aoda_tobacco - Center for Tobacco Research and Intervention
advertisement
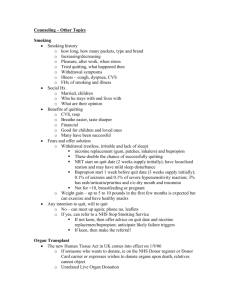
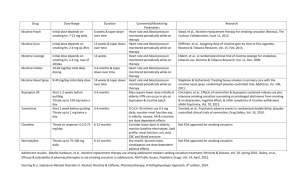
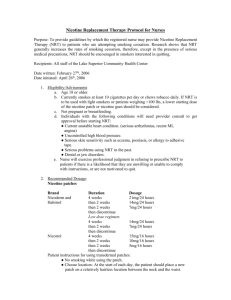
Treating Nicotine Dependence in Patients with Addictive Disorders Eric Heiligenstein, M.D. Director of Psychiatry University Health Services University of Wisconsin-Madison • Evidence of effective strategies for addressing the disproportionate rate of tobacco use among smokers with cooccurring addictive disorders is lacking • The 2008 update of the US Clinical Practice Guidelines for treating tobacco dependence was informed by more than 8700 tobacco control studies • Fewer than 2 dozen randomized controlled trials have focused on smokers with addictive disorders • Smokers with mental illness or substance use disorders are among the most likely to be excluded from clinical trials because they are viewed as too complicated • That said, we cannot continue to overlook the epidemic of tobacco dependence that has plagued persons with substance use disorders • The following recommendations are based on the best available evidence and national expert consensus panels Treatment Principles for Nicotine Dependence in MHA • All smokers trying to quit should be encouraged to use both counseling and medication1 – Counseling and medication in combination are more effective than either alone • Dose level and duration of drug treatment individualized • Many will need – Higher doses of medication – Longer duration of treatment – Combination treatments 1. PHS Clinical Practice Guideline, 2008 Clinical Solutions: Treating Nicotine Dependence in MHA • Traditional cessation treatments may be inadequate – Flexibility in setting quit date – Reduced smoking to reach abstinence – Practice quit attempts – Combination and tailored treatments (behavioral & medical) Peters & Hughes, 2009; McFall et al, 2010 Determining Readiness to Proceed • Motivation – “Interested” is sufficient – Don’t rule out initiating some type of intervention if not motivated to quit now • Stability – Need to be psychiatrically stable-do not need to be in full remission – No major medication changes – No major life changes – No active intoxication/withdrawal; consumer/client in recovery process Nicotine-Drug Interactions • Smoking induces CYP1A2 isoenzyme – Approximately doubles clearance of • Antipsychotics: fluphenazine, haloperidol, olanzapine, clozapine, chlorpromazine • Antidepressants: amitriptyline, nortriptyline, imipramine, clomipramine, doxepin, fluvoxamine • Cessation may produce rapid, significant increase in blood levels • Need to monitor for increased side effects First-line Pharmacotherapies • • • • • • • Nicotine patch Nicotine gum Nicotine lozenge Nicotine inhaler Nicotine nasal spray Buproprion SR Varenicline Reasons for Using NRT • It helps the person feel more comfortable (treats nicotine withdrawal syndrome). • It is very safe: the person is getting “clean” nicotine instead of “dirty” nicotine with 4000 plus chemicals. 11 NRT Combinations • Provide an increase in long-term quit rates (42%) • Limited safety concerns • Which combinations? – Patch + patch – Patch + oral product – Oral product + oral product Pre-Quit Use of NRT (Patch) • Starting patch 2 weeks before quitting increases the odds of quitting about 4 fold • Weakens link between smoking and pleasure • Need to switch to low-nicotine cigarettes NRT Summary • NRT increases the odds of quitting about 2 fold • Long-term and high-dose NRT (patch) may not produce added benefit beyond regular dose (14-25 mg) and duration (614 weeks) 14 Bupropion SR • Atypical antidepressant that acts as a norepinephrine and dopamine reuptake inhibitor • Is a nicotinic antagonist that prevents cravings and withdrawal symptoms Bupropion SR • Dose response efficacy in treating smokers • Attenuates weight gain • Can be prescribed to diverse populations of smokers with expected comparable results Hays JT & Ebbert JO. Mayo Clin Proc 78:1020, 2003 Bupropion SR Summary • Bupropion SR increases the odds of quitting about 2 fold • Insufficient evidence that adding Bupropion SR to NRT provides an additional long-term benefit • Extended therapy with Bupropion SR to prevent relapse after initial cessation has not find evidence of a significant long-term benefit • Trials comparing Bupropion SR to Varenicline showed a lower odds of quitting with Bupropion SR • Concerns that Bupropion SR may increase suicide risk are currently unproven Varenicline • Varenicline is a partial agonist activating the α4β2 nAChR subtypes to prevent cravings and withdrawal symptoms • It also acts as a partial antagonist by occupying receptor sites and blocking nicotine binding leading to a reduction in the satisfaction gained by smoking Varenicline Summary • Varenicline at standard dose increased the chances of successful long-term smoking cessation between two- and threefold • Lower dose regimens also conferred benefits for cessation, while reducing the incidence of adverse events • More patients quit successfully with Varenicline than with Bupropion • Limited evidence suggests that Varenicline may have a role to play in relapse prevention • Possible links with serious adverse events, including depressed mood, agitation and suicidal thoughts, have been reported but are so far not substantiated Behavioral Toxicity and Pharmacotherapy for Nicotine Dependence • Bupropion SR and Varenicline have slight risk for suicide or attempts (1.12 OR; 1.17 OR), and suicidal ideation (1.20 OR; 1.43.OR) • Untreated nicotine withdrawal can cause adverse behavioral changes, including suicidal ideation • All patients should be informed of this potential when treatment is discussed • Half of all smokers who don’t stop by middle age will die from a tobacco-related disease Gunnell, et al, 2009 Smoking and Substance Use Disorders • The research on the association between smoking and substance use outcomes is limited by a lack of longer follow-ups • Most studies have not exceed 18 months and none examined prospectively the impact of smoking on long-term outcomes Treating Nicotine Dependence in SUD • Smoking cessation attempts or concurrent smoking cessation and substance use treatment does not interfere with recovery from substance use disorders • Stopping smoking during the first year after substance use treatment predicted better long-term substance use outcomes through 9 years after intake Burling et al, 1996; Cooney et al, 2009; Tsoh et al, 2010 Treating Nicotine Dependence in SUD • Standard combinations of behavioral and pharmacological treatment (e.g., weekly counseling plus NRT) have produced disappointing results in alcoholic smokers • Bupropion SR not effective in one trial • Combination NRT, Naltrexone, Topiramate, and Varenicline hold promise Kalman et al, 2006; Hays et al, 2009; Cooney et al , 2009; Ebbert et al 2009; Johnson et al, 2005; O’Malley et al, 2006 Unique Tobacco Treatment Needs • Determine need for involvement from primary care/other health care providers • Determine need for more intensive behavioral therapy • Address psychotropic medication issues • Tailor treatment plan based on – – – – Current symptoms/recovery Functional status Current psychotropic medications Previous quit history – Stage of readiness – Level of impairment/functional status