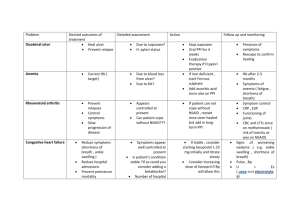
65 with no other risk factors
advertisement
Proton Pump Inhibitors A Curate’s Egg? Dr John O’Malley MA MB ChB MRCGP Join www.pcsg.org.uk Meetings, journal, website access ALL FREE !!!!!!!!!!!!!!! This f***ing egg is off! This is a fantastic drug It has an important role in treating x Why didn’t we realise it has horrendous side effects? PPIs £1 billion NHS costs Globally £40 Billion Pharmacology Unstable at acid ph Parietal cell not stomach activation Act by forming a irreversible bond with cysteine residues in the proton pump Short pharmacological half life Pharmacology 2 But.... Lasts for 24 hours No tachyphylaxis The Proton Pump H2 Antagonists Atropine Proton Pump Inhibitors Text Text Good bits Dyspepsia Reflux Barretts/? Prevention of cancer Prevention of strictures Diagnostic test Upper GI bleeding Ulcer prophylaxis in NSAIDs and aspirin Ulceration/ HP eradication Zollinger Ellison Syndrome And the bad bits? Side effects Slow response Headaches Rashes Diarrhoea Abdominal pain Flatulence Interactions Problems Interstitial nephritis Osteoporosis Vitamin B12 absorption C. Diff and other infections Microscopic colitis Inappropriate investigation and referral And when we should, we don’t Underuse • Gastroprotection • Oesophageal strictures • ? Barrett’s oesophgus Gastroprotection NICE 2001 • Recommendations for patients for whom a regular NSAID is absolutely necessary: • Patients at any age with existing cardiovascular disease, including patients on low dose aspirin: Standard NSAID e.g. ibuprofen, diclofenac or naproxen +misoprostol or PPI if misoprostol not tolerated. • Patients aged 65+ with no cardiovascular risk factors and not onaspirin: • Consider Cox-II selective inhibitor (not sure on that one!) • All other patients i.e. patients < 65 with no other risk factors*: • • Standard NSAID e.g. ibuprofen or diclofenac Risk factors for GI complications with NSAIDs • • Age Previous ulcer, bleed or perforation • Concomitant drug treatment (steroids,anticoagulants, SSRIs) • Co-morbidity (CVD, renal and hepatic impairment, etc.) • Rheumatoid Arthritis • NSAID dosage and duration. HP eradication Maastricht -3 2005 • Chronic NSAID users • Naive NSAID users – test and treat • Long term aspirin users – test and treat • PPI is superior in preventing ulcers Risk of NSAID related gastrointestinal bleeding by age for population 100,000 Age Range Number taking NSAID Number with GI bleed Risk in any one year of a GI bleed due to NSAID Risk in any one year of dying from GI bleed due to NSAID 16-44 2100 1 1 in 2100 45-64 3230 5 1 in 646 1 in 12353 1 in 3800 65-74 2280 4 1 in 570 1 in 3353 75+ 1540 14 Anon. Cox-21 roundup. Bandolier 1 in 110 in 647 2000;75 ACUTE Vs CHRONIC NSAID USE Drug exposure OR (95%CI) for GU OR (95% CI) for DU Non use 1 1 Acute use 4.47 (3.19-6.26) 2.39 (1.73 – 3.31) Chronic use 2.80 (1.97 – 3.99) 1.68 (1.22- 2.33) SSRIs AND UGIH • “Our meta-analysis shows that SSRIs • more than double the risk of UGIH and • concomitant NSAID use increase the risk • of UGIH by 500%” Loke et al. Alim. Pharm. Therapeutics 2007 SSRIs: NUMBER NEEDED TO HARM Patient population Baseline upper GI Event Rate NNH per year with SSRI ( 95% CI) NNH per year with SSRI AND NSAID( 95% CI) Unselected >50 23 years 318 (152- 979) 82 (41-181) No previous ulcer drug use or hospitalisation Ulcer drug 18 411 (196- 1266) 106 (52-233) 42 177 (85-545) 46 (24- 101) Hospitalisation 62 121 (58 – 370) 32 (17-69) Ulcer drug use and hospitalisation 108 70 (34 -214) 19 (10-41) SSRIs and NSAIDs Do PPIs work? Drug Risk of UGIB NSAID 5.3 Rofecoxib 2.1 Paracetamol 0.9 NSAID and PPI 0.9 Number needed to treat to avoid a peptic ulcer in elderly NSAID/aspirin users........... 