Donald McLaren, MD
Seventh International Symposium in
Continuing Nursing Education/March 2014
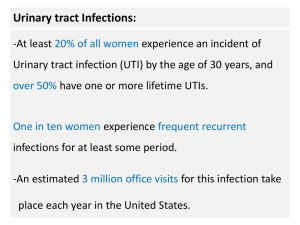
Discuss
latest AAP guidelines for diagnosis
and treatment of UTIs in febrile infants
Discuss UTI symptoms, diagnosis and
treatment in children of all ages except
newborns
To discuss some causes recurrent UTI and
prevention of UTI and kidney damage in
children with recurrent UTI
In
febrile infants and small children, the
urinary tract is the most common site of
bacterial infection – about 5% of children 224 months will get at least one UTI
Some recommend UC in all 2-24 mo girls and
uncircumcised males with fever >39o with no
source and < 6 moa for a circumcised male
(their risk much lower) (2-4 % vs. 10-25%)
The
AAP periodically has put out guidelines
for diagnosis and management of UTI in
children.
The 2011 guidelines updating the 1999
guidelines: “Urinary Tract Infection: Clinical
Practice Guideline for the Diagnosis and
Management of the Initial UTI in Febrile
Infants and Children 2-24 months” found at:
http://pediatrics.aappublications.org/conten
t/early/2011/08/24/peds.2011-1330
This
has significant recommendation changes
concerning diagnosis and evaluation of
febrile UTIs in this age group.
We will discuss these guidelines. While there
has been some controversy, the guidelines
are very useful for us on the field as we work
with children with possible UTI. They will
decrease the amount of travel required for
work-up after the initial febrile UTI in this
age group over the 1999 guidelines
I
presented this topic in 2009. At that time
the recommendation was that children with
a first time febrile UTI needed an evaluation
including a Renal Bladder US (RBUS) and
VCUG (Voiding cystourethrogram)
This was because 33% had an underlying
condition or vesicoureteral reflux (VUR) to
explain the UTI AND
It was felt that repeated febrile UTIs in
someone with VUR would result in significant
sequelae – renal scarring, HTN, and eventual
RF and as evidence see the next 2 slides
When
1999 guidelines written, belief was
that renal scarring occurred with UTI ONLY if
VUR allowed infected urine reflux back up to
the kidneys
But some then were already questioning
whether this was true? Was this aggressive
approach really indicated? I ended with this:
Medicine is fun, exhilarating, maddening,
frustrating, challenging, ever changing
We in the profession must keep up as best we can
to offer our patients the best care.
What is dogma now may become wrong tomorrow
We often don’t know what we don’t know.
So,
as I present the 2011 guidelines, realize
there is some controversy – some still think a
first time UTI in a febrile child needs to be
evaluated with a RUS and VCUG
But these new guidelines give us some much
needed guidance for patients living overseas
in deciding who needs to travel for further
evaluation. They providing excellent
guidance for diagnosis, treatment and workup of UTI in this group of children.
“This
clinical practice guideline is not
intended to be the sole source of guidance
for the treatment of febrile infants with
UTIs. Rather, it is intended to assist
clinicians in decision making. It is not
intended to replace clinical judgment or to
establish an exclusive protocol for the care
of all children with this condition.”
Action
Statement 1: If a clinician decides
that a febrile infant with no apparent
source for the fever requires antimicrobial
therapy because of ill appearance or
another pressing reason, the clinician
should ensure that a urine specimen is
obtained for UA AND UC by catheterization
or SPA (suprapubic urine) before
antimicrobials given.
