Bladder Cancer
Diagnosis and Treatment
Albert McBride, MD, FICS
Epidemiology
Incidence 74,690 new cases in 2014:
• Men 56,390
• Women 18,300
Mortality 15,580 deaths in 2014
• Men 11,170
• Women 4,410
2014
• 71,830 new cases of colo-rectal cancer
2020
• Bladder cancer will be the 3rd most common malignancy in
men
Epidemiology continued
• 90% of bladder cancers in the U.S. are urothelial
cell tumors.
– Squamous cell carcinoma (7%)
– Adenocarcinoma (2%)
Risk Factors
• Risk Factors:
– Age
• M: median – 72
• F: median – 74
– Cigarette smoking: strongest RF
• Attributable risk: 46%
• RR of death from Bladder CA
– Males:
» Current smokers = 3.3; past smokers = 2.1
– Females:
» Current smokers = 2.2; past smokers = 1.9
• Smoking cessation: can reduce risk up to 40%
(ROLE OF PHYSICIANS!)
Risk Factors (continued)
• RF’s continued…
– Chemicals:
• Aniline dyes (color fabrics)
• Cyclophosphamide
– Occupational:
• Aromatic amines (betanaphthylamine, 4-aminobiphenyl, and
benzidine)
• Painting, leather industries, autoworkers, truck drivers, metalworkers,
paper and rubber manufacturers, foundry workers, dry cleaners,
dental technicians, hairdressers, and marine engineers
• 30-50 years after exposure
– Arsenic
• Northestern Taiwan (high water arsenic levels)
– Exposure to herb Aristolochia fangchi in Chinese herbal
weight-reduction supplement
Risk Factors (continued)
•
•
•
•
•
Urinary tract infection - SCC
Chronic irritation (catheters, bladder stones) -SCC
Non-functional bladder – SCC
Schistosoma haematobium (SCC, Egypt)
Radiation
• Lower risk:
– increased fluid intake (still controversial)
• Rationale:
– Increased urine output
– Decreased contact time of carcinogens
– Dilution of carcinogen concentration
– Fruits and vegetables (still controversial)
• Cost Analysis:
– Predicted life-time cost per patient: $99,270$120,684(best case-worst case scenario)
(Avritscher,et al, 2006)
– 5-yr net cost: $1B (7th highest all cancers)
Tumor Genetics
Diagnosis
• Signs and symptoms
– Asymptomatic
– Hematuria: MC (85%)
• AUA’s Best Practice Policy Panel on Asymptomatic
Microscopic Hematuria : at least 3 RBC’s/hpf from 2 of
3 properly collected specimens.
– Irritative voiding symptoms: frequency or dysuria
– Flank pain (hydronephrosis?, ureterovesical jxn
tumor)
• Cystoscopy
– Conventional or white light, “gold standard”
• Disadvantage: flat lesions (CIS) -> incomplete resection ->
recurrence
– Flexible: office procedure, w/w/o fulguration of small
tumors
• Well-tolerated
– Fluorescent cystoscopy: [5-aminolevulinic acid (ALA)]:
• Visualization of tissue w/high metabolic rate
• Improves effectiveness of initial resection in superficial and early
invasive CA
• Comparison vs conventional cystoscopy
– Single-center studies(Denzinger, et al 2007; Filbeck et al, 2002 ) :
» Increased recurrence-free survival
» Lower residual tumor rate
» Overall improved dx
– Multicenter study (Schumacher et al, 2010):
» No difference in terms of recurrence-free and progression-free
survival
• Currently not included in the NCCN nor the updated AUA
guidelines on management of non-invasive bladder cancer
• Imaging
– Staging, pretreatment planning
– CT: essentially replaced IVP in many centers
– MRI: patients with renal failure
• Risk of nephrogenic systemic fibrosis (NSF) from
gadolinium
• More accurate staging
• 85% accuracy (non-invasive vs invasive)
• 82% accuracy (organ-confined vs nonorgan-confined)
• Disadv: overstaging
– Especially after recent biopsy or resection (edema and
hyperemia)
CT scans
• Should include abdomen and pelvis, and be
done with and without contrast.
