Transfusion_Dr Kate Pendry_Nov13
advertisement

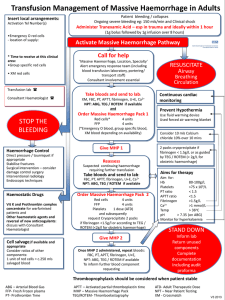
Transfusion for Medical Students Nov 2013 Requesting blood for transfusion • What is a group and screen test? The patient’s blood group is checked and an antibody screen is performed on the patient’s plasma. The sample can be kept in the lab for up to 6 days and then a crossmatch can be subsequently requested • What is a crossmatch test? The patient’s plasma is mixed with the donor’s red cells to make sure there is compatibility. When ordering state amount, time required, urgent / routine (look at surgical blood order schedule for elective surgery) Case 1: 27-year-old patient has a massive post-partum haemorrhage with severe hypotension. • Emergency Gp O RhD negative blood does not need to be crossmatched T • Fully crossmatched blood would take 45 mins to be made available F • If O RhD blood is given there is no need to take a crossmatch sample F • Group specific blood can be made available in 1530 mins REQUESTING BLOOD Extreme emergency only Pre transfusion testing ASSESS URGENCY On receipt of the the right pre-transfusion Choose products sample the following steps are undertaken: •Check the historical records •Group: Identify ABO and RhD group Allocate a lead to plasma liaise with •Screen: Check for lab & porters antibodies •Crossmatch: Select component COMMUNICATE AVOID ERRORS The patient’s serum or plasma can beCareful savedbedside for up labelling to 6 days in case later cross-match is XM, FBC, coag screen – swiftly to lab required Group O Important antibodies may cause reaction Valuable resource ~15mins from sample arriving Group specific ABO & RhD compatible Important antibodies may cause reaction Safest product if time allows Crossmatched Fully screened for antibodies ~45-60 mins from sample arriving Preempt need for FFP (30mins to thaw; 12-15mL/kg = 4 units for average adult) Preempt need for platelets Transfusion Management of Massive Haemorrhage Insert Insert local local arrangements: arrangements: Activation Activation Tel Tel Number(s) Number(s) •Emergency •Emergency O O red red cells cells -- location location of of supply: supply: ** Time Time to to receive receive at at this this clinical clinical area: area: •Group •Group specific specific red red cells cells •• XM XM red red cells cells Transfusion Transfusion lab lab Consultant Consultant Haematologist Haematologist Patient Patient bleeding bleeding // collapses collapses Ongoing Ongoing severe severe bleeding bleeding eg: eg: 150 150 mls/min mls/min and and Clinical Clinical shock shock Administer Administer Tranexamic Tranexamic Acid Acid (1g (1g bolus bolus followed followed by by 1g 1g infusion infusion over over 88 hours) hours) Haemorrhage Haemorrhage Control Control Direct Direct pressure pressure // tourniquet tourniquet ifif appropriate appropriate Stabilise Stabilise fractures fractures Surgical Surgical intervention intervention –– consider consider damage damage control control surgery surgery Interventional Interventional radiology radiology Endoscopic Endoscopic techniques techniques Haemostatic Haemostatic Drugs Drugs Vit Vit KK and and Prothrombin Prothrombin complex complex concentrate concentrate for for warfarinised warfarinised patients patients and and Other Other haemostatic haemostatic agents: agents: discuss discuss with with Consultant Consultant Haematologist Haematologist Cell Cell salvage salvage ifif available available and and appropriate appropriate Consider Consider ratios ratios of of other other components: components: 11 unit unit of of red red cells cells == c.250 c.250 mls mls salvaged salvaged blood blood Resuscitate, call for help Activate Massive Haemorrhage Pathway Call for help ‘Massive ‘Massive