Pediatric EM Morsels © 2010-2014
http://pedemmorsels.com/hyperpyrexia-2/hyperpyrexia-2/
To
tx first would obscure diagnosis of UTI
SPA gold standard but many consider it
invasive and is more painful. May be only
option in some (phimosis, labial adhesions)
Catheterization urine culture 95% sensitive,
99% specific compared to SPA
A bagged urine specimen not adequate in this
age - has very high false positive rate (88%
false + rate) and is only useful if negative
If
a clinician assesses a febrile infant with
no apparent source for fever as not being
so ill as to require immediate antimicrobial
therapy, then the clinician should assess
the likelihood of UTI
2a If clinician determines the febrile infant
to have a low likelihood of UTI, then
clinical follow-up monitoring without
testing is sufficient
2b
If clinician determines that the febrile
infant not in a low-risk group then either:
Option 1 is to obtain a urine specimen through
cath or SPA for UA and UC. OR
Option 2: Obtain urine specimen by most
convenient means and perform UA. If the UA
results suggest UTI (+ leukocyte esterase or
nitrite test; + microscopic analysis for
leukocytes or bacteria), obtain the urine by
cath or SPA for UA and UC (fresh < 1 hour old
specimen or if refrigerated < 4 hours old)
UTI
prevalence among febrile girls > 2X that
of infant boys.
Rate for uncircumcised boys 4-20X that of
circumcised boys who only have 0.2-0.4% risk
Presence of another source (i.e. OM) lowers
risk by half.
New guidelines has a system based on studies
to determine if risk is < 1% or at least 2%
Risk grid not absolute – if patient unlikely to
keep F/U or lives in a remote location it is
wise to check for UTI even if risk very low
Individual Factors
•
•
•
•
•
Race: White
Age: <12 months
Temperature: ≥39⁰C
Fever: ≥2 days
Absence of another
source of infection
Probability of
UTI
# of Factors
Present
≤1%
No more
than 1
≤2%
No more
than 2
Individual Factors
•
•
•
•
Race: Nonblack
Temperature: ≥39⁰C
Fever: >24 hours
Absence of another
source of infection
Probability
of UTI
# of Factors
Present
Circumcised
No
Yes
≤1%
*
No more
than 2
≤2%
None
No more
than 3
*Probability of UTI exceeds 1% even with no risk factors other than being
uncircumcised.
To
establish the diagnosis of UTI, clinicians
should require both UA results suggesting
infection (pyuria and/or bacteriuria) and
the presence of at least 50 000 colonyforming units (CFUs) per mL of a
uropathogen cultured from a urine
specimen obtained through catheterization
or SPA
+
UA AND UC now considered essential to
diagnosis – UA essential, not sufficient alone
If only a + UC with - UA, considered to be
either asymptomatic bacteriuria or
contamination as inflammation should lead
to an abnormal UA also
Asymptomatic bacteriuria known to occur in
older children. 0.7% of afebrile girls had 3
cultures with a single uropathogen
Lack of pyuria distinguishes true UTI from
asymptomatic bacteriuria
Dipstick
Positive leukocyte esterase is a marker for pyuria
Sensitivity 94% in context of clinically suspected UTI
Reported as 83% in other studies
Specificity much less – 64-92% - false positives
Positive Nitrite (converted from dietary nitrates
in presence of most gram negative bacteria but
requires 4 hours in bladder)
Not sensitive but very few false positives (specific) so
if positive almost certainly have bacteria in the urine
>
5 WBC / hpf (25 WBC / microliter)
> 10 WBC/microliter in counting chamber
Unspun gram stained urine – 1 gm – bacteria
/ 10 hpf = 105 bacteria
UC of fresh or refrigerated specimen
Significant > 50,000 CFUs/ml of a single urinary
pathogen
Lower number for SPA (> 1000 CFU/ml)
Always do sensitivity if grows urinary pathogen
http://www.impactednurse.com/?p=2144
http://library.aua.edu.ag/webpath/webpath/tutorial/urine/urine.htm
Action
Statement 4a When initiating
treatment, the clinician should base the
choice of route of administration on practical
considerations. Oral and parenteral are
equally efficacious. The choice of agent
should be based on local antimicrobial
sensitivity patterns (if available) and should
adjust the choice according to sensitivity
testing of the uropathogen
4b
One can choose 7 to 14 days as the
duration of antimicrobial therapy
Goals
of treatment
Eliminate infection and relieve symptoms
Prevent complications
Reduce likelihood of renal damage
“Most experimental and clinical data support the
concept that delays in the institution of appropriate
treatment of pyelonephritis increase the risk of
renal damage.”
