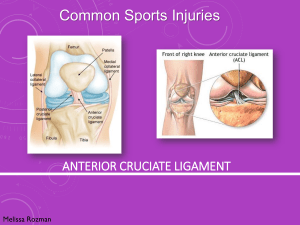
ANTERIOR CRUCIATE LIGAMENT:
A RESEARCH UPDATE ON THE CANCER
OF THE KNEE
Luke Bahnmaier MS, ATC/L, OTC
Idaho Athletic Trainer’s Association Summer Symposium
July 26, 2014
Cancer of the Knee?
“This is the cancer of
the knee!!!”
What this IS about….
Objectives
Epidemiology/Prevalence
Factors influencing ACL injury
Screening programs
Injury prevention programs
Return to play
Things to consider….
First…..
Yikes….
Epidemiology
WE ALREADY
KNOW THIS
>
Factors Influencing ACL Injury
Non-modifiable
Anatomic
Hormonal
Quasimodifiable
Neuromuscular
Modifiable
Anatomic/Developmental Factors
Q-Angle
Static pelvis and hip alignment
Body Mass Index
Knee Joint Laxity
Femoral Notch Width/Height
ACL cross-sectional area/volume/length/ultrastructure
Tibiofemoral Joint Geometry/Morphology
Medial and Lateral Posterior Tibial Slope (MTS and PTS)
MTS:PTS ratio
Tibial Plateau Width (TPW), and Depth
Anatomic/Developmental Factors
Geometric Profile More important than we thought?
Anatomic/Developmental Factors
Geometric Profile More important than we thought?
Tibial geometry influences hip and knee joint
biomechanics and forces during drop-jump and
SL land-and-cut tasks
(Schultz and Schmitz, 2010, McLean et al., 2010)
Retrospective review of ACL injured patients
shows increased posterior tibial slopes, and
increased MTS: LTS ratio and shapes (Brandon
et al., 2006, Todd et al., 2010)
Tibial sub-chondral bone geometry
retrospectively predicted ACL injury (Hashemi et
al., 2010)
Similar findings when tibial articular cartilage is
mapped (Beynnon et al., 2014)
Anatomic Factors
Anatomic Factors
What We Still Don’t Know….
Large-scale, prospective studies to
incorporate all LE alignment and
geometric measures to determine
most susceptible profiles
Is there a practical tool
that can be used to
elucidate these
measures on the field or
in the training room?
Interaction of joint laxity,
tibial geometry, and ACL
size on knee joint
biomechanics and ACL
load
HORMONES
Research suggests
females suffer most ACL
injuries during the preovulatory (follicular)
phase, compared to
post-ovulatory (luteal)
phase
HORMONES
Risk of ACL may be
higher in female athletes
with elevated serum
relaxin concentration
Sex hormone receptors
present on the human
ACL potential direct
influence on structure
Cyclic variations in knee
laxity may result in
altered knee
biomechanics
throughout the
menstrual cycle
HORMONES
What we still don’t know……
Question is….what
DO we know?!?!?!
Neuromuscular/Biomechanical
Extensively researched
Neuromuscular measures + Biomechanical measures =
Neuromechanics
Neuromuscular/Biomechanical
What we THINK we know…
Move differently
than….
Neuromuscular/Biomechanical
Neuromuscular/Biomechanical
ACL is loaded by combined sagittal and non-sagittal plane
loads, compressive and shear forces
• Knee valgus, internal rotation, and anterior shear forces
• “Dynamic Valgus” phenomenon…
Females vs. Males
Females land “stiff”, with less knee and hip flexion
• Increased VGR forces…rely on passive restraints to absorb energy
More “quad dominant” landing patterns
• Thought to increase anterior shear forces during “stiff” landing
Land with increased knee valgus angles
Neuromuscular/Biomechanical
Practicality….
http://diabeteshealth.com/cartoons/type-1/13.html
Screening Programs
What’s out there?
• Laboratory 3D Motion Capture Programs
• Expensive laboratory equipment
• Very accurate….Very expensive
• Not practical for on-field utility
• 2D Video Analysis
• Less expensive….
• Still time intensive
• Still not very practical (You already have ImPACT baselines…now
you’re telling me we need to do a 2D video jumping analysis?!?!?!)
