Business and Financial Implications - 508 compliant
advertisement
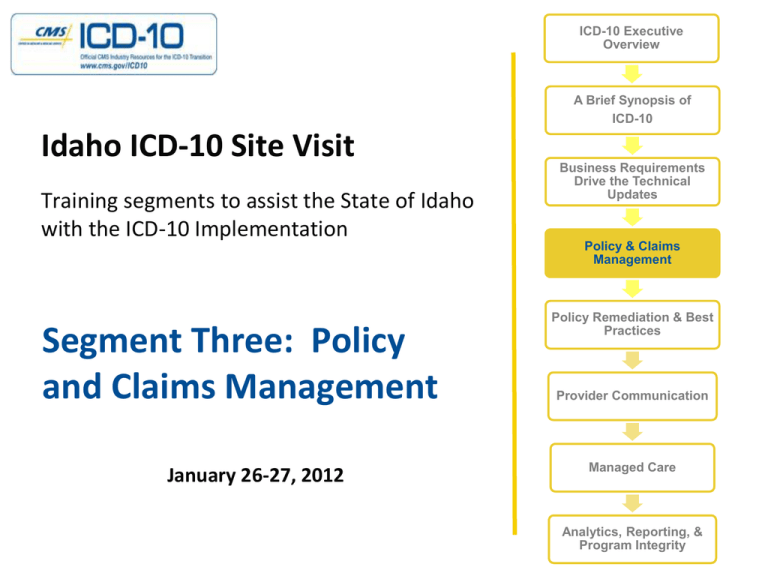
ICD-10 Executive Overview A Brief Synopsis of ICD-10 Idaho ICD-10 Site Visit Training segments to assist the State of Idaho with the ICD-10 Implementation Segment Three: Policy and Claims Management January 26-27, 2012 Business Requirements Drive the Technical Updates Policy & Claims Management Policy Remediation & Best Practices Provider Communication Managed Care Analytics, Reporting, & Program Integrity Introduction Impact to SMA Pharmacy Benefit Management Disease Management Programs BCCPTA and HIV/AIDS EPSDT Third Party Liability Impact to DRG Claims Management 1 Impact to SMA Claims Processing Product Development Enrollment Management Processing claims during the transition period Reimbursement / Network Management Customer Service Care Management Quality Management 2 3 Pharmacy Services Claims processing assistance Drug coverage and payment information Eligibility issues or inquiries Plan limitations Coordination of benefits Prior authorization status 4 Highlights of Changes PDL What’s New in Pharmacy 5 Therapeutic Criteria for Growth Hormone 6 Therapeutic Criteria for Growth Hormone (cont.) 7 UNIVERSAL PRIOR AUTHORIZATION FORM ICD -10 8 Strattera Authorization Form DX Impact 9 10 Diabetes Management 11 Data Collection Document DX Impact? 12 Data Submission Instructions Column Heading Description Requirement Field Length 13 · Added azilsartan to “Angiotensin II inhibitors” description in Table CDC-L. Performance Measurement · Added aliskiren-hydrochlorothiazide-amlodipine to the “Antihypertensive combinations” description in Table CDC-L. Example - Comprehensive Diabetes Care (CDC) · Clarified BP Control criteria for the Administrative Specification. · Clarified that members who meet the Optional Exclusion criteria must be excluded from the denominator for all rates, if optional exclusions are applied. · Clarified reduction of sample size in the Hybrid Specification. The Comprehensive Diabetes Care (CDC) measures are often · Clarified that “Documentation of a renal transplant” meets criteria for the Medical attention for nephropathy used by State Medicaid Agencies to determine performance indicator. Description The percentage of members 18–75 years of age with diabetes (type 1 and type 2) who had each of the following. · Hemoglobin A1c (HbA1c) testing · LDL-C screening · HbA1c poor control (>9.0%) · LDL-C control (<100 mg/dL) · HbA1c control (<8.0%) · Medical attention for nephropathy · HbA1c control (<7.0%) for a selected population* · BP control (<140/80 mm Hg) · Eye exam (retinal) performed · BP control (<140/90 mm Hg) * Additional exclusion criteria are required for this indicator that will result in a different eligible population from all other indicators. This indicator is only reported for the commercial and Medicaid product lines. Eligible Population Diagnosis and procedure codes are used to determine both the Product lines Commercial, Medicaid, Medicare (report each product line separately). denominators and numerators Ages 18–75 years as of December 31 of the measurement year. The measurement year. Source:Continuous National Committee for Quality Assurance (NCQA). HEDIS 2012 Volume 2: Technical Specifications. enrollment 14 15 Asthma Management Distribution of Primary Payor for Asthma Hosp., Illinois 2007 Age Distribution of Medicaid Recipients with Asthma, Illinois, 2006 Data Source: Inpatient Hospital Discharge Data, Office of Policy, Planning and Statistics, IL Dept. of Public Health, 2007 Source: Medical Data Warehouse, Illinois Dept. of Healthcare and Family Services, 2006 16 " Use of Appropriate medications for People With Asthma (ASM) ICD-10 Diagnosis Code Recommendations Table "Description (HEDIS Table)" Type ICD-10 Diagnosis Code Recommendations ICD-10 Code Code Definition Table