• May demonstrate extravesical extension, nodal
involvement, or metastases.
• Cannot differentiate depth of bladder wall
invasion and may miss tumors <1cm in size.
CT scan
Fluorescence cystoscopy
Fluorescence cystoscopy
Jacobs et al, 2010
• PET (18-FDG):
– Detection of early mets or lymph node spread
(adv over CT or MRI)
– Increased glycolytic activity in neoplastic cells with
a high metab rate -> increased 18-FDG uptake
– Combined PET/CT imaging (combined PET/CT device):
• Functional findings on PET with anatomic structures shown on CT
• Diagnosis of metastatic disease
– Drieskens et al, 2005:
» Sensitivity: 60%
» Specificity: 88%
» PPV: 75%
» NPV: 79%
– Kibel et al, 2009:
» Prospective study on 43 muscle-invasive bladder cancer patients
w/o mets on conventional CT or MRI:
» Sensitivity: 70%
» Specificity: 94%
» PPV: 78%
» NPV: 91%
» Conclusion: Lower recurrence-free, disease-specific, and overall
survival in patients with positive 18-FDG PET/CT Scans
Staging
• Stage 0: noninvasive papillary carcinoma or CIS
• Stage I: involves lamina propria.
• Stage II: invasion of muscularis propria or microscopic
invasion of perivesical tissue.
• Stage III: macroscopic invasion of perivesical tissue or
invasion of prostatic stroma/uterus/vagina.
• Stage IV: Involvement of pelvic wall/abdominal wall, or
any lymph node involvement or metastases.
Staging
Bladder Cancer: Stage Distribution
• Stage Distribution
‒ Ta, Tis, TI
‒ T2-T4
‒ N+, M+
75%
15%
10%
15% of deaths
85% of deaths
• Progression
‒ 15-20% of patients with NMIBC will progress
‒ 18-45% of patients with MIBC will have metastatic disease
Bladder Cancer: Stage and Prognosis
Stage
TNM
5-yr Survival
Occult N+
0
Ta/Tis
N0M0
95%
5%
I
TI
N0M0
65-75%
5%
II
Ta-b
N0M0
57%
18-27%
III
T3a-4a
N0M0
31%
45%
IV
T4b
N0M0
24%
45%
T any
N+M0
14%
T any
N any M+
Median OS <9 months
Treatment (General Principles)
• TURBT (Transurethral resection of bladder tumor)
– Initial - Diagnostic, prognostic and often therapeutic
• 80 percent of patients with high-risk tumors recur within 12
months
– Repeat: to optimize staging, 2 to 6 weeks after initial
•
•
•
•
•
•
30 percent of T1 tumors will be under staged at initial TURBT
Bulky high-grade Ta tumor
Incompletely resected tumor
Any T1 tumor especially if no muscle in resected specimen
34-76% with residual disease
Divrik et al, 2006: initial only (+ MMC) vs repeat TURBT (+MMC)
– 3-yr recurrence free survival
» Later group had 30% higher survival rate
Treatment
Non-muscle invasive
Goal: prevent recurrence and progression decrease mortality
•
Adjuvant intravesical therapy
– permits high local concentrations of a therapeutic agent
within the bladder, potentially destroying viable tumor cells
that remain following TURBT and preventing tumor
implantation
2010 NCCN guidelines indicate use for:
• low grade Ta recurrences
• High grade Ta and T1 lesions
• CIS: Treatment of choice- Bacillus Calmette-Guerin (BCG)
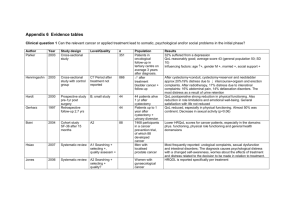
Tx: Non-muscle invasive
Goal: prevent recurrence and progression decrease mortality
– Periop intravesical tx during TURBT
• 2007 Update AUA guidelines
• meta-analysis of 7 randomized trials comprising 1476 patients
(Sylvester, 2004)
–
–
–
–