Most
can be treated orally
Treat parenterally if toxic appearing
Or if cannot hold down meds due to N/V
Possibly if not responding or cannot get F/U
Duration
of treatment 7-14 days
Data comparing 7,10,14 days not available
Evidence 1-3 days of treatment inferior
Based
on local resistance patterns if possible
Must cover E. coli (80% of UTIs in this age)
and other gram negative organisms
Significant degree of resistance in many
places to TMP-SMP and Cephalexin
Those with multiple previous episodes of UTI
often seem to be resistant to more drugs
© 2013 Answers in Genesis www.AnswersInGenesis.org.
Amoxicillin/clavulanate
20-40 mg/kg/day
q8hr
Sulfisoxazole or TMP-SMX: 6-12 mg/kg TMP
and 30-60 mg/kg SMX daily in 2 doses
Cephalosporins
Cefixime – 8 mg/kg/ day in 1 dose
Cefpodoxime – 10 mg/kg/day in 2 doses
Cefprozil – 30 mg/kg/day in 2 doses
Cefuroxime axetil – 20-30 mg/kg/day in 2 doses
Cephalexin – 50-100 mg/kg/day in 4 doses
Ceftriaxone
75 mg/kg every 24 hours
Cefotaxime 150 mg/kg/day divided q 6-8 hr
Ceftazidime 100-150 mg/kg/day divided q 8
hr
Gentamycin 7.5 mg/kg/day divided q 8 hours
Tobramycin 5 mg/kg/day divided q 8 hours
Pipercillin 300 mg/kg/day, divided q 6-8
hours
Febrile
infants with UTIs should undergo
renal and bladder ultrasonography (RBUS)
While
not super useful, helpful in some cases
Non-invasive and no radiation
To detect anatomic abnormalities that
require further evaluation and abscesses
Evaluate renal parenchyma
Assess renal size as baseline so as to monitor
Less useful now as many already had RBUS as
prenatal screening (but often uncertain
timing and quality of US during pregnancy)
Timing
of RBUS within 2 days if severe or not
improving
Otherwise, later better as 2 days into a UTI
would not be a true baseline as E-coli
endotoxin can cause edema
DMSA scan shows if patient has pyelonephritis
much better but rarely changes initial
treatment. Not recommended at early stage
© 2014 RemakeHealth Inc.™ All Rights Reserved. http://www.remakehealth.com
© 1994-2014 by WEBMD LLC. http://www.emedicine.medscape.com
Action
Statement 6a: VCUG should not be
performed routinely after the first febrile
UTI; VCUG is indicated if there is
hydronephrosis, scarring or other findings
that would suggest high grade VUR or
obstructive uropathy on RBUS as well as in
other atypical or complex clinical
circumstances
Action Statement 6b: Further evaluation
should be conducted if there is a
recurrence of febrile UTI (evidence
quality: X; recommendation).
Strategy
for 40 years
Prevent further damage after initial UTI by
determining which had treatable GU
abnormalities which would increase risk of renal
damage with recurrent UTI
Antimicrobial prophylaxis with Bactrim or
Nitrofurantoin to prevent further UTI if VUR
Or if high grade VUR or failed trial of
prophylactic antibiotics, VUR surgery
However several studies have shown that one can
get renal scarring/damage without VUR
Some studies indicate that antibiotic prophylaxis
is not effective except in grade V reflux
If prophylaxis is not usually helpful AND one can
get pyelonephritis, renal damage without VUR,
then rationale for VCUG is questionable for VUR
grades I-IV.