Description Type ICD-10 Code Code Definition Recommendation (HEDIS Table) ASM-A Asthma Diagnosis asthma J45.3 ASM-A J45.3Asthma Mild persistent Diagnosis Mild ASM-A Asthma Diagnosis J45.4persistent Moderate persistent Add asthma ASM-A Asthma Diagnosis J45.5 Severe persistent ASM-A Asthma Diagnosis J45.4 Table Description Type ICD-10 Code Code Definition Moderate persistent Add (HEDIS Table) ASM-A Asthma Emphysema Diagnosis J45.5 Severe ASM-E Emphysema Diagnosis J43 ASM-E COPD Diagnosis J44 Other chronic obstructive pulmonary Use of Appropriate medications for People With Asthmadisease (ASM) persistent Add ASM-E Emphysema Diagnosis J68.4 Chronic respiratory conditions due to fumes and Table "Description (HEDIS Table)" Type vapors Code ASM-E Emphysema Diagnosis J68.8ICD-10 Code Other respiratory conditions dueDefinition to chemicals, Recommendation gases, fumes and vapors ASM-E Emphysema Diagnosis Interstitial emphysema Diagnosis J43 ASM-E J98.2Emphysema ASM-E Emphysema Diagnosis J98.3 Compensatory emphysema Add Emphysema ASM-E Cystic fibrosis Diagnosis E84 Cystic Fibrosis ASM-E COPD Diagnosis J44 Other ASM-E Acute respiratory failure Diagnosis J96.0 Acute respiratory failure chronic obstructive pulmonary disease Add ASM-E Emphysema Diagnosis J68.4 Chronic respiratory conditions due to fumes and vapors Add ASM-E Emphysema Diagnosis J68.8 Recommendation Add Add Add Recommendation Add Add Add Add Add Add Add Add 17 Prescriptions to ID Members with Diabetes ICD-10 CM 18 ICD-10 Codes to ID Diabetes ICD-9 CM Description 250 ICD-10 CM Diabetes mellitus without mention of E119 complication, type II or unspecified type, not stated as uncontrolled 357.2 Polyneuropathy in diabetes 362.01 E1042 E11.319 Diabetic retinopathy 36641 Diabetic cataract E1136 648.0 Diabetes mellitus of mother, O24319 complicating pregnancy, childbirth, or the puerperium, unspecified as to episode of care or not applicable Description Type 2 diabetes mellitus without complications Type 1 diabetes mellitus with diabetic polyneuropathy Type 2 diabetes mellitus with unspecified diabetic retinopathy without macular edema Type 2 diabetes mellitus with diabetic cataract Unspecified pre-existing diabetes mellitus in pregnancy, unspecified trimester 19 Better health for people, better health for populations, and better value for consumers. Triple Aim VBP * * Value-Based Purchasing Care Management Coverage (e.g. Drug Coverage) Person-Centered Benefits (e.g. HIX) Program Integrity (e.g. deterrence of Fraud, Waste, and Abuse) Health Information Technology (HIT) ICD-10 Eligibility & Enrollment Benefits & Coverage Payment Figure 1. ICD-10 as a Foundation for Initiatives to Achieve the Triple Aim Breast and Cervical Cancer Prevention and Treatment Programs 21 SMA - Policies for HIV/ AIDS ICD-10 Impact on Eligibility - State Medicaid programs should update their business rules to reflect expanded eligibility criteria. ICD-10 Impact to Benefits - State Medicaid programs should update their business rules and benefit package codes to reflect these medical necessity criteria ICD-10 Impact on Operations - Due to the increased detail contained in the codes, SMA policies will be impacted ICD-10 Impact on Reimbursement - ICD-10 codes will contain information to assist in the reimbursement of claims based on the stage of HIV or 22 DX Codes - HIV / AIDS ICD-9 DESCRIPTION ICD-10 DESCRIPTION 042 Human immunodeficiency virus (HIV) disease B20 Human immunodeficiency virus (HIV) disease 795.71 Inconclusive human R75 immunodeficiency virus [HIV] test (adult) (infant) Inconclusive laboratory evidence of human immunodeficiency virus [HIV], 647.81 Other specified infectious and parasitic diseases of mother with delivery, in which HIV is not even identified as the root disease in the ICD-9 code, O98.711 HIV disease complicating pregnancy, first trimester O98.712 HIV disease complicating