Haemorrhage, Haemorrhage, Location, Location, Specialty’ Specialty’ Alert Alert emergency emergency response response team team (including (including blood blood transfusion transfusion laboratory, laboratory, portering/ portering/ transport transport staff) staff) Consultant Consultant involvement involvement essential essential Take Take bloods bloods and and send send to to lab lab:: 2+ XM, XM, FBC, FBC, PT, PT, APTT, APTT, fibrinogen, fibrinogen, U+E, U+E, Ca Ca2+ NPT: NPT: ABG, ABG, TEG TEG // ROTEM ROTEM ifif available available and and Order Order Massive Massive Haemorrhage Haemorrhage Pack Pack 11 STOP THE BLEEDING Red 44 units Red cells* cells* units FFP 44 units FFP units Platelets 11 dose Platelets dose (ATD) (ATD) (*Emergency (*Emergency O O blood, blood, group group specific specific blood, blood, XM XM blood blood depending depending on on availability) availability) Give Give MHP MHP 11 Reassess Reassess Suspected Suspected continuing continuing haemorrhage haemorrhage requiring requiring further further transfusion transfusion Take Take bloods bloods and and send send to to lab lab:: 2+ FBC, FBC, PT, PT, APTT, APTT, fibrinogen, fibrinogen, U+E, U+E, Ca Ca2+ NPT: NPT: ABG, ABG, TEG TEG // ROTEM ROTEM ifif available available Order Order Massive Massive Haemorrhage Haemorrhage Pack Pack 22 Red 44 units Red cells cells units FFP 44 units FFP units Platelets 11 dose Platelets dose (ATD) (ATD) and and subsequently subsequently request request Cryoprecipitate Cryoprecipitate 22 packs packs ifif fibrinogen fibrinogen <1.5g/l <1.5g/l or or according according to to TEG TEG // ROTEM ROTEM Give Give MHP MHP 22 Once Once MHP MHP 22 administered, administered, repeat repeat bloods: bloods: FBC, FBC, PT, PT, APTT, APTT, fibrinogen, fibrinogen, U+E, U+E, NPT: NPT: ABG, ABG, TEG TEG // ROTEM ROTEM ifif available available To To inform inform further further blood blood component component requesting requesting RESUSCITATE Airway Stop the bleeding – TXA, PCC Breathing Circulation Continuous Continuous cardiac cardiac monitoring monitoring Team approach Prevent Prevent Hypothermia Hypothermia Use Use fluid fluid warming warming device device Used Used forced forced air air warming warming blanket blanket Emergency runner Consider Consider 10 10 mls mls Calcium Calcium chloride chloride 10% 10% over over 10 10 mins mins Communicate with lab early and clearly 22 packs packs cryoprecipitate cryoprecipitate ifif fibrinogen fibrinogen << 1.5g/l 1.5g/l or or as as guided guided by by TEG TEG // ROTEM ROTEM Aims Aims for for therapy therapy Know where the Emergency O Neg is in your Trust Aim Aim for: for: Hb 8-10g/dl Hb 8-10g/dl Platelets >75 Platelets >75 xx 10 1099/l/l PT << 1.5 PT ratio ratio 1.5 APTT <1.5 APTT ratio ratio <1.5 Fibrinogen >1.5g/l Fibrinogen >1.5g/l 2+ 2+ Ca >1 Ca >1 mmol/l mmol/l Temp >> 36 Temp 36ooCC pH >> 7.35 pH 7.35 (on (on ABG) ABG) Monitor Monitor for for hyperkalaemia hyperkalaemia Massive haemorrhage packs 1 and 2 STAND DOWN Inform lab Return unused components Complete documentation Including audit proforma Monitor coag tests and move to goal directed therapy Thromboprophylaxis should be considered when patient stable ABG – Arterial Blood Gas FFP- Fresh Frozen plasma PT- Prothrombin Time Recognise blood loss APTT – Activated partial thromboplastin time MHP – Massive Haemorrhage Pack TEG/ROTEM- Thromboelastography ATD- Adult Therapeutic Dose NPT – Near Patient Testing XM - Crossmatch Stand down v1 2011 Case 2 67-year-old male, Mr Arvind Patel, (Group O) is admitted for elective hip replacement surgery. His Hb is 100 g/L. Because of excessive bleeding on the operating table the Consultant Anaesthetist asks for 2 units of blood. The theatre nurse collects 2 units of red cells labelled for Mr Suhail Patel and