VDR-4 * A Case Study
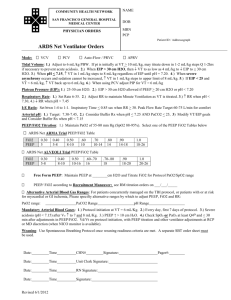
advertisement

David Albecker, BS, RRT-NPS, RPFT RT Clinical Programs Manager Winchester Medical Center I have no financial interest in any device, ventilator, corporation, method, rehab facility, or therapy, mentioned in this presentation, and no conflicts of interest. David Albecker (April, 2012) • 58 year old female w/ Hx of COPD and long-term tobacco use • Bilateral CAP • Septic shock → ARDS – – – – – BP ≈ 72/53 Febrile pH ≈ 7.0 Thick, yellow pulm secretions CXR – bilateral infiltrates all 4 lung quadrants • NSTEMI during critical illness complicated the case • • • • • IV Fluid Bolus Multiple Antibiotics Multiple Vasopressors Heavy sedation Increasing vent support w/ FiO2 of 1.0 • Changed to HFPV w/ VDR-4 on day #2 • 6 days on VDR-4 – ABG improved – FiO2 ↓ from 1.0 to 0.4 – CXR improved • Refractory hypoxemia that was not improving with conventional VC A/C • Copious thick, yellow pulmonary secretions • In our opinion, starting the VDR-4 in ARDS is better done sooner than later • APRV: the heavy sedation meant she would not breathe spontaneously in the Thigh phase - important for CO2 clearance in APRV 1 • 3100B: active exhalation can cause gas trapping in severe COPD pts2; & high, steady MAP may ↓ venous return/CO Date: 2012 Ventilator Mode 4/11 VC-A/C 4/11 VC-A/C 4/12 VC-A/C 4/12 HFPV 4/13 HFPV 4/14 HFPV 4/15 HFPV 4/16 HFPV 4/17 HFPV 4/18 VC-A/C Rate 16 22 24 15 15 15 15 15 15 14 PEEP 12 12 12 12 12 12 12 12 8 10 Tidal Volume (ml) 400 400 500 FiO2 Percussive rate (frequency/min) 0.9 0.9 1.0 500 0.9 600 0.85 500 0.7 500 0.6 500 0.5 500 0.4 500 Inspiratory Time (sec) 2 2 2 2 2 2 Expiratory Time (sec) 2 2 2 2 2 2 Peak Pressure 34 34 34 34 34 34 0.6 pH PaCO2 7.04 64 7.02 67 7.15 40 7.25 45 7.37 36 7.32 37 7.26 46 7.30 43 7.32 42 7.45 41 PaO2 78 78 71 70 87 105 90 94 58 67 HCO3 17 17 14 20 21 19 20 21 22 28 BE -14 -15 -14 -8 -4 -7 -7 -5 -4 +4 SaO2 Lactate (mM/L) Change made after ABG 88% 2.8 87% 2.7 88% 91% 96% 98% 95% 1.2 96% 87% 94% 0.8 on 4/23 ↑ rate to ↑rate to change to ↓ FiO2 to 0.85, ↓ FiO2 to ↓ FiO2 to ↓ FiO2 to ↓ FiO2 to change 22 24, ↑tidal HFPV with ↓ percussive 0.7 0.6 0.5 0.4, ↓ back to vol to VDR-4 rate to PEEP to VC- A/C on 500ml, 500/min 10, then 8 4/18 ↑FiO2 to 1.0 3 pressure levels • Add 5-10 cmH2O above PIP for recruitment, but you can add it without ↑PIP. • “Gives the lung time to get out of its own way” – Slow-responding lung areas • Philosophy Issue: – Start w/ convective rise – Add it only for recruitment • VC A/C Settings: – – – – – VT = 6ml/kg IBW Measured Pplat = ? Rate = ? PEEP = ? FiO2 = ? – Observe MAP & ABG • Same for PC A/C except use PIP rather than Pplat • HFPV Settings: – Consider MAP & ABG on VC A/C • PIP ≈ Pplat on VC A/C – Good chest rise? • PEEP ≈ PEEP on VC A/C • I-Time = 2 sec – E-Time = 2 sec – Percussive rate=600/min • FiO2 ≈ FiO2 on VC A/C – Or 100% ( for transition) • Convective Rise ? • APRV Settings: • The “Habashi way” – – – – – PHIGH = ? PLow = 0 THigh ≈ 4-6 sec TLow ≈ 0.8 sec FiO2 = ? – Observe MAP & ABG • HFPV (VDR-4) Settings: – Consider MAP & ABG • PIP (AIP) ≈ PHIGH from APRV – Good chest rise? • PEEP ≈ 10-18 – Consider MAP & TLow exp flow inflection point • I-Time = 2 sec – E-Time = 2 sec – Percussive rate=600/min • FiO2 ≈ FiO2 on APRV – Or 100% for transition • Pinch ETT • Convective Rise? • If pt not breathing spontaneously, hard to manage CO2 w/ APRV (heavily sedated ARDS pt) • This inflection pt determines end-exp lung volume in APRV and, w/ MAP, helps determine PEEP (AEP) setting on the VDR-4 • Example: HFOV w/ 3100B • HFPV settings: remove cuff leak if it was used w/ 3100B • Consider 3100B MAP when setting VDR-4 PEEP – MAP = 34 cm H2O – Amplitude = 90 cm H2O • Ventilation difficulty – FiO2 = ? – Hz = 3, 4, 5, or 6 – higher HFOV MAP → higher VDR-4 PEEP • Ventilation difficulty – % I-time = 33% (no concern) – Cuff leak? Ventilation difficulty • VDR-4 will ventilate better than 3100B • Consider: tops of Amplitude pressure spikes ≈ 79 cm H2O – Bottom of Amp waveform could be -10 cm H2O! • Observe MAP & ABG • Monitron PIP may ≈ 3100B top of Amplitude waveform – AIP on VDR-4 (sustained PIP) will be lower & clinically usable – Good chest rise? • • Match FiO2 (or 100% for transition) I-time= E-time = 2 sec – Percussive rate = 600 • Convective Rise? Pinch ETT • Observe MAP from 3100B • Set VDR-4 PEEP (AEP on Multimeter) as