1 immediate instillation intravesical chemo vs TUR alone
Outcome: recurrence
median follow-up of 3.4 years
Either epirubicin, MMC, thiotepa, pirarubicin:
» Immediately postop or within 24 hours
» No significant difference between chemo agents
– 37% vs 48% (p< 0.0001)
– Contraindications:
» Bladder perforation
» Extensive TURBT
Adjuvant intravesical therapy
BCG immunotherapy
BCG shown to delay tumor progression to more advanced stage,
decrease subsequent cystectomy and increase overall survival
compare to TURBT alone
• 6 randomized trials that included 585 eligible patients with Ta or T1
disease
– TURBT plus BCG had significantly fewer recurrences at 12 months
compared to those managed with TURBT alone (odds ratio 0.30; 95%
CI 0.21-0.43)
• BCG + IFN-alpha combination
‒ Still controversial results
‒ Not yet recommended in NCCN guidelines
Shelley, M.D., Court, J.B., Kynaston, H., Wilt, T.J., Fish, R.G., and Mason, M. (2000). Intravesical Bacillus Calmette-Guerin in Ta and T1 Bladder
Cancer. Cochrane Database Syst Rev CD001986.
• Failure rate (BCG):
– 20-40% recurrence rate
• 35% success rate after 2nd BCG cycle
• ~15% success rate after conventional chemo
(Valrubicin)
Surveillance
• Nonmuscle-invasive
– Cystoscopy + Urine cytology:
• 1st 1-2 yrs: q 3mos
• 3-4 yrs: up to q 6months
• >4 years: annually
– Upper tract imaging: for high-grade tumors
• q1-2 years
Surveillance
• Muscle-Invasive Disease
– 1st 2 yrs:
• Urine cytology, electrolyte and creatinine levels, chest
xray, A/P imaging q 3-12 months
• Urethral washing q 6-12 mos
• Vitamin B12 level annually (continent diversion)
• Cystoscopy, urine cytology and/or bladder biopsies q3-6
mos x 2 years (bladder-sparing protocols)
• Bone scans: only indicated for patients with suspicious
bone pains and advance disease (at least pT3 and pN+)
– After 2 years: as needed
• Tx of Recurrence(Non-muscle invasive):
– 2007 Update AUA Guidelines
• Cystectomy : tx of choice
• Further intravesical therapy (patients who are
poor surgical candidates)
Tx: Muscle-Invasive
• Radical Cystectomy
• Robotic Cystectomy
• Urinary Diversion
• Periop Chemo
Ileal Conduit
Procedure
Figures from Campbell-Walsh Urology, Ninth Edition
Indiana Pouch
Appendix
removed
Right colon is
opened
lengthwise and
folded down to
create a sphere
Figures from Campbell-Walsh Urology, Ninth Edition
Modified Hautmann with Studer Chimney
http://www.sciencedirect.com/science/article/pii/S0022534701642551
• Radical Cystectomy
–
–
–
–
–
Organ-confined muscle-invasive Ca
5 year survival: 45-66%
Operative mortality rate: up to 3%
Complication rate: 25-57% (first month post op)
Surgery alone (failure rates):
• pT2 : 20-30%
• pT3: 40-60%
• pT4: 70-90%
– Delay greater than 12 weeks associated with advanced pathologic
stage and decreased survival
– concensus: should be done within 3 mos of dx of muscle-invasive
disease
– Low- vs high-volume hospitals
– Low-vs high-volume surgeons
– Surgical margin status
– No of LN’s removed: higher -> better survival
• Minimum: 9-20 nodes
• Robotic cystectomy
– Potential advantages:
•
•
•
•
•
Lower blood loss
Less intraop fluid needs
Smaller incisions
Reduced bowel exposure
Greater ergonomics
– Disadvantages:
• Less lymph nodes (controversial)