Grade V is not common among those with UTI
(1/100) so by waiting reduce need for invasive
VCUG testing after first febrile by UTI 90%
Study now underway to determine effects of
prophylaxis in children 2 months – 6 years “The
Randomized Intervention for Children with VUR
study” (TMP-SMX in 607 children with grade I-V
VUR following UTI)
100%
80%
Prophylaxis
60%
No Prophylaxis
NS
40%
20%
NS
NS
NS
NS
0%
None
Grade I
Grade II
Grade III
Grade IV
N=373
N=100
N=257
N=285
N=104
Pediatric Care OnlineTM ©American Academy of Pediatrics
250
Prophylaxis
No Prophylaxis
200
150
100
50
0
None
Grade I
Grade II
Grade III
Grade IV
Pediatric Care OnlineTM ©American Academy of Pediatrics
After First UTI
(N=100)
After Recurrence
(N=10)
No VUR
65 (65%)
2.6 (26%)
Grade I–III VUR
29 (29%)
5.6 (56%)
Grade IV VUR
5 (5%)
1.2 (12%)
Grade V VUR
1 (1%)
0.6 (6%)
Pediatric Care OnlineTM ©American Academy of Pediatrics
Impact of a More Restrictive Approach to Urinary
Tract Imaging After Febrile Urinary Tract Infection
N=103
“By restricting urinary tract imaging after an initial
febrile UTI [based on NICE guidelines, 2007], rates of
voiding cystourethrography and prophylactic antibiotic
use decreased substantially without increasing the risk
of UTI recurrence within 6 months and without an
apparent decrease in detection of high-grade VUR.”
Schroeder AR, Abidari JM, Kirpekar R, et al. Impact of a more restrictive approach to urinary tract
imaging after febrile urinary tract infection. Arch Pediatr Adolesc Med. 2011;165(11):1027–1032
Action
statement 7: After confirmation of
first UTI, parents should be instructed to
seek prompt (ideally within 48 hours) for
future febrile illnesses to ensure that
recurrent infections are detected and
treated promptly.
Why? (Early treatment limits renal damage better
than late treatment and risk of renal scarring
increases with number of recurrences)
1.
2.
3.
4.
5.
6.
7.
8.
Relationship between UTIs and reduced
renal function / hypertension
Alternatives to invasive collection of urine
and culture
Role of VUR (and, thus, VCUG)
Role of prophylaxis (RIVUR study)
Genetics
Hispanics
Further treatment: What and for whom?
Duration of treatment
TM
AAP Guideline for the
Diagnosis and Management
of UTIs in Febrile Infants
Unanswered Questions and Unquestioned
Answers
Kenneth B. Roberts, MD, FAAP
Professor of Pediatrics (Emeritus)
University of North Carolina
Roberts KB. “AAP Guideline for the Diagnosis and Management of UTIs in Febrile
infants.” Pediatric Care Online Accessed 1/17/2014 at
www2.aap.org/pcorss/webinars/pco/AAP%20Webinar_UTI-Roberts-Final.ppt
80%
E. coli but also Klebsiella, Proteus,
Enterobacter, Citrobacter, etc. Gram + rare.
Non-E.coli more common with anomalies of
UT, younger age, previous tx with antibiotic
Few bacteremic except newborns.
Beyond newborn period due to bacteria
ascending up urethra to bladder
Newborn hematogenous or ascending
Most UTIs due to UPEC (uropathogenic E.
Coli); most E. Coli pyelo have P. pili fimbriae.
