DK, MBSS
advertisement
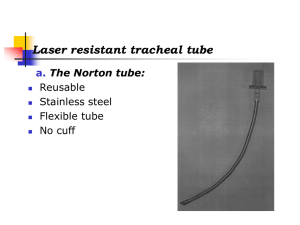
Management of Communication and Swallowing for Adults with Tracheostomy Tubes Sally L. Gorski, M.A. CCC Purpose of Artificial Airways Provide adequate ventilation and oxygenation Maintain a patent airway Eliminate airway obstruction Reduce potential for aspiration Provide access to the airway for pulmonary toilet Endotracheal Intubation Creating an alteration in the airway: Translaryngeal -orally -nasally Transtracheal Endotracheal Intubation Creates an artificial airway Insertion of a tube into the mouth or nose Passes through the pharynx and vocal cords Need for airway protection Need for mechanical ventilation Temporary Intubation Issues Depends on the route of intubation Size of the tube Trauma during intubation or selfextubation Length of intubation Complications of Oral Intubation Trauma to teeth and gums Abrasion of the lips, tongue, pharynx and larynx Damage to the vocal folds Overinflated cuff Hypoxemia Rare – damage to the recurrent laryngeal nerve Complications of Nasal Intubation Trauma to nasal passages Necrosis may result Removal of the tube may cause epistaxis Otitis media and conductive hearing loss due to mechanical blockage of the Eustachian tube Long Term Complications Stenosis Pressure necrosis Granuloma – may develop into a polyp Persistent hoarseness Laryngeal web Compromised laryngeal closure and airway protection Cricothyroidotomy Procedure usually performed in an emergency situation Surgical creation of an opening into the cricothyroid membrane May be necessary due to upper airway obstruction Tracheostomy Tracheotomy The surgical creation of an opening into the trachea through the neck. The surgical placement of a plastic or metal tube into the trachea to create an airway. Indications for Tracheostomy Facilitate weaning from the ventilator Bypass an obstruction of the upper airway Facilitate removal of secretions Facilitate long-term airway management Prevent gross aspiration from the pharynx or GI tract Decreased risk of accidental removal Procedure – tube choice Depends on the patient’s ventilation needs, age, size Medical status Physician preference Institution preference/practice Procedure - tracheostomy Placement of the tube above or below the 2nd and 3rd tracheal ring Incision type and placement Vertical skin incision is most common Horizontal skin incision, rarely used today Risks with Trach placement Stenosis at the stoma site: 1-8% Massive hemorrhage: 1% Aspiration of oral secretions Pneumothorax Incorrect placement of the tube can lead to cardiorespiratory arrest Long Term Complications Tracheal granuloma Tracheomalacia Tracheal stenosis – assoc with longer term tracheotomy Tracheoesophageal fistula Percutaneous Trach Minimally invasive, “simple” technique Eliminates a trip to the OR Reduced blood loss Reduced infection rates (0 to 3.3%) (As high as 36% in open trach procedure.) Stenosis rates range from 0 – 9% Performed in the ICU Complications of Perc Trach Risk of bleeding False passage of the tube Infection and tracheal wall injury Long Term – Tracheal granuloma Stenosis Tracheomalacia Clinical Conditions – Trach Obstructive disease; COPD, asthma Restrictive disease; ARDS, pneumonia, scleroderma Chest wall disorders; kyphoscoliosis, chest trauma Neuromuscular; ALS, Guillain-Barre’, muscular dystrophy, post polio syndrome, multiple sclerosis, SCI Clinical Conditions - Trach Upper airway; trauma, tumors, infection Respiratory center dysfunction; sedation, narcotics, anesthesia, CVA, drug overdose Cardiac/circulation; cardiopulmonary arrest, pulmonary edema, congestive heart failure Types of Tubes Design: Cuffed, uncuffed, TTS cuff, fenestrated Composition: Silicone plastic, metal, polyvinyl chloride (PVC), etc. Manufacturers: Shiley, Portex-Bivona, Pilling-Weck Components of a Trach Tube Neck flange Inner & Outer cannula Obturator Cuff Pilot balloon, cuff inflation line Plug, cap or button Standard length; extra long The Referral to Speech Path When to intervene? -Upon consult from the physician -While pt is intubated, if awake and alert -After trach is placed, if awake and alert -As soon as the patient is communicative; yes/no head nods, mouthing, writing, gestures, etc. The Initial Consult Review the chart Discuss pt’s status with the RN, physician and the respiratory care practitioner Can pt tolerate cuff deflation? Level of ventilatory support Secretion status Passy-Muir Speaking Valve If the patient