PRACTICE TRANSITION TO ICD10
advertisement

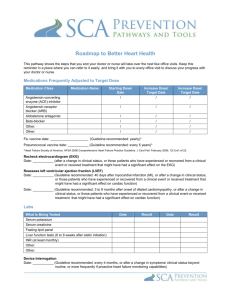
PRACTICE TRANSITION TO ICD10 ADSoyerDO AAOS Practice Management Committee AAOS San Francisco February 10, 2012 Disclosures AAOS Practice Management Committee 2010-12 IMPLEMENTATION OF ICD10 Where to begin? No US tested model in place for implementation Draw on experiences from EMR transition Look at experiences from Canada Challenges to Implementation In addition to ICD 10, HIPAA will be updated from version 4010 to 5010 Overlap between both Will require preparedness for both conversions Impact of ICD Implementation Total Cost Impact Nachimson Advisors, LLC 2008 Small Practice $83,290 Medium Practice $285,195 Large Practice $2.7 million Total Cost Impact Costs Arise from 6 Key Areas 1. Staff Education & Training 2. Analysis of Health Plan Contracts, Coverage Determination & Documentation 3. Changes to Superbills 4. IT System Changes 5. Increased Documentation Costs 6. Cash Flow Disruption Staff Education & Training Clinical & Administrative Staff will require significant time to learn new codes Learned patterns will have to be re-learned because of the changed structure and organization of the code set Business-Process Analysis of Health Plan Contracts Assessment of ICD 10 impact on business processes, including provider health plan contracting Health Plans may modify provider contracts to comply with greater specificity required by the ICD 10 mandate - adjusting payments accordingly Coverage determinations may also be revised in accordance with new diagnostic codes and additional documentation required to support patients’ treatment plans Changes to Superbills, IT System Superbills will need to be changed to support 5x number of codes. Software changes and associated costs to EMR IT costs of ensuring compliance of Practice Management / Billing software and Clearinghouse Vendors with ICD 10 Increased Documentation Costs & Cash Flow Disruption Additional documentation will be required to support the patient’s diagnosis - less time for clinical work = decrease in productivity Health plan payments will be changing based on severity of diagnosis and changes in coverage There may be significant changes in reimbursement patterns disrupting cash flow Total Cost Summary Total Cost Summary Typical Small Practice Medium Practice Large Practice Education $2,405 $4,745 $46,280 Process Analysis $6,900 $12,000 $48,000 Changes to Superbills $2,985 $9,950 $99,500 IT Costs $7,500 $15,000 $100,000 Inc Documentation Costs $44,000 $178,500 $1,785,000 Cash Flow Disruption $19,500 $65,000 $650,000 TOTAL $83,290 $285,195 $2,728,780 Canadian Implementation Experience Implemented in 2001, 12 month trials prior &5 yr transition period completed in 2006 4 phase approach (education/training, IT support, trials, maintenance/ upgrades) Lessons to be learned Dedicated training staff, IT development, Gantt charts Differences:US & Canada Canada has Universal Healthcare Decisions & funding from one source http://library.ahima.org/xpedio/groups/public/documents/ahima/bok3_0055 58.hcsp?dDocName=bok3_005558 ICD 10 & HIPAA version 5010 Obstacles to Implementation: 1. to busy with EMR / meaningful use 2. scarce technical resources 3. some payers systems aren’t ready 4. some vendors systems aren’t ready 5. some clearinghouse systems aren’t ready www.cms.gov › Medicare › Electronic Billing & EDI Transactions ICD 10 Timeline Step 1- Impact Analysis (3-6 months) Step 2-Contact your Vendors (2-3 months) Step 3- Contact your Payers, Billing Service & Clearinghouse (2-3 months) Step 4- Installation of Vendor Upgrades (3-6 months) Step 5- Internal Testing (2-3 months) Step 6- Update Internal Processes (2-3 months) ICD 10 Timeline Step 7- Conduct Staff Training (2-3 months) Step 8- External Testing with Clearinghouses, Billing Service and Payers (6-9 months) Step 9- Make the Switch to ICD 10- Oct 1 2013 www.ama-assn.org/go/ICD-10. Preparation AMA Guide Identify your current systems and work processes in which you use ICD 9 including: - Clinical documentation - Superbills PMS (Practice Management System) EHR Quality reporting Contracts Preparation Talk to your current PMS vendor Questions to ask: Can my current system accommodate data format changes for ICD 10 codes? Will they be upgrading your system to accommodate the new codes? If yes, will there be a fee? When will upgrades be installed? When will implementation be completed? Preparation Talk to your Clearinghouses &/or Billing service Questions to ask: Will they be upgrading your system? If so, When? When can you send test claims (with ICD 10 codes) to see if they are accepted? Preparation Talk to your Payers about possible changes to your contracts from implementing ICD 10 Questions to ask: Do they plan on re-negotiating contracts? If yes, when? At time of renewal or prior? What impact will ICD 10 have on your payment, medical review, auditing and coverage? Preparation Identify potential changes to existing practice work flow and business processes Consider these areas: Clinical documentation Superbills Quality reporting Preparation Identify Staff Training needs Who gets trained & in which areas? Develop program with training leader who in turn trains other staff Resources: http://www.ahima.org/icd10/role.aspx Preparation Budget for Implementation costs - expenses for system changes - practice business process changes - resource materials - training - consultants Recommendations Use your experience from EMR transition to alter workflow & anticipate revenue shortfalls Access to credit line for implementation costs and cash shortfalls post Oct 2013 Utilize your EMR vendor & Clearinghouse tech support- If any doubt in their ability to make seamless transition, NOW is the time to switch. AAOS resources ( e.g Gateway program) Consultant? Thank You Twitter @ ADSoyerDO Email:ADSBONES@gmail.com AdamDSoyerDO@Facebook