3 Compliance - GPs “In individual studies in primary care adherence to prescribing guidelines varied from 9% to 27%.” Compliance - patients “...adherence to NSAID plus PPI or H2RA declined rapidly, so that after 6 months the majority of patients were not taking gastroprotection prescribed.” Moore et al. BMC Musculoskeletal Disorders 2006; 7:79 Cost Resource Mean cost £ Minimum Maximum Diagnostic endoscopy Therapeutic endoscopy GI opd Surgical procedure Rebleed costs 435.38 282.68 650.67 1158.61 682.1 1532.73 72 3181.80 50 1731 84 3804.13 17025 14619 19964 Omeprazole cost • 28 days of 20mg/day =£1.62 Conclusion • Right person with the right drug gives the right outcome Problems Interstitial nephritis Osteoporosis Vitamin B12 absorption C. Diff and other infections Microscopic colitis Inappropriate investigation and referral Interstitial nephritis Interstitial nephritis 15% of all acute admission with acute kidney damage Immune mediated? Can lead to severe kidney damage Who checks kidney function? Osteoporosis UK study (GPRD) 13,556 patients with hip fracture Risk 1.4 after using PPI for >1 year Risk 2.65 if long term high dose Causal? Reduces absorption of dietary calcium Inhibits magnesium absorption Also inhibit osteoclasts ? Prevent osteoporosis Coincidental? Iron deficiency Iron absorption ? Long term, high dose PPI link Theoretical but not proven Vitamin B12 Deficiency B12 bound to protein Pepsin needed B12 levels reduced but significant deficiency? Infections PPI use and Salmonella/ campylobacter Clostridium Difficile infection Gram positive bacteria Anaerobic spore forming Severe diarrhoea Can lead to pseudomembranous colitis Toxic megacolon Absent gut flora PPI problems Often taken as antacids Not all reflux is acid Misdiagnosis 50-60% of PPI scripts there is no or an inappropriate reason for prescribing £100 million in the NHS wrongly prescribed £2 billion worldwide Decrease in price but increase use has increased costs PPIs make up 90% of the drug budget for dyspepsia 63% 33% 67% NICE NICE Guidance 2000 Treat with healing doses then step down Shortest length of treatment with smallest dose No long term use without definitive diagnosis NICE Dyspepsia Guidelines 2004 Check if PPI needed Lifestyle advice Avoid precipitants Educate Review need So who do we need to treat more? Who should we treat more? NSAID Aspirin And who less? Rebound hyperacidity Prolonged treatment Increased parietal cell mass Peaks at 2 weeks. Problems caused Increased use of PPIs Unwillingness to try step down Gastroscopies Overuse/ wrong use 40% ‘unknown reason’ Mean duration of use 450 days 50% taking drugs that cause or worsen GORD 18% smokers GORD and effect of medication H2 blockers 30-60 minutes PPI 24 hours Step down 42% couldn’t be stepped down 43% reduced need for PPI or changed to antacid/alginate or H2RA 15% stopped completely Lifestyle Lifestyle changes • Obesity • Smoking • Raising the head of the bed • Decrease fat intake ( chocolate, peppermint, garlic and onions) • Large volume meals • Rich energy dense meals • Low dietary fibre • Alcohol decrease Lifestyle • Only reduce severity and frequency • Very few patients do it well • And some don’t want to........ PPIs • Used too much • Used not enough • ‘Lifestyle drug’ Thank you