Cyanotic CHD
advertisement

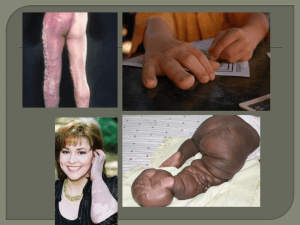
Congenital Heart Disease Incidence and Etiology Incidence of 1% in general population. VSD is most common CHD TOF is most common cyanotic CHD TGA is most common cyanotic CHD presenting in infancy Etiology: Multifactorial inheritance 90%. Chromosomal 5% Single mutant gene 3% Environmental 2% Presentations Asymptomatic heart murmer Cyanosis Congestive heart failure Syncope Shock CHD in Chromosomal Aberrations Trisomy 21 Trisomy 18 Trisomy 13 XO Turner Incidence Most common lesion 50% VSD or A-V canal 90+% VSD 90% VSD 35% CoA CHD in Single Mutant Gene Syndromes Marfan’s Noonan’s Williams’ Holt-Oram NF Aortic aneurysm PS, ASD Supravalvular AS ASD, VSD PS, CoA Teratogens and CHD Alcohol Phenytoin Lithium Rubella Diabetes Frequency 25-30% 2-3% 10% 35% 3-5% Most common VSD PS,AS,CoA,PDA Ebstein PPS, PDA Hypertrophic septum TGA, VSD, CoA (Incidence can be as high as 30-50% in poorly controlled DM) Lupus PKU 50% 25-50% 3rd degree heart block TOF, VSD, ASD Presentations Asymptomatic (heart murmur) Cyanosis Congestive heart failure Syncope Shock Small VSD, ASD D-TGA, TOF Large L-R shunt lesions AS, PS Coarc, hypoplastic left heart Birth VSD ASD| PDA CoA AS HLHS TOF TriA/S PA TGA TA TAPVR 2w 8w 4m 1y 3-5y Adolescence CHF P. HTN P. HTN CHF Often asymptomatic Shock Shock CHF/HTN CHF CHF/syncope/murmur Shock Cyanosis CHF Shock/Cyanosis Shock/Cyanosis Cyanosis HLHS=Hypoplastic left heart syndrome Cyanosis/CHF Shock/Cyanosis TriA/S=Tricuspid atresia CHF=Congestive heart failure P.HTN=Pulmonary hypertension FTT=Failure to thrive Cyanotic CHD 1. Truncus Arteriosus 2. Transposition of the Great Arteries 3. Tricuspid Atresia 4. Tetralogy of Fallot 5. Total Anomalous Pulmonary Venous Return Acyanotic CHD 1. VSD 2. ASD 3. PDA 4. Coarctation Aorta 5. Aortic Stenosis 6. Hypoplastic Left Heart Cyanotic CHD with Decreased Pulmonary Blood Flow 1. Tetralogy of Fallot 2. Tricuspid Atresia 3. Total Anomalous Pulmonary Venous Return with obstruction Cyanotic CHD with Increased Pulmonary Blood Flow 1. Transposition of the Great Arteries 2. Truncus Arteriosus 3. Total Anomalous Venous Return without obstruction Acyanotic CHD with Increased Pulmonary Blood Flow (Volume Load) 1. ASD 2. VSD 3. PDA Acyanotic CHD with Pulmonary Venous Congestion or Normal Blood Flow (Pressure Load) 1. 2. 3. 4. Coarctation Aorta Aortic Stenosis Hypoplastic Left Heart Pulmonary Stenosis Circulation before birth Circulation after birth Cyanotic CHD with Decreased Pulmonary Blood Flow 1. Tetralogy of Fallot 2. Tricuspid Atresia Tetralogy of Fallot 1. 2. 3. 4. VSD Pulmonary artery stenosis Overriding aorta Right ventricular hypertrophy Tetralogy of Fallot • Incidence of total CHD • Age at presentation • Clinical • Auscultation • • • • • • Most common cyanotic CHD Usually by 6 months Cyanosis Cyanotic spells (squatting) Harsh systolic murmur Softer if worsening obstruction Tetralogy of Fallot • Radiology • EKG • • • • Decreased pulmonary vascularity Boot-shaped heart R-sided aortic arch RAD, RAE, RVH TOF treatment 1. For cyanotic spells: Knee-chest position Morphine sulfate Vasoconstrictors Propranolol 2. Iron for anemia 3. Surgical a. Palliation Blalock-Taussig Waterston shunt Pott’s operation b. Corrective at 1-5 years of age Tetralogy of Fallot Tetralogy of Fallot Tricuspid Atresia Types 1. Normally related great arteries (69%) With small VSD and PS (most common). Intact septum with pulmonary atresia Large VSD without PS 2. D-transposition of great arteries (28%) 3. L-transposition of great arteries (4%) Tricuspid Atresia • Incidence: • Age at presentation • Clinical – No obstruction pulmonary blood flow – Obstruction pulmonary blood flow • Rare • Infancy, depending on pulmonary blood flow • Congestive heart failure Similar to VSD Cyanosis • Variable More intense cyanosis as ductus closes Tricuspid Atresia • Auscultation: • Radiology: Systolic murmur with single S2 Variable Decreased pulmonary vasculature Treatment Tricuspid Atresia 1. PGE1 to keep ductus open 2. Balloon septostomy if no VSD 3. Surgical a. Palliation systemic-pulmonary shunt (PS) pulmonary artery banding (large VSD) b. Corrective Fontan Cyanotic CHD with Increased Pulmonary Blood Flow 1. Truncus Arteriosus 2. Transposition of the Great Arteries 3. Total Anomalous Pulmonary Venous Return Truncus Arteriosus • Incidence • Age at presentation • Clinical • • • • • Rare Neonatal Cyanosis Signs of CHF Wide pule pressure and bounding arterial pulses • Harsh systolic murmur • Auscultation • Pulmonary vasculature • Increased • BVH or RVH • EKG Truncus Arteriosus • Associations • Treatment • Right sided aortic arch • Thymic aplasia - DiGeorge Syndrome • Medical • Pulmonary artery bending • Rastelli’s operation Truncus Arteriosus Transposition of the Great Vessels D-type D-transposition, complete transposition, most common form -Aorta arises from the right ventricle. -Pulmonary artery arises from the left ventricle. -PDA is the only connection between systemic and pulmonary circulations, although VSD in 40%. Transposition of the Great Vessels L-type L-transposition, also called corrected transposition -Both ventricles and great vessels are transposed D-TGA • Incidence • • • • • • Age presentation • Clinical • • Auscultation • Radiology • • • EKG 8% of all CHD Male:female 2:1 Newborn, when ductus closes Cyanosis within 1st 48 hrs if no VSD CHF when large left to right shunts Loud single S2, no murmur Egg-on-a-string heart Increased pulmonary vasculature, depending on size shunt • RVH Treatment for D-TGA 1. Prostaglandin E 2. Surgical a. Atrial septostomy if no VSD (Rashkind, Blalock - Hanlon etc.) b. Anatomical correction (Jatene’s operation) TGA TAPVR types 1. Supracardiac emptying in the left vertical vein (most common type 80-90%) which subsequently drains into the SVC 2. Cardiac emptying into the coronary sinus or right atrium 3.Infradiaphragmatic emptying into vertical vein that descends through diaphragm into portal vein and or IVC TAPVR • Incidence • Age at presentation • Clinical findings • EKG • Radiology • 2% • Newborn • Rapid cyanosis in the infradiaphragmatic type • Non-obstructive similar to ASD plus mild cyanosis • RVH • “Snowman” configuration • Diffuse reticular opacities • Looks like HMD without air bronchograms! TAPVR • Associations • Treatment • Polysplenia • Asplenia (3/4 patients also TAPVR) • Surgical ligation of anomalous vein Total anomalous venous return Acyanotic CHD with Increased Pulmonary Blood Flow (left to right shunt lesions) 1. ASD 2. VSD 3. PDA ASD • Incidence • Types • • • • • • • • • Age presentation • Clinical • • Auscultation • EKG • Treatment • • 10% CHD Ostium secundum (most common) Sinus venosus defect Ostium primum (AV canal) Varies Mostly asymptomatic Slender body build Widely split and fixed S2! + SEM RAD and RVH No SBE coverage needed! Surgery for large shunts ASD VSD • Incidence • • • Types • • • Age presentation • Most common CHD (20%) Coexists with other lesions in 5% Membranous (80%) Muscular (10%) Large - at age 2-3 months with congestive failure • Small to moderate - usually asymptomatic VSD • Clinical • Auscultation • Congestive heart failure if large • Poor weight gain • Systolic thrill with holosystolic murmur at LLSB • Diastolic murmur with large shunts and loud P2 with pulmonary hypertension • Diastolic rumble