pregnancy, second trimester O98.713 HIV disease complicating pregnancy, third trimester 23 Emotional, Mental and Behavioral health 24 Mental Health – Coding Example ICD-9-CM Diagnosis Code: 319.0 ICD-10-CM Diagnosis Code: F79 Unspecified mental retardation Unspecified mental retardation • subnormal intellectual functioning which originates during the developmental period; multiple potential etiologies, including genetic defects and perinatal insults; intelligence quotient (IQ) scores are commonly used to determine whether an individual is mentally retarded; IQ scores between 70 and 79 are in the borderline mentally retarded range and scores below 67 are in the retarded range. • Impaired intellectual (IQ below 70) and adaptive functioning manifested during the developmental period. Use a more specific term if possible. Use for both the concept of the disorder itself and for populations of mentally retarded persons. • . F79 is a billable ICD-10-CM code that can be used to specify a diagnosis. Applicable To • Mental deficiency NOS • Mental subnormality NOS 25 DSM IV & ICD-10 DSM IV was designed to correspond with codes from the ICD The most recent edition is called DSM-IV-TR and incorporates changes made to some criteria sets in order to correct errors identified in DSM-IV "Comparing the two most visible diagnostic systems, it found that ICD-10 was more frequently used and more valued for clinical diagnosis and training and that DSM-IV was more valued for research."1. 26 DSM V & ICD-10 Timeline for implementation extended – May 2013 Major Changes: Inclusion of dimensional assessments for depression, anxiety, cognitive impairment and reality distortion that span across many major mental disorders. Gender identity disorder will likely be renamed and placed under a different category, to reflect the modern reality that it is rarely considered a sexual dysfunction. Introduction of new disorders – Hoarding maybe added to the category of obsessive-compulsive illness as its own disorder. 27 Comparison of Codes DSM-IV Description ICD-9-CM Description ICD-10 Description 295.20 Schizophrenia, catatonic type 295.2 Catatonic type F202 Catatonic schizophrenia 295.30 Schizophrenia, paranoid type 295.3 Paranoid type F200 Paranoid schizophrenia 295.40 Schizophreniform disorder 295.4 Acute schizophrenic episode F2081 Schizophreniform disorder 296.2 major depressive disorder, single episode 296.2 F329 300.00 anxiety disorder NOS 300.00 major depressive disorder, single episode anxiety state, unspecified Major depressive disorder, single episode, unspecified Anxiety disorder, unspecified F419 28 29 Managing Programs (EPSDT) ICD-10 30 EPSDT Annual EPSDT Report: CMS-416 ICD-10 31 EPSDT Annual EPSDT Report: CMS-416 Report Need Inclusion Exclusion CPT Code 83655 Blood lead test 83655 Blood lead test ICD-9 Code Accompanying V15.86, V82.5 984(.0-.9), e861.5 Crosswalk of Codes: ICD-9 Code V15.86 Personal history of contact with and (suspected) exposure to lead V82.50 Screening for chemical poisoning and other contamination 984.0 Toxic effect of inorganic lead compounds E861.5 Accidental poisoning by lead paints ICD-10 Code Z77.011 Contact with and (suspected) exposure to lead Z13.88 Encounter for screening for disorder due to exposure to contaminants T56.0X1AToxic effect of lead and its compounds, accidental (unintentional), initial No ICD-9-CM code(s) convert to ICD-10-CM E861.5 32 COB / Third Party Liability What will be the impact of ICD-10 considering that Medicaid is payer of last resort? Impact when entity is a non HIPAA compliant entity When primary entity has processing rules (i.e. services span the compliance date, difference in “from date and through date rules” etc.) Differences in mapping rules 33` 34 Diagnosis-Related Groups (DRGs) The Basics DRGs attempt to align actual payment to expected costs by bundling a set of services over