Improving Bedside CPR Skills and Team Skills with In
advertisement

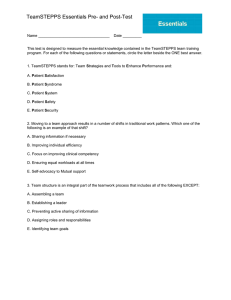
Paris Hotel and Casino Las Vegas, Nevada Improving Bedside CPR Skills and Team Skills with In-Situ Simulations Presented by: Jennifer Sweeney, MSN, RN, CEN Advanced Practice Program Coordinator Center for Advanced Surgery & Simulation Sarasota Memorial Health Care System Presenter Disclosure Information Jennifer Sweeney, MSN, RN, CEN Improving Bedside CPR Skills and Team Skills with In-Situ Simulations. No relevant financial relationships exist. Random In-situ Critical Event Simulation • Improving CPR skills and teamwork for providers at the hospital patient’s bedside. • This presentation will demonstrate the design and implementation of the program – Garnering stakeholder support. – Tools to produce measurable outcomes. – Results from 12 months of data collection. Background • SMHCS is a 806-bed regional medical center. – 4,000 staff, 802 physicians • Large simulation center with 8 High fidelity simulators, 1 Program Coordinator, 0 Simulation Technicians • Florida “seasons” make in-lab training difficult to schedule most of the year. • Financial constraints necessitated driving the simulation program out to the bedside. Problem: • Needs assessment revealed concern with direct care providers’ comfort and confidence with recognizing and responding to emergent patient care situations. • Concern with cost involved with lengthy simulation classes, loss of productive time, scheduling concerns, etc. • Fear in the first five minutes. Solution: • Short critical event scenarios are simulated in the actual areas these events may take place. • TeamSTEPPS principles integrated into scenario planning and debriefing. • Simulations last no longer than 20 minutes including pre-briefing, conduction of the simulation, and debriefing of all providers involved. • Results shared with the unit educator and manager for further review, in–depth debriefing, and ongoing staff education. TeamSTEPPS: • Team Strategies and Tools to Enhance Performance and Patient Safety • FREE, Evidence-based teamwork system aimed at optimizing patient outcomes by improving communication and teamwork skills among health care professionals. • http://teamstepps.ahrq.gov/ Scenario Selection • • • • • • Interdisciplinary Short critical events IN-SITU Impromptu What scare you the most? Focus on patient safety and teamwork! Garnering Support - Keep it quick: in and out as fast as possible. Meaningful: set clear and realistic objectives. Interprofessional: look for your champions. Budget neutral: high fidelity, low fidelity, no fidelity. FOCUSED on PATIENT SAFETY. Build it (Hype it) and they shall come! Implementation Conducted in-situ for no longer than 20 minutes with any/all health care team members working at that time: - 10 minutes for conduction of the Video recorded for educational review at a later time (staff meeting, huddle, end of shift). simulated event and 10 minutes for debriefing of all providers involved. Debriefing focused on identification and immediate correction of latent safety threats and principles of TeamSTEPPS. Just do it! The program and results sell themselves! Always have “crowd controllers” to communicate with patients and visitors during the exercise. Big crowd pleaser! RISCE Simulation in OB ECC Goal: Test new communication plan for rapidly summoning help to new unit and overall emergency preparedness of new unit. MD RN RT Time: 8 minute Scenario, 5 minute Debrief Debriefing: Latent Safety Threat Identified: Operator paged out location incorrectly causing delay in arrival of NICU Team. Follow up meeting scheduled that day to correct. TeamSTEPPS: Excellent demonstration of Mutual SupportConcern voiced by physician to increase speed of compressions. Team did not respond. Physician began counting cadence aloud. Room for improvement noted in use of call outs and check backs between Respiratory Therapist and Nurse. Evaluation Tool Selection: - Quantitative Data for the number crunchers. Qualitative data for the emotional impact. Baseline data to compare to ongoing data. Look for tools that are already validated, reliable, have been utilized in other programs, etc. - TeamSTEPPS tools. Outcomes • Post-RISCE participant evaluation tool: – Perceptions are evaluated per session and for improvements over time. • Review of the RISCE simulation video: – TeamSTEPPS behaviors • Scored as consistently applied ‘1’, inconsistently applied ‘0.5’, or absent ‘0’. – BLS/ ACLS guidelines: • Recommended practice is compared to actual performance. – Video breakdown 3/29/2012 6/10/2012 9/13/2012 12/16/2012 2/4/2013 Start time to recognition 0 10 10 15 10 Start time to call for help 0 30 10 15 25 Start time to start CPR 50 60 30 42 33 Start to arrival of AED 100 140 65 60 60 Start to use of AED 150 170 95 97 86 Start to Code Blue arrival 210 140 65 180 95 Compressor 1 time before switch 140 220 60 200 150 Time off chest 1 20 40 15 18 20 Time off chest 2 10 30 12 30 10 Time off chest 3 35 Time off chest 4 12 Compressor 2 time before switch Safety threat 1 Safety threat 2 Safety threat 3 Safety threat 4 20 Order should be directed to a particular person, then repeated back by that person. long delay from Poor closed loop recognition to response communication long time off chest Long breaks in chest compressions Multiple calls made to ensure code team and NICU team were en route, need better closed loop communication Infant resuscitation area missing needle decompression supplies Code Blue did not have badge access through new door RN did not visually clear team before delivering shock. Questions? Jennifer Sweeney, MSN, RN, CEN Sarasota Memorial Health Care System Jennifer-sweeney@smh.com 941-917-1761 References • Edelson DP, Litzinger B, Arora V, Walsh D, Salem K, Lauderdale DS, Vanden Hoek TL, Becker LB, Abella BS. (2008). Improving In-Hospital Cardiac Arrest Process and Outcomes With Performance Debriefing. Arch Intern Med.168(10):1063-1069. • Gillespie BM, Chaboyer W, Murray P. (2010). Enhancing communication in surgery through team training interventions: a systematic literature review. AORN J. 92:642-657. • Halverson AL, Andersson JL, Anderson K, Lombardo J, Park CS, Rademaker AW, Moorman DW. (2009). Surgical Team Training: The Northwestern Memorial Hospital Experience. Arch Surg.144(2):107112. • Siassakos D, Bristow K, Draycott TJ, Angouri J, Hambly H, Winter C, Crofts JF, Hunt LP, Fox R. (2011). Clinical efficiency in a simulated emergency and relationship to team behaviours: a multisite crosssectional study. Simul Healthc. 6(3):143-9.