at apex indicates CHF VSD • EKG • Radiology • Associations • Complications • • • • • 1. normal if small VSD 2. LAE-LVH if moderate 3. LAE-BVH if large 4. RVH-PVOD Increased vascularity with larger shunts and enlargement cardiac size • Holt-Oram syndrome, Down’s, Trisomy 13, Trisomy 18 • Eisenmenger’s Syndrome (shunt reverses to rightleft) Treatment VSD 1. Spontaneous closure of small VSD’s 2. Medical therapy (diuretics, digitalis) 3. Pulmonary artery banding 4. Surgical placement of patch over VSD 5. SBE prophylaxis VSD PDA Clinical Premature infants - Congestive heart failure Term infants - usually asymp murmur Pulm. Vasculature Increased Radiology Dependent on size of shunt Left atrial enlargement often present Massive bulge at left upper mediastinum in large shunts Treatment Premature infants - Indomethacin Ligation and division of the ductus Prostaglandin E infusion maintains ductal patency when needed PDA Acyanotic CHD with Pulmonary Venous Congestion or Normal Blood Flow (Pressure Load) 1. 2. 3. 4. Coarctation Aorta Aortic Stenosis Hypoplastic Left Heart Pulmonary Stenosis Coarctation of the Aorta Incidence: Clinical: Radiology: Associations: Treatment: 5% of CHD Preductal or infantile type presents in young child with CHF and LE pulses Adult type presents with hypertension and difference in arm and leg pulses Rib notching - starts age 6-8 Often isolated Turner’s, NF, William’s, Sturge-Weber Primary repair Prostaglandin E to infants Rib notching Aortic Stenosis Clinical: Pulm. Vasc.: Associations: Treatment: Most asymptomatic Angina Syncope - may be fatal Normal Williams’ Syndrome Medical Surgical No high impact sports Hypoplastic Left Heart Incidence: Age at present.: Clinical: Pulm. Vasc.: Radiology: Treatment: 8% of all CHD, most common cause for early cardiac death Immediately at birth or first weeks 1st presentation is usually not cyanosis, but signs of shock Increased Large cardiac silhouette Prostaglandin E Norwood procedure (high mortality) Mitral Valve Prolapse Facts More common in girls May be inherited as autosomal dominant trait with variable expression Common in Marfan’s Dominant signs are ausculatory; late systolic apical murmur preceded by a click PVC’s may be a complication Non progressive in children Endocarditis prophylaxis indicated only in substantiated cases, usually those with mitral insufficiencies Blalock-Taussig shunt. The subclavian artery is transected and anastomosed in a end-to-side fashion to the ipsilateral pulmonary artery. Usually the subclavian artery opposite to the arch is used. The Modified Blalock-Taussig shunt now uses a Goretex graft (green) to connect the subclavian artery to the pulmonary artery. This preserves the subclavian artery. Potts shunt is where a side-to-side anastomosis is made between the descending aorta and the pulmonary artery. The Waterston-Cooley shunt is similar to the Potts shunt. A side to side anastomosis or window is created between the pulmonary artery and the ascending aorta. The difference is that it is the ascending aorta (Waterston-Cooley) rather than the descending aorta which is anastomosed to the pulmonary artery (Potts). Pearls • Bounding pulses; think PDA or AV fistula. • Widely fixed split second heart tone; think ASD. • No pre- and postductal saturation differences – when there is total mixing of deoxygenated venous blood with oxygenated pulmonary blood in the heart; such as -total anomalous pulmonary venous return -truncus arteriosus Pearls • Pre- and post-ductal saturation differences – post-ductal saturation is higher in TGA – all other congenital heart anomalies without total mixing in the heart have a lower postductal saturation