a period of time for patients with similar resource intensity and clinical coherence. Additionally, DRGs attempt to adjust payments for cost factors outside of a provider’s control (e.g. inflation and geographic variation in wage rates) The assignment of DRGs and determination of relative payment weight is heavily dependent on inpatient procedures and diagnoses 35 Diagnosis-Related Groups (DRGs) ICD-10 Impact on DRGs Major Surgery … Type of Surgery Minor Surgery Other Surgery O.R. Procedure Major Diagnostic Category Surgery Unrelated to Principal Diagnosis O.R. Procedure Neoplasm Specific Conditions Relating to the Organ System … Principal Diagnosis Specific Conditions Relating to the Organ System Symptoms Figure: Typical DRG Structure for a Major Diagnostic Category Other 36 Diagnosis-Related Groups (DRGs) Moving from ICD-9 to ICD-10 DRGs are based on an analysis of historical information and are typically licensed and maintained by an entity who is responsible for their updates and revisions – But there are no historical information yet for ICD-10 In order to create DRGs for ICD-10, maintainers use clinical and/or probabilistic maps (e.g. CMS’ Reimbursement Map) to use historical ICD-9 data for developing ICD-10 groupers The only ICD-10 grouper that has been publically specified for public review and comparison is the MS-DRG (v26+) Maintainers attempt to make ICD-10 groupers ‘financially neutral’ but this assumes coding conventions will be similar across two very different code sets 37 Diagnosis-Related Groups (DRGs) Crosswalking Matters Reimbursement Map ICD-9 procedure: 3734 - Other Heart Lesion Excision • 427.32 Atrial Flutter • 424.0 Mitral Valve Disorder ICD-10 procedure: 02BH3ZZ – Percutaneous pulmonary valve excision • I481 Atrial Flutter • I340 Nonrheumatic ICD-10 procedure: 02BL3ZZ – Percutaneous excision of the left ventricle • I481 Atrial Flutter • I341 Nonrheumatic mitral insufficiency mitral prolapse DRG 251 Percutaneous cardiovascular procedure w/o stent w/o MCC weight 1.7992 ($10,047) DRG 251 Percutaneous cardiovascular procedure w/o stent w/o MCC weight 1.7992 ($10,047) DRG 230 Other Cardiothoracic Procedures w/o CC/MCC weight 3.5451 ($19,796) 38 Diagnosis-Related Groups (DRGs) Same Case – Different DRG Reimbursement Map A 30 year old male has a repair of the abdominal aorta due to a laceration with damage to surrounding soft tissues of the abdomen from an assault with a knife. ICD-9 procedure: 3931 – Suture of Artery ICD-10 procedure: 04Q00ZZ – Repair abdominal aorta, open approach • 9020 Injury abdominal aorta 86819 Intra-abdominal injury NEC- open DRG 907 Other O.R. procedures for injuries w/ MCC weight 3.8268 ($21,369) S3502XA Major laceration of abdominal aorta… S36899A Injury of other intraabdominal organs… X991XXA Assault by knife… DRG 908 Other O.R. procedures for injuries w/ CC weight 1.9251 ($10,750) 39 Diagnosis-Related Groups (DRGs) Unintended Consequence A 50 year old woman with rheumatoid arthritis is admitted for a right total hip replacement. Patient is noted to have respiratory failure as a secondary diagnosis at the time of discharge, but this was not primary reason for hospitalization. M05651 Rheumatoid arthritis of right hip w involvement of other organs/systems Respiratory failure, unspec, unspec whether hypoxia or hypercapnia DRG 469 Major joint replacement or reattachment of lower extremity w/ MCC weight 3.4724 ($19,390) M05651 Rheumatoid arthritis of right hip w involvement of other organs/systems J9610 Chronic respiratory failure, unspec whether hypoxia or hypercapnia DRG 470 Major joint replacement or reattachment of lower extremity w/o MCC weight 2.1039 ($11,748) ICD-10 procedure: 0SR90JZ – Replacement of right hip joint w synthetic J9690 substitute, open approach ICD-10 procedure: 0SR90JZ – Replacement of right hip joint w synthetic substitute, open approach 40 Diagnosis-Related Groups (DRGs) “Weight” Watchers So, what does this mean? Since ICD-10 DRGs are based on ICD-9 data and coding practice, they do not account for the learning curve or actual use of the new code set This means that we better “watch our weight” - DRG weights that is. We should implement new metrics to monitor DRG weights and assignments to guard against DRG drift. 