Younger
age, Being female, white race
Lack of circumcision
Genetic factors
Urinary tract obstruction or VUR
Bowel/bladder dysfunction
Sexual activity
Bladder catheterization
Risk of renal scarring: recurrent UTI, delay in
treatment of acute UTI, bladder/bowel
dysfunction, obstruction, VUR, ? young age
Very
non-specific in younger children
First 2 months high fever, jaundice, apnea,
many more – often with sepsis
After 1-2 months: fever (especially > 39o and
if >48 hours) and suprapubic tenderness
Some irritability or fussiness and other nonspecific signs: poor feeding, FTT
Foul smelling urine and GI symptoms not
found to be helpful in diagnosis
Classic
sx: fever and urinary symptoms
(frequency, dysuria, urgency, incontinence,
hematuria, abd. pain)
For pyelonephritis in older children fever,
chills, flank pain and abdominal pain
Not all with sx have UTI: ddx of urethritis
include vulvovaginitis, irritant or chemical,
urethritis, urinary calculi, STD, vaginal FB
In past it was said and I always presume if
UTI + fever = pyelonephritis. Not always true
but cannot do a DMSA scan in all of them
http://nutravize.com
History
-Determine if chronic symptoms,
constipation, previous UTIs or undiagnosed
febrile illnesses, VUR, FH, antenatally
diagnosed renal abnormality, high Bp, poor
growth, sexual activity and spermicides
Physical: Bp, Temp, growth parameters,
tenderness of abdomen, external genitalia,
low back exam, other sources of fever
Lab
– Need + UA AND UC to confirm UTI
Usually no need for BC after 2 months
No need for creatinine unless recurrent
If potty trained can do CCUA specimen
> 100,000 CFU/ml for CCUA
> 1000 CFU/ml for SP
>50,000 CFU/ml for cath culture
If 10-50,000 repeat
If same result of same and only one uropathogen treat
50%
E. Coli resistant to Amoxicillin, Amp;
increasing resistance to TMP-SMX,cephalexin,
Amoxacillin-clavulanate, Amp-sulbactam
If suspect enterococcus don’t use
monotherapy – add Ampicillin (urinary
catheter, anatomical abnormality)
3rd gen. cephalosporins best starting drug.
Oral as good as IV for time to symptom
resolution, sterilization of urine, reinfection
rate, renal scarring at 6 months
FLQs
effective but increasing resistance. ?
safety in children - limit to Pseudomonas and
multidrug resistant gram negative organisms
Should improve within 24-48 hours.
No need to reculture unless not improving 24
hr
Studies conflict on whether prophylaxis
useful for recurrent UTI – some say only if
grade V reflux – others if III-V reflux
Would try after 2nd UTI + VUR as trial
Study ongoing to see if steroids prevent renal
damage with UTI
RBUS:
Children < 2 with 1st UTI, any age with
recurrent febrile UTIs, children with FH of
kidney issues, HTN, poor antibiotic response.
VCUG if < 2 yo with 2 or more febrile UTIs,
FH of renal/urological disease, poor growth
or HTN, perhaps those with organism other
than E.Coli and prophylaxis if grade > III VUR
DMSA not routine – shows pyelonephritis,
most VUR III or higher, as well as scarring.
F/u with growth, weight and Bp – not UA, UC
Refer
if dilating VUR (III-V) or obstructive
uropathy, renal abnormalities, impaired
kidney function, elevated Bp, bowel or
bladder dysfunction that is refractory to
primary care measures
Most
have no long term sequelae
< 19 with first UTI – 25% had VUR, 2.5% had
grade IV or V reflux.
VUR increases risk of acute pyelonephritis
and renal scarring and 15% showed evidence
of renal scarring at F/U
8% had at least one recurrence
8-30%
have > one symptomatic reinfections.
Evaluate for, tx bowel/bladder dysfunction
No need for F/U cultures
Inform parents after febrile UTI they need to
seek care soon if symptoms or fever develop
Consider prophylaxis for those without VUR if
3 febrile UTIs in 6 months or 4 in year.
With VUR grade 3-5 after second febrile UTI.
TMP-SMX 2 mg TMP/kg or Nitrofurantoin 1-2
mg/kg
6 months and if no UTIs can stop and resume if
another recurrence
90% E. coli (then other gm - organisms)
>100,000 CFU/ml uropathogen
Ddx- bladder dysfunction, vaginal FB, drug,
chemical, nonspecific vulvovaginitis, cervicitis,
urethritis, prostatitis, epididymo-orchitis,
nephrolithiasis, urethral stricture, interstitial
(autoimmune), neoplasm
Treat empirically
If > 13, uncomplicated include coverage for
staph saprophyticus – TMP-SMX or cephalosporin
In older children if not complicated treat 5-7
days. If younger or complicated 7-14 days
© 2005-2014 All Rights Reserved http://www.childrenshospital.org
Retrograde
passage of urine into upper
urinary tract from the bladder
1% newborns; 30-45% young children with UTI
Most common urological finding in children
Can be primary or secondary due to
abnormally high pressures in bladder
More common in whites, girls, younger.