starts transfusion. Mr Suhail Patel is Group B. What are the potential clinical consequences for Mr Arvind Patel and how would they be managed? A. There would be no problems as it is safe to give Group B blood to a Group O donor so the transfusion could continue F B. The transfusion must be stopped immediately T C. The partially transfused bag must be returned to the lab with a blood sample from the patient T D. Oozing from venepuncture sites might be a sign of a transfusion reaction T Blood Groups Blood Group Antibodies A Anti-B B Anti-A AB None O Anti-A Anti-B RhD positive or RhD negative A B AB O How could the error have been avoided? A. The theatre nurse collecting the blood should make a note of the patient’s details so that she can identify the correct patient F B. The bag of blood should be checked against the patient’s notes F C. The bag of blood should be checked against the patient’s wrist band T D. There is no need to do the bedside check when the patient is anaesthetised F Could the transfusion have been avoided in the first place? A. Yes because this type of surgery is suitable for cell salvage T B. Yes because a Hb of 100g/L is a safe level for a 67 year old man F C. No because the Hb alone is not the only trigger for transfusion T D. Tranexamic acid would help to reduce blood loss in this situation T BLOOD “1 unit RBC” COMMON INDICATIONS Acute blood loss Only with significant blood volume loss Consider cell salvage Anaemia Hb < 70 g/L Likely requires transfusion Usual time: 3hrs 4hr limit from removal from cold storage to end of transfusion Blood warmer for rapid transfusions Refer to Trust Blood Transfusion Policy Consider correctible causes Anaemia Hb 70 - 100 g/L Consider correctible causes Transfuse if symptoms/needs eg IHD Pre-operative assessment Correction of anaemia reduces need for transfusion MBOS (Maximum Blood Ordering Schedule) Case 3: 17-year-old female with heavy periods presents with Hb of 50 g/L and MCV 55 fl. Would you give a blood transfusion? A. Yes, I would give a blood transfusion – that Hb level is very low F B. No, I wouldn’t give a blood transfusion because she will respond to an alternative therapy T C. Oral iron will increase the Hb by 40g in 1 week F Case 4: A full blood count states the platelet count to be ‘6 x 109/L’ with an associated peripheral blood film comment of ‘platelet clumping seen’. A prophylactic platelet transfusion (1ATD) is indicated as the platelet count is <10 x 109/L. T/F The answer is False Fresh Frozen Plasma (FFP) is the optimal treatment available to treat life-threatening bleeding in patients on warfarin T/F The answer is False Blood Components Red Cells Whole Blood Platelets (also apheresis) Plasma Fresh Frozen Plasma Cryoprecipitate Fractionation Factor concentrates Eg FVIII, FIX, PCC Immunoglobulin Albumin (Non UK Plasma) BLOOD COMPONENTS Fresh Frozen Plasma “1 unit FFP” Usual time: 30 mins/unit Needs 30 mins to thaw in lab Usual dose 12-15 mL/kg (4-6 units for average adult) Main indications: coagulopathy with bleeding/surgery, massive haemorrhage, TTP. Not warfarin reversal. Cryoprecipitate “1 pool cryoprecipitate” Usual time: 30 mins/bag Needs 30 mins to thaw in lab Adults: 1 pool = 5 donor units Usual adult dose: 2 pools (10 donor units) Main indication: coagulopathy with fibrinogen < 1.5 g/L Platelets Platelets Massive haemorrhage Keep platelet count above 75 x 109/l “1failure ATD platelets” Bone marrow platelet count <10 × 109/l 30 mins or <20Usual × 109/ltime: if additional risk, e.g. sepsis Prophylaxis for surgery 1hr limit Minor procedures 50 x 109/l; More major 80 x 109/l;dose CNS(ATD) or eye Usual dose: 1surgery adult treatment 9 surgery 100 x 10 /l Shelf-life only 7 days from donation Cardiopulmonary bypass should be readily available