41 42 Are Providers Coding Correctly? Will provider staff use codes that are most familiar Consider effect if the incorrect code is utilized Will providers collect the appropriate information Challenge of training billers and coders How will they change behaviors and mitigate challenges Are providers aware of SMA plans to comply with regulation 43 MITA Architecture Focus 44 Authorize Referral Description ICD-10 Impacts Used when referrals between providers Referral for specialist may depend must be approved for payment on diagnosis and/or procedure May be performed by Health Examples are to providers for lab Service Contractors (HSCs) procedures and surgery Primarily used in provider network and managed care settings 45 Authorize Service Description ICD-10 Impacts Encompasses both a pre- and postapproved service request Service authorization will depend on diagnosis and/or procedure May be performed by HSCs Focuses on specific types/numbers of visits, surgeries, tests, drugs, Durable Medical Equipment (DME), and institutional days of stay (Primarily used in Fee for Service (FFS) 46 Authorizations Impact to the 278 transaction (5010 initiative) Ensure translation decisions do not cause access to care and/or budget issues Modifications to all prior authorization documents Communication and collaboration 47 Authorize Treatment Plan Description ICD-10 Impacts Treatment plans are created for specific diagnoses Primarily used in care management May be performed by HSCs settings where team assesses Updates to treatment plan as client, completes plan, which priordiagnoses change authorizes providers and services over period of time Encompasses both pre- and postapproved treatment plan 48 Edit Claim Encounter Description ICD-10 Impacts Receives original or adjustment claim/encounter and determines its submission status, validates edits, service coverage, Third Party Liability (TPL), coding; and populates with pricing information Sends validated data to audit process and failed data sets to the remittance advice/encounter report process Diagnoses and procedures are used in claims edits Claims edits, provider allowed services, member coverage, medical necessity, authorization COB Validation of code sets and correct coding Program Integrity (PI) edits Groupers and bundles Pricing of claim/encounter Different processes for encounters 49 Edit Claim 50 Price Claim – Value Encounter Description ICD-10 Impacts Receives a claim/encounter from audit claim/encounter process, applies pricing algorithms, calculates managed care and Primary Care Case Management (PCCM) premiums, decrements service review authorizations, calculates and applies member contributions, and provider advances, deducts liens and recoupment Diagnoses and/or inpatient procedures may impact bundling methodologies (i.e. case rates, DRG, per diem etc.) Responsible for ensuring all adjudication events are documented in Payment History data store and are accessible to all Business Areas 51 Claim Impacts To Consider Claim edits need to be updated to reflect new codes Codes used to determine a covered service require update Policies require remediation Claims processing during the transition period will require monitoring / Dual Processing Claim history will contain ICD-9 and ICD-10 codes; consider impact 52 Claim Impacts To Consider Applications used to look up claims may have to be modified Staff Training Update policies, manuals and procedures to accommodate ICD-10 Develop workarounds 53 Questions 54