can tolerate cuff deflation, on or off the ventilator, proceed with the initial trial of the PMV. Open Tracheostomy Tube Inflated Cuff Breathing in and out through the tube only No airflow through the upper airway Lack of vocal production Open Tracheostomy Tube Inflated Cuff Decreased sense of smell/taste Risk of tissue necrosis Cuff impingement on esophagus may cause reflux Lack of Airway Pressure Decreases effectiveness Patient is unable to mobilize secretions effectively Patient requires more frequent suctioning Lack of Airway Pressure Decreased physiologic PEEP Decreased gas exchange due to reduced surface area of alveoli Decreased oxygenation Possible atelectasis Open Position Valves All other valves are open position valves Patient must exhale to close the diaphragm of the valve Secretions travel up the tube and may occlude the valve For communication only Passy-Muir Valve Design Closed position, “no leak” design Open only during inspiration with minimal effort Closes automatically before the end of the inspiratory cycle/beginning of the expiratory cycle Passy-Muir Valve Design No air leakage occurs through the PMV during exhalation A column of air is trapped in the PMV and in the trach tube that inhibits secretions from entering the tube Restores more normal “closed respiratory system” Animations courtesy of Passy-Muir Inc. Irvine, CA. Physiologic Benefits of the PMV Improved voice production Improved sense of smell/taste Restoration of normal physiology may prevent aspiration Deflated cuff allows for increased laryngeal elevation Physiologic Benefits of the PMV Restoration of subglottic pressure facilitates a better swallow and decreases the risk or aspiration Swallow is not only mechanical, but a pneumatic system as well The patient has a more efficient and effective cough Physiologic Benefits of the PMV Improved secretion management Improved cough Decreased suctioning needs Decreased risk of tracheal damage Patient Selection Where is the patient? What type of trach tube? What type of vent? Who are your allies? Where do you begin? Team Members Varies depending on the setting Speech-Language Pathologist Respiratory Care Practitioner Nurse Physician Indications for Use of the PMV - review Traumatic Brain Injury Spinal Cord Injury Chronic Obstructive Pulmonary Disease Chest or laryngeal trauma Acute Respiratory Distress Syndrome Neuromuscular diseases; ALS, MS, Guillain-Barre’ Contraindications for Use of the PMV Unconscious and/or comatose patients Inflated cuff on the trach tube Foam-filled cuffed trach tube Severe airway obstruction Severe risk for aspiration Severely reduced lung elasticity Patient Assessment Medically stable Adequate level of alertness Ability to handle secretions Swallowing status/risk for aspiration Viscosity and abundance of secretions Patient Assessment Monitor baseline parameters Oxygen saturation Heart rate Respiratory rate Blood pressure Breath sounds Normal Values Oxygen Saturation: 90-100% Respiratory Rate: <28 bpm Heart Rate: <120 bpm Acid-Base Balance (pH): 7.35-7.45 Albumin: 3.5-5.5 Ventilator Adjustments Alarms -Volume -Pressure Compensate for loss of airflow through vocal cords if necessary Placement of the PMV Inline Assess whether the pt can exhale around the trach tube and through the upper airway Trach tube should be sized for sufficient airflow around trach tube Trach tube cuff may create bulk even in the deflated condition Assess for Upper Airway Patency With the vent dependent patient, deflate the cuff, let patient adjust his respirations, encourage the patient to open mouth slightly and say “ahhh” when exhaling and encourage a cough or throat clear. Placement Guidelines Suction patient tracheally and orally Deflate cuff slowly, allowing patient time to adjust Suction again as necessary Encourage pt to clear throat and expectorate secretions from the oral cavity Place PMV inline with the vent circuit In-Line Suction Catheter The Initial Trial – How Long? Continue to monitor the vital signs; SaO2 level, RR, HR, etc. Is the patient talking? Are they breathing comfortably? Continue as tolerated Troubleshooting Issues Changes in breathing – pt may require short trials and/or gradual transition Increased coughing – due to airflow through upper airways. Remove valve and reassess Troubleshooting Issues Anxiety and fear – educate patient, reassure patient that feelings or fears are valid Depression or lack of motivation – enlist family involvement; allow pt