Strong genetic component
Diagnose by VCUG or radionuclide cystogram
(RNC)
30-60%
of those with IV or V reflux have
primary renal scarring – may be
developmental issue
? if scarring result of developmental issue or
due to infections ascending up to kidney due
to VUR; many continue to believe latter
> ½ resolve on their own – more likely with
milder degrees (I-II 80% resolve in 5 years)
High grade rarely resolve on own
Evaluate all with VUR and F/U for renal
status, growth parameters, Bp, creatinine
(initially) and UA for pyuria and proteinuria
Unknown
benefits of treatment. UpToDate
management based on available data,
prevention of pyelonephritis, likelihood of
renal scarring and of spontaneous resolution
of VUR, and patient/family preference
Screen for voiding dysfunction
III-V either treat (prophylaxis) or surveillance and
prompt treatment if UTI
I,II observation vs. antibiotic prophylaxis with
family input
Trials so far display no difference in outcome
between antibiotic prophylaxis, surgical VUR
repair - get family input
Surgery recommended if unlikely to resolve
(family input); Grade V reflux + scarring, Grade
V > 6 YOA, III-V with failed medical tx
Dx and tx promptly if symptoms or febrile illness.
Yearly RBUS. DMSA if RBUS suggests renal
scarring, poor renal growth, those with recurrent
UTI and with Grade III-V VUR
F/u yearly growth, Bp and UA
Essential
to determine in children with UTI or
VUR if have bladder dysfunction - problems
with bladder filling or emptying which can
predispose to repeated infections.
Can be from neurogenic, anatomic (ectopic
ureter, obstruction) or functional causes
Hx,
Px, UA, UC – Suspect if:
Daytime urinary incontinence in school age or
previously toilet trained children
Urinary sx: urgency, dribbling, dysuria, daytime
frequency, nocturia, hesitancy, holding
maneuvers to avoid voiding, abnormal or
intermittent flow or stream, incontinence,
abdominal straining, holding maneuvers, post
void residual, if VUR or recurrent infections
Dysfunctional Voiding Symptoms Survey
questionnaire or voiding diary very helpful
R/O neurological or anatomical causes
http://fmymind.com/urine-trouble/
Many
types beyond scope of talk. Will
discuss only daytime wetting due to
dysfunctional voiding - occurs in 20% of 4-6
years old- causes
Overactive bladder (urgency)
Voiding postponement and underactive bladder
(Valsalva to urinate large volume post void
residual)
Dysfunctional voiding (Inability to relax
urethral sphincter and/or pelvic floor
musculature during voiding. Detrusor
contractions during voiding against a closed
external urinary sphincter. Get interrupted
staccato flow pattern, prolonged voiding time)
Other
http://www.vcu.edu/urology/patients/conditions/peds_urology/dys_voiding.html
Can
reduce symptoms in as many as 40-70%
Take care of constipation
Explain to parents, patient if appropriate
Voiding behavior modification if age
appropriate
Educate family including how child’s voiding
patterns deviate from normal
Timed voiding schedule and 72 hr voiding diary
Frequent voiding q 2-3 hours all day
Try to empty bladder fully and use double voids
Reward for following program, not for staying dry
If
not working refer to urologist MD for
testing and treatment which might include
RBUS, VCUG, MRI, urinary flow measurement,
urodynamic testing
Medication
Pelvic floor relaxation techniques
Biofeedback
Electrical stimulation therapy, botox injection,
surgery,, intermittent clean catheterization
If not treated risk high pressures, complications
thereof – some feel all need urologist
Subcommittee on Urinary Tract Infection and Steering
Committee on Quality Improvement and
Management. “Urinary Tract Infection: Clinical
Practice Guideline for the Diagnosis and Management
of the Initial UTI in Febrile Infants and Children 2 to
24 months.” Pediatrics accessed 1/20/2014 at
http://pediatrics.aappublications.org/content/early/
2011/08/24/peds.2011-1330
Allen HA. “Fever without a source in children 3 to 36
months of age.” UpToDate accessed 1/17/2014
http://www.uptodate.com/contents/fever-withouta-source-in-children-3-to-36-months-ofage?source=search_result&search=fever+without+a+s
ource&selectedTitle=1%7E15
McLorie G, Herrin JT. “Management of vesicoureteral reflux.
