome in single ventricle palliation SVC is anastomosed end to side with the RPA Is more compatible with an extracardiac fontan procedure down the line Hemi-Fontan Similar to BDG physiologically Has additional proximal SVC and inferior RPA anastomosis RA communication closed with a patch More suited for eventual lateral baffle Fontan Stage II Physiology Half the blood to the heart comes from the IVC, half from the pulmonary veins Qp:Qs is now 0.5 SaO2 about 75-85% Infants with bigger heads have higher sats Excessive volume load is now eliminated Ventricle now pumps only Qs Decreased cavity dimension and increased wall thickness improves tricuspid function Preload is not critically dependant upon unimpeded pulmonary flow Increases in PVR won’t significantly affect systemic circulation Qp driving force is now SVC pressure Qp must pass through two highly regulated vascular beds Pulmonary and cerebral Transpulmonary pressure gradient Mean pulmonary arterial pressure – mean atrial pressure Represents the driving force through the lungs Low PVR allows for a low delta P Which means lower SVC pressures Pulmonary flow can be impaired by High PVR Increased atrial pressures AV valve dysfunction Ventricular diastolic dysfunction A low transpulmonary gradient with a good CO means good things for sleep…. Post-Op issues – Ventilator Management Excessive Paw will limit systemic venous return via increased intrathoracic pressure increase PVR, potentially decreasing pulmonary flow AND increases SVC pressure Minimize iT, PIP and choose PEEP that allows for maintenance of FRC Remember that Qp comes through the cerebral vascular bed… So maneuvers like alkalosis and hyperventilation to decrease PVR may INCREASE cerebral vasc resistance, decreasing flow and further exacerbate hypoxemia Low Cardiac Output Low systemic cardiac output can be due to Globally decreased ventricular function Elevated Qp:Qs AV valve regurgitation Loss of AV synchrony Low Cardiac Output Careful choice of inotropes Passive pulmonary blood flow occurs mostly during diastole Tachycardia is bad Alpha agonists work on both pulmonary and systemic vascular beds Increase in PVR will decrease preload Increase in SVR increases afterload Both bad in the post-op single ventricle Low dose dopamine and milrinone are good choices Elevated SVC Pressure As evidenced by upper compartment plethora and edema DDx Obstruction at anastomosis Pulmonary artery distortion Elevated PVR Elevations in SVC pressure limit cerebral blood flow CPP = MAP – SVC pressure Combined with hyperventilation / alkalosis to maintain low PVR, perfusion decrease is more marked Prolonged SVC pressure elevation can lead to cerebral edema, worsening the above 3% NaCl / Mannitol Hypoxemia Three broad categories of cause: Pulmonary Venous desaturation Systemic venous desaturation Decreased pulmonary blood flow I just brought these up again because I like the organization of thinking here…I’m trying to ram this one home.. Dis ees a fontan Stage III - Fontan The final step in single ventricle palliation When is the stage II patient ready? Usually about 6 months following stage II Increasing growth and activity increases venous return from lower limbs When the ventricle has remodeled and displays good function on echo Good AV valve function Small transpulmonary pressure gradient Low ventricular end diastolic pressure Most centers aim for completion between 12-24 months of age Lateral baffle Blood from IVC directed into RPA via a baffle in the lateral portion of the RA If the preceding operation was a hemifontan, then IVC to RPA continuity is achieved by removing the RA patch Extracardiac Fontan A conduit of PTFE tubing or aortic allograft is placed between IVC and RPA Advantages Limited bypass Atrial arrythmias less common Disadvantage Conduit cannot increase in size as pt. grows In both operations, poor ventricular compliance or increased PVR is a concern Both lead to decreased pulmonary flow, and, possibly, decreased preload Often a fenestration is left in the baffle or conduit When systemic venous pressure increases, increased shunting of blood through the fenestration occurs Maintains cardiac output when it is compromised by decreased pulmonary venous return Fontan Physiology Qp:Qs is equal Ventricle supplies Qs Systemic venous pressure drives Qp Shunt through fenestration lowers SaO2 slightly Pulmonary flow is nonpulsatile Increases pulmonary vascular bed impedance Decreases capillary recruitment Flow through pulm vasc bed dependant upon those factors that lend to a low transpulmonary pressure gradient Good ventricular systolic and diastolic function AV valve competence Low PVR Elevated pulmonary artery pressures leads to higher fluid replacement to maintain high SVC pressures Third spacing leads to effusions, ascites Acsites increases required ventilator pressures, decreases renal perfusion Post-Op Issues - Ventilator Management Pulmonary flow is impeded by a high PVR Positive pressure ventilation increases PVR PEEP in excess of that required to maintain FRC increases PVR Minimal PEEP Aim is usually to allow pt to do as much of the work of breathing as possible Low set rate with high PS Low Cardiac Output Discerning cause made easier by “physiologic” RA and LA lines SVC/RPA and common atrial pressure lines Low Cardiac Output Causes Inadequate preload Low SVC and atrial pressures Elevated PVR High SVC and low atrial pressure Anatomic obstruction Low atrial and high SVC pressures Pump failure High SVC and atrial pressures Can be due to AV valve regurgitation Ventricular dysfunction Loss of A-V synchrony Ventricular outflow obstruction Poor CO can lead to acidosis Acidosis contributes to increased PVR, leading to further desaturation, worse O2 delivery, more acidosis….etc Careful use of vasoactive agents that increase pump function without increasing afterload Milrinone Dopamine nesiritide Cyanosis AGAIN…… Pulmonary Venous desaturation Atelectasis pulmonary edema pneumothorax Systemic venous desaturation Anemia Low cardiac output Decreased pulmonary blood flow Elevated PVR in those with fenestration Pulmonary venous hypertension Arrhythmias Atrial and ventricular pacing wires are in place Loss of AV valve synchrony is bad Decreases CO, increases required transpulmonary pressure gradient Given the extent of this lecture, and how vast a subject arrythmias are…… You got the wires….and the box…figure something out. Usual bothersome arrhythmias are atrial in nature, so pacing the atria at a rate higher than the intrinsic rate will fix the issue Same goes for a fast junctional rate…. References Chang et al, Pediatric Cardiac Intensive Care, LWW, 1998 Schwartz S et al, Single Ventricle Physiology, Critical Care Clinics 2003;19:393-411 Walker SG, et al, Single Ventricle Physiology – Perioperative implications, Seminars in Ped Surg, 2004, 188-202