Katherine Supiano, MSW PhD
advertisement
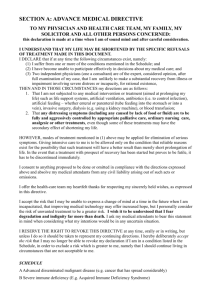
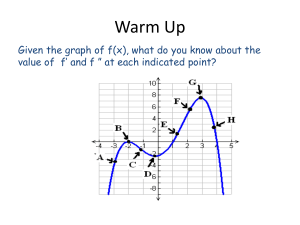
The Continuum of Advance Care Planning Kathie Supiano, PhD, LCSW Associate Professor University of Utah College of Nursing Effective Communication: The intersection between empathic listening & imparting knowledge that creates a respectful, productive professional relationship. Advance Care Planning The process that aims to inform and facilitate medical decision making that reflects patients’ preferences in the event that patients cannot communicate their wishes. Communicating effectively with patients and families has been regarded as a core skill in Palliative Care. • Assurance that medical information and treatment options are conveyed in ways patients and families comprehend intellectually and process psychologically. • Care plans and goals of care are continually evolving, and communication methods must address the reality of change at inflection points the disease process. The trajectories of chronic illness: • Provide parameters for discussion, and • Identify disease inflection points Communication responsibilities in palliative care • Know the patient’s medical issues; options of care and the possible outcomes of each. • Know the patient: personal history, values, hope and goals. • Inform the patient with honesty, cultural awareness, sensitivity, and conveying a sense of presence and accessibility. • Guide (vs. direct) the process of decisionmaking. Questions to begin the conversation • What is your understanding of your present state of health? • What decisions have you made thusfar? Leading to….. • What are your goals of care? • What is your definition of quality of life? Common expressions stated in goals of care discussions: • • • • • “No heroics.” “Don’t keep me alive if I am a vegetable.” “Don’t keep me alive on machines.” “If I am terminal, let me go.” “Do nothing.” Explore these statements further and invite the patient to clarify meaning Discussion of goals of care with a healthy adult • Surrogate decision maker. • Goals of care if one permanently loses ability to know who and where they are. • Any conditions considered worse than death. • Identify who will be available to care for individual, and under what circumstances. • Any religious or cultural personal beliefs that influence EOL treatment preferences. www.gundluth.org/eolprograms Discussion with adult with new, life-limiting condition • To begin or continue life-sustaining treatment if: • No longer able to think for self, recognize others or communicate. • Permanently dependent for all needs. • Permanently unconscious or vegetative state. • Functional status, co-morbidities, or very advanced age. Caring Conversations-Making your wishes known for End of Life care www.practicalbioethics.org Center for Practical Bioethics, Kansas City, MO Discussion with an adult with a chronic, progressive disease • How to balance living longer with quality of life; looking forward to any special events. • Any concerns or worries about disease or needs of caregivers. • Any needs, services, information required for current or anticipated care. • The meaning of what it is to live well now or in future circumstances. www.gundluth.org/eolprograms Discussion with adult with end-stage disease; anticipated death in the next year • Any story/experience with end-of-life care. • Any activities that are important to maintain or fulfill. • Consider when to proceed with lifesustaining treatment and/or move toward focus of comfort. • Desired location of death, funeral preferences identified. www.gundluth.org/eolprograms Benefits versus Burdens Benefits can be defined as: • Effective in prolonging life. • Effective in restoring/maintaining function. • Promotes goals/values of patient. • Consistent with religious/cultural beliefs. Benefits versus Burdens Burdens can be defined as: • Results in more or intolerable pain/symptoms. • Damaging to body image or function. • Psychologically harmful. • Unacceptable cost for the patient. “I felt it shelter to speak to you.” Emily Dickinson