UpToDate accessed 1/16/2014 at
http://www.uptodate.com/contents/management-ofvesicoureteralreflux?source=search_result&search=Management+of+vesicou
reteral&selectedTitle=1%7E68
McLorie G, Herrin JT. “Presentation, diagnosis and clinical
course of vesicoureteral reflux.” UpToDate accessed
1/16/2014 at
http://www.uptodate.com/contents/presentation-diagnosisand-clinical-course-of-vesicoureteralreflux?source=search_result&search=presentation%2C+diagno
sis+adn+clinical+course+of+vesicoureteral+reflux&selectedTit
le=1%7E150
Nepple KG, Cooper CS. “Etiology and clinical features of
bladder dysfunction in children.” UpToDate accessed
1/16/2014 at http://www.uptodate.com/contents/etiologyand-clinical-features-of-bladder-dysfunction-inchildren?source=search_result&search=bladder+dysfunction&s
electedTitle=3%7E150
Nepple KG, Cooper CS. “Evaluation and diagnosis of
bladder dysfunction in children.” UpToDate accessed
1/16/2014 at
http://www.uptodate.com/contents/evaluation-anddiagnosis-of-bladder-dysfunction-inchildren?source=search_result&search=bladder+dysfunct
ion&selectedTitle=4%7E150
Nepple KG, Cooper CS. “Management of bladder
dysfunction in children.” Uptodate accessed 1/16/2014
at http://www.uptodate.com/contents/managementof-bladder-dysfunction-inchildren?source=search_result&search=bladder+dysfunct
ion&selectedTitle=6%7E150
O’Donovan DJ. “Urinary tract infections in newborns.”
Uptodate accessed 1/20/2014 at
http://www.uptodate.com/contents/urinary-tractinfections-innewborns?source=search_result&search=urinary+tract+i
nfection+in+newborns&selectedTitle=1%7E150
Palazzi DL and Campbell JR. “Acute cystitis in children older than two years and
adolescents.” UpToDate accessed 1/20/2014 at
http://www.uptodate.com/contents/acute-cystitis-in-children-older-than-twoyears-andadolescents?source=search_result&search=acute+cystitis&selectedTitle=2%7E74
Roberts KB. “AAP Guideline for the Diagnosis and Management of UTIs in Febrile
infants.” Pediatric Care Online Accessed 1/17/2014 at
www2.aap.org/pcorss/webinars/pco/AAP%20Webinar_UTI-Roberts-Final.ppt
Shaikh N, Hoberman A. “Urinary tract infections in Infants and children older than
one month: acute management, imaging, and prognosis.” UpToDate accessed
1/20/2014 at http://www.uptodate.com/contents/urinary-tract-infections-ininfants-and-children-older-than-one-month-acute-management-imaging-andprognosis?source=search_result&search=uti+in+children&selectedTitle=1%7E150
Shaikh N, Hoberman A. “Long-term management and prevention of urinary tract
infections in children. UpToDate accessed 1/20/2014 at
http://www.uptodate.com/contents/long-term-management-and-prevention-ofurinary-tract-infections-inchildren?source=search_result&search=uti+in+children&selectedTitle=5%7E150
Shaikh N, Hoberman A. “Urinary tract infections in
infants and children older than one month: clinical
features and diagnosis.” UpToDate Accessed 1/20/2014
at http://www.uptodate.com/contents/urinary-tractinfections-in-infants-and-children-older-than-onemonth-clinical-features-anddiagnosis?source=search_result&search=uti+in+children
&selectedTitle=2%7E150
Shaikh N, Hoberman A. “Urinary tract infections in
children: epidemiology and risk factors.” UpToDate
accessed 1/20/2014 at
http://www.uptodate.com/contents/urinary-tractinfections-in-children-epidemiology-and-riskfactors?source=search_result&search=uti+in+children&s
electedTitle=3%7E150
Narrowest
coverage possible