use only UsedPlatelets as prophylaxis or treatment of bleeding / pre if bleeding procedure in patients with thrombocytopenia Prothrombin Complex Concentrate (PCC) Plasma-derived Vit K dependent factors: II VII IX X For emergency reversal of life-threatening warfarin over-anticoagulation (do not use FFP) Issued by transfusion lab – supply in A&E See trust policy Special Blood Requirements • All patients with Hodgkin’s Disease should receive irradiated blood T • All patients born after 1996 should have virally inactivated, non-UK sourced Plasma T • All Stem Cell Transplant / Bone marrow transplant recipients require CMV negative blood F • Pregnant women have no special blood requirements, so there is no need to inform the transfusion laboratory of their pregnancy or gestation on the request form F SPECIAL REQUIREMENTS Fairly specific indications… Paeds, Haem, Onc, O&G… …but “it is the responsibility of the prescribing doctor” CMV NEGATIVE IRRADIATED To keep at-risk patients CMV free (~50% of us are CMV negative) To prevent transfusion-associated graft versus host disease (rare) in specific T-cell immunodeficiency cases Children < 1yr Intrauterine transfusions Intrauterine transfusions Congenital immunodeficiency Congenital immunodeficiency and unless known to be CMV IgG +ve: Hodgkin Lymphoma Pregnant women having elective transfusion Stem cell / marrow transplant patients After purine analogue chemo (eg: fludarabine) Refer to Trust Blood Transfusion Policy Risks of Transfusion • The risk of transmission of HIV with transfusion of red cells is 1 in 5 million donations in the UK (0.2 per million donations). T • A patient becomes acutely short of breath following a transfusion of FFP. Chest X-ray shows bilateral pulmonary infiltrates and you give diuretics with some effect. The case should be reported as a clinical incident via the hospital reporting system, so it can be followed up appropriately. T • All donors are now screened for vCJD F Risks of Transfusion • A patient complains of feeling unwell during their transfusion. Their observation chart shows their temperature, BP, pulse rate and respiratory rate to be stable. No specific action is required. F • A patient develops mild urticaria following a platelet transfusion. You should administer IV chlorphenamine (piriton) and IV hydrocortisone. F • Anaphylaxis is most likely to happen in the first 15 minutes of transfusion T Serious Adverse Events from blood transfusion reported in UK 1996-2011 Risk of giving wrong blood is much greater than transfusion transmitted infection TRANSFUSON REACTIONS Mild reaction Temp rise < 1.5°C Urticaria Rash Pruritis STOP TRANSFUSION Review obs Paracetamol Chlorpheniramine? Trust Blood Transfusion Policy Restart cautiously OR STOP TRANSFUSION Suspected www.transfusionguidelines.org.uk severe reaction Right patient? Right blood product? Pyrexia, rigors OR Hypotension Whole set to lab Loin / back pain New set with saline Ask for help Increasing anxiety Pain at the infusion site Full bloods as policy Respiratory distress Checklist (see policy) Dark urine Severe tachycardia Incident form Unexpected bleeding (DIC) Refer to Trust Blood Transfusion Policy Yes Severe / life-threatening •Call for urgent medical help •Initiate resuscitation- ABC •Discontinue transfusion and maintain venous access •Monitor the patient : TPR, BP, urinary output, oxygen sats Anaphylaxis follow anaphylaxis pathway If bacterial contamination policy likely start antibiotic treatment Inform hospital transfusion department Return unit and administration set to transfusion Perform appropriate investigations Not Life threatening or Severe Resources Trust Guidelines and Policies Your Hospital Transfusion Team The Transfusion Handbook www.transfusionguidelines.org.uk