to communicate, perhaps with a chaplain or psychologist If Patient is Unable to Exhale: Remove PMV immediately Check trach cuff for complete deflation Make sure patient and trach tube are positioned appropriately Repeat suctioning tracheally and orally Nasal suctioning may be indicated If Patient is Unable to Exhale Assess trach tube size for possible downsizing Consider edema as a factor, try again in 24 hours Potential for change to a cuffless trach Potential for change to a Bivona trach with a tight-to-shaft cuff Educate Staff When using the Passy-Muir Valve the cuff must be completely deflated Use the warning label provided with the patient care kit Trach/Vent Patients Tracheostomy Cuffs Bonnano, P.C. (1971) Difficulty in swallowing results by direct inhibition of the hyomandibular complex. This occurs as a result of the tracheostomy tube anchoring the trachea to the strap muscles and skin of the neck. Cuff Presence and Aspiration Does not prevent aspiration Even when the cuff is deflated, can still be bulky in the trachea Clinical Dysphagia Exam Completed in conjunction with nurse or RT Complete an oral mechanism exam Preferable to perform the exam with the cuff deflated to maximize laryngeal function Clinical Dysphagia Exam Preferable to conduct the exam with the PMV in place Prepare consistencies with blue if available Present in small amounts, suction after each consistency type Blue Food Coloring At HCMC: Dispensed by the Pharmacy in 1 ml syringes Single use amounts Used for bedside exams with trach pts and for FEES exams Approved by MDs and PharmDs Modified Barium Swallow Study Considerations: Patient has to transport to Radiology Will need RN and RT present if on the vent Additional preparation completed by the Speech Pathologist If pt is tolerating the PMV, place the PMV during the MBSS Fiberoptic Endoscopic Evaluation of Swallowing Exam can be conducted at the bedside eliminating the need for transport Additional coordination provided by the Speech Pathologist Treatment Strategies Traditional treatment approaches May only tolerate frequent, smaller meals May receive primary nutrition/hydration via an alternative source and have limited oral intake “for pleasure” or “for comfort” Treatment Strategies Post instructions regarding PMV use during oral intake May need to add blue to food or liquid items at each meal for several meals Dysphagia Treatment Case Study J. A., 28 y.o. admitted 3/29 with nausea and vomiting x4 days Intubated for two surgical procedures PMHx: pituitary macroadenoma, s/p resection in 2003 Extubated 4/5 and referred to Speech Pathology Dysphagia Treatment MBSS completed 4/11, absent swallow response FEES completed 4/24, profound pharyngeal dysphagia Trach placed, PEG placed following the MBSS Dysphagia Treatment Repeated the MBSS 5/31, continued severe dysphagia, continue NPO Pt’s trach is a Jackson, tolerates plugging Dysphagia tx during the month of July Base of tongue exercises Pharyngeal strengthening exercises Dysphagia Treatment Repeat MBSS, 7/26 Mild dysphagia, start oral intake Per ENT, subglottic granulation tissue, so trach was not immediately removed Laser excision of granulation tissue in early Sept, then decannulated PEG removed Persistent mild dysphonia secondary to right TVC paralysis Case Study J.B., 42 y.o. admitted 8/16 w/ selfinflicted GSW right below chin Perc trach placed on DOA Clinical dysphagia exams 8/19 and 8/20 – no evidence of blue in secretions Holding on PMV – pt writing/gesturing to communicate 8/23 - MBSS J.B., cont. Nectar thick and water thin liquid selfpresented via syringe Encouraged him to administer 2-4 ml per swallow Good oral control Timely pharyngeal response No aspiration OK for a Fractured Jaw Diet w/ syringe J.B., MBSS – Aug 23 Case Study D.K., 51 y.o. male, C5-C6 dislocation w/ resulting quadriplegia after a fall, onset date 5/18 ACDF 5/20 Trach/PEG 5/27 Discharged to acute rehab Outpatient MBSS 8/22. Bivona TTS trach - capped D.K., MBSS – Aug 22 D.K., cont. Results: moderate dysphagia Pharyngeal residue Penetration with nectar and water Trace aspiration with water, delayed cough Advance to Soft Diet, cont nectar thick liquids D.K., MBSS – Sep 22 D.K., cont. Repeat MBSS 9/21/11 Persistent dysphagia – silent aspiration of trace amts of water thin liquid Advance to Mechanical Soft Diet, cont nectar thick liquids Continue effortful swallow Strategy: Swallow, cough hard, swallow again with all liquids A.B., MBSS – Mar 23 QUESTIONS?