• Cost
• Urinary Diversion
– Options:
• Neobladder (47%)
– Orthotopic neobladder (50-90% in some centers):
» No need for cutaneous stoma and urostomy appliance ->
decreased physician reluctance and increased patient
acceptance for early cystectomy
– Tissue-engineered neobladder:
» Still under research
» Uses autologous urothelial and smooth muscle cells cultured
on biocompatible synthetic or naturally derived substrates
•
•
•
•
Conduit (33%)
Anal(10%)
Continent cutaneous(8%)
Incontinent cutaneous(2%)
– Factors in choosing method:
•
•
•
•
safety (patient, cancer control)
Complications (short , long term)
Quality of life
Physician experience
• Perioperative chemotherapy
– Rationale:
• 30-50% understaged clinically
• pT3/4 or node positive: >50% failure rate after
cystectomy
– Goal:
•
•
•
•
Downstage
Eradicate micromets
Reduce implantation of circulating tumor cells intraop
Improve survival
– Neoadjuvant Chemo
• Grossman et al, 2003:
– Intergroup 8710 trial
– Cystectomy alone vs neoadjuvant MVAC
(methotrexate, vinblastine, doxorubicin, cisplatin)
– Neoadjuvant gp:
» Higher likelihood of eliminating residual cancer
in the cystectomy specimen(pT0)
» Improved survival
• Adjuvant chemo:
• Insufficient studies for inclusion in latest
recommendations
• Theoretical advantages:
•
•
•
•
Careful patient selection based on P staging
Lack of delay to cystectomy
Alleviation of patient anxiety
Enhancement of chemotherapy against small-volume dse
• Disadvantages:
• Poor tolerance
• Delay in receiving postop chemo due to postop complications
‒ Donat et al, 2009: 30% of patients may have postop complications
that might preclude or delay adjuvant chemo
• Main disadvantages of chemo regimens: Toxic
– MVAC:
•
•
•
•
Severe granulocytopenia
n/v
Stomatitis
Diarrhea/constipation
– Alternative regimens:
• G-MVAC (G-CSF + MVAC): no difference in survival
• GC (gemcitabine + cisplatin)
– Similar efficacy/survival rates but less toxicity
» Less neutropenia/mucositis/neutropenic fever
• Cisplatin based chemo:
– Contraindicated in patients with poor renal
function
– Alternative: carboplatin
• Hussain et al, 2001: PCG (paclitaxel,
carboplatin,gemcitabine)
– Higher response rate with median survival of 14.7 months
Summary/Conclusions
• Bladder cancer is one of the most costly cancers from dx until
death.
• Improvements in diagnosis and treatment of bladder cancer
(tumor markers, fluorescent cystoscopy, PET/CT imaging,
neoadjuvant chemo, extended lymph node dissection, use of
orthotopic neobladder)
• A lot of room for improvement in management:
–
–
–
–
Periop and adjuvant intravesical therapies remain underused (31%)
Understaging at time of cystectomy (30-50%)
High complication rates after cystectomy (25-57%)
Improvement in imaging techniques and molecular markers to
improve clinical staging
– Neoadjuvant chemo and extended LN dissection underused
References
• Jacobs, et al. Bladder Cancer in 2010: How Far Have
We Come?. CA Cancer J Clin 2010; 60: 244-272
• 2010 NCCN Guidelines for Bladder Cancer
• 2007 Update of AUA Guidelines for Bladder Cancer
• Glenn’s Urologic Surgery, 7th ed. 2010
• Campbell-Walsh Urology, ninth edition
• UCLA State-of-the-Art Urology Symposium, March
2014