• Landing Error Scoring System (LESS)
• Recently developed, easy to implement, based off the BESS test
• Still requires video analysis, however
Screening Programs
3D Motion Capture Systems
DARI System, University of Missouri
Brett Hayes
“It allows us to see the small changes in joint angles, joint
torques and even muscular instabilities that are difficult — if
not impossible — to measure with the naked eye,” said Brett
Hayes, a physical therapist and physical rehabilitation
manager for the Missouri Orthopaedic Institute. “We’re able to
determine where that specific athlete may have a muscular
imbalance, a joint imbalance or basically just a weakness that
we can see is a detriment to performance or, in worst cases,
we can see as potentially leading to injury if we don’t address
it.”
Screening Programs
Landing Error Scoring System (LESS)
• Valid and reliable (Padua et al., 2009)
• Intra- and inter-rater reliability good to excellent (Padua et
al., 2009, Onate et al., 2010)
• LESS scores higher in subjects s/p ACL-R (Bell et al., 2014)
Screening Programs
Landing Error Scoring System (LESS)…BUT…
Smith et al., 2012
Injury Prevention Programs
Injury Prevention Programs
Multiple studies have shown training programs correlate
with changes in biomechanical profiles thought to be “highrisk”
….So why wouldn’t these programs work to prevent, or
reduce, ACL injury?
Short answer:…some have
shown promising results, though study
design has been questionable
Long answer:…Talk to Dr. Shea
and get his opinion
Injury Prevention Programs
Hewett and colleagues, AJSM, 1999
Sportsmetrics program
6 week pre-season program
1,263 basketball, soccer, and volleyball athletes for 1 season
Injury Prevention Programs
Mandelbaum and colleagues, AJSM, 2005
Prevent injury, Enhance Performance (PEP) Program
Injury Prevention Programs
Gilchrist et al., AJSM 2008
Prevent injury, Enhance Performance (PEP) Program
Prospective, RCT of D-1 collegiate female soccer athletes
Intervention athletes 3.3 times less likely to suffer NC-ACL
Only statistical significance was ACL injuries in practice…
Promising trend in a Level I study…how do we interpret?
Injury Prevention Programs
Pfeiffer and colleagues, JBJS 2006
Boise, Idaho Special!
Prospective, non-randomized, two year study
Program similar to Sportsmetrics, but less time-intensive
Injury Prevention Programs
Injury Prevention Programs
Things to Consider…
Retention of movement patterns affected by program duration (Padua
et al., AJSM 2012)
Current, commercially available training programs may not affect LE
biomechanics for youth athletes under the age of 12 (DiStefano et al.,
AJSM 2011)
Numbers needed to treat to prevent 1 non-contact ACL injury over one
season is estimated at 108 individuals (Sugimoto et al., Br J Sports
Med. 2012)
Peripheral and central fatigue, with unanticipated landings, are shown
to significantly affect LE biomechanics during landing and cutting….so
WHY aren’t we incorporating these into our programs? (McLean and
Samorezov 2009, Borotikar 2007, McLean 2007)
Return to Sport
Ryan Mizner PT, PhD
University of Montana
Growing body of evidence showing significant asymmetries
in landing biomechanics at time of RTS following ACL-R
(Paterno et al., 2011, Di Stasi et al., 2013, Delahunt et al., 2012,
Webster et al., 2014)
Asymmetries retrospectively predicted re-rupture or contralateral ACL tear upon RTS (Paterno et al., 2010)
Asymmetries present even in those who have passed RTS
testing (Di Stasi et al., 2013)
Do we need to include 3-D motion analysis in our
RTS criteria?
Return to Sport: Re-injury
Incidence rate of ACL injury following ACL-R 15 times
greater than that of controls (Paterno et al., 2012)
• Females 4X more likely to suffer ACL graft rupture, 6X more likely
to suffer contralateral ACL injury
29.5% of 78 patients who underwent ACL-R (Paterno et
al., 2014)
• Risk of second ACL injury 6 times greater in ACL-R group
• Twice as likely to suffer contralateral ACL injury
For patients under 20 s/p ACL-R, odds of suffering
ipsilateral and contralateral ACL injury increased 6-,
and 3-fold, respectively (Webster et al., 2014)
Clinical Take Home Points
Critically evaluate research, don’t swallow the
“Blue Kool-Aid”
Consider modifying current prevention programs
to include fatigue, with unanticipated movements
Consider assessing jump-landing movement
patterns with return to play, access to 3-D motion
analysis?
Understand that geometric profiles of the tibia may
be more important in ACL injury risk than we have
historically thought
THANK YOU