high as physician comfort allows • Then adjust VDR-4 PIP (AIP on Multimeter) high enough to get similar MAP as with 3100B • Downside: If you underestimate PEEP, you will overshoot on PIP in order to get target MAP – this can be similar to ARDSnet fail VC A/C w/ low PEEP and high tidal volume. – Use ARDS Peep/FiO2 table rather than physician comfort level Dedicated Expiratory Half-Cycle on VDR-4 allows ETCO2 measurement • Delivered tidal volume w/ VDR-4 allows effective MDI/aerosol use • Similar to VC or PC w/ conventional vent • For MDI, time inhalation w/ inspiratory phase – We place MDI adaptor between Phasitron and ETT/trach • Aerosol med through Aerogen neb – We place between insp limb of circuit and green insp port of Phasitron, can also go between ETT/Trach and Phasitron • Cuff Leak not required or used for ventilation w/ the VDR-4. Many better ways to ↓ CO2: • • • • ↑PIP (or ↓ PEEP if oxygenation allows) to ↑∆P Add Convective pressure rise to ↑ ∆P Decrease percussive rate from 600 to 450 (for COPD pt) Increase sinusoidal E-time allowing for better exhalation • ↑ PEEP • Add Convective Pressure Rise (recruitment maneuver) • ↑ percussive rate from 600 to 750 • ↑ sinusoidal I-time (for pt without COPD) which creates APRV-like pressure waveform • ↑ FiO2 You must pay close attention to humidity Passover + Aeroneb Solo – similar to disposable circuit + Passover Phasitron w/ Aerogen neb Complete circuit w/2 humidifiers Aerogen neb FP Passover Pumps w/ Syringes Aeroneb Driver Flolan pump Saline pump Connection to VDR-4: extension sets from syringes attach to 3-way stopcock @ Aeroneb Solo which runs in continuous mode Next 3 slides come from Brent Kenney’s presentation We use this only as a back-up for Flolan in adult ICU Adaptor placed between Phasitron and ETT/trach Adaptor w/ connecting tubes in place Blended gas to INOblender, then flow out to adaptor @ Phasitron. Sample line to INOmax sample line inlet port. INO concentration measured in standard way but adjustments made @ INOblender • Pathway that we follow for the difficult-tooxygenate pt • By the time we get to ECMO, we are almost always on the VDR-4 • We have a partnership w/ VCU for ECMO pts in adult ICU • Experienced physician champion is a must (for us it was Dr Barillo) • We developed a HFPV protocol for adult ICU • I did short, introductory inservices for as many ICU nurses as possible (both shifts) on HFPV w/ VDR-4 • We did more complete inservices for all ICU RTs • On a predetermined go-live date we started pt care • Yearly mandatory education is a must for ICU RTs • We have a protocol for the resp care of the spinal cord injured (SCI) pt • After the initial acute phase, how do you maintain lung clearance and expansion longterm for vent-dependent SCI pt? • IPV + Cough Assist = Perfect! Why IPV? – Next slide… • Kessler Institute for Rehabilitation was recently ranked #2 in USA for rehab facilities by U.S. News & World Report. • Mike Feinberg (Resp Care Manager for Kessler Institute) helped us develop our SCI protocol. Here is what he sent us: – “There is no conclusive literature that states a non surgically fixed spinal cord injury patient is safe for the vest.” • Our conclusion: This is an expert opinion and should not take the place of a review of the published studies, but we do not use any device that externally vibrates or shakes these patients (Vest, CPT thru the bed, etc). • Story of Ms. M and trauma from falling tree • VDR-4 as Primary vent for status-asthmaticus pts in acute, severe respiratory failure • High energy inspiratory gas takes center of tube where resistance is the lowest. • Passive exhalation • “…all intubated asthmatics are put on the VDR. We usually start with our traditional settings, and will increase the Pulsatile flow and reduce the Oscillatory PEEP to increase the pressure gradient to overcome the high airway resistance. That awesome “Accelerated Laminar Flow” takes over and ventilation happens.” –Denny Gish (Legacy Emanuel Med Ctr) • Questions? • We share all of our protocols. Please contact me at: dalbecke@valleyhealthlink.com • References: (from case report on slide #4) 1. 2. Habashi NM. Other approaches to open-lung ventilation: Airway Pressure Release Ventilation. Crit Care Med. 2005 Mar; 33(3 Suppl): S228-40. 3100B High Frequency Oscillatory Ventilator owner’s manual. CareFusion. Revision P. Chapter 1 – Warnings; page 2. • Thank You.