LVAD - Silver Cross Emergency Medical Services System
advertisement

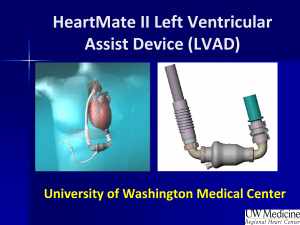
Silver Cross EMSS March 2013 EMD CE LVAD Anatomy of the Heart • The heart can be thought of as 2 pumps in one • The right atrium and ventricle is a low pressure pump because it only has to pump blood to the lungs for oxygenation • The left atrium and ventricle is a high pressure pump because it has to pump all of the oxygenated blood from the lungs to the rest of the body • A VAD or Ventricular Assist Device can assist the Left Ventricle, Right Ventricle or both ventricles in pumping blood when the ventricles need help The Heart Low pressure pump High pressure pump Before VADs • In the old days, when someone needed a heart transplant, they were often stuck in the hospital. • They were hooked up to large heart pumps. • Their life-spans were very short. • They often died before a new heart became available. A Ventricular assist device, or VAD, is a mechanical circulatory device that is used to partially or completely replace the function of a failing heart. Some VADs are intended for short term use, typically for patients recovering from heart attacks or heart surgery, while others are intended for long term use (months to years and in some cases for life), typically for patients suffering from congestive heart failure. VADs need to be clearly distinguished from artificial hearts, which are designed to completely take over cardiac function and generally require the removal of the patient's heart. The unit below is for in-hospital use. Ventricular Assist Device or VAD: Is an artificial device implanted in the chest to assist a damaged or weakened heart. An LVAD is a LEFT Ventricular Assist Device Sometimes also referred to as an LVAS (Left Ventricular Assist System). There are Right Ventricular (RVAD) and Bi-ventricular (BiVAD) devices too, but the Left is the most common. Due to its design, basic equipment will not detect a blood pressure or pulse even when the unit is working and the patient is alive and talking. Special Dopler equipment is necessary and 60–90 mmHg is the acceptable range. VADs are designed to assist either the right (RVAD) or left (LVAD) ventricle, or both at once (BiVAD). Which of these types is used depends primarily on the underlying heart disease and the pulmonary arterial resistance that determines the load on the right ventricle. Why the LVAD • The LVAD is, in effect, a portable heart pump. •Connected to the left ventricle, which does the major work of pumping blood through the body. •Worn with chest harness and fanny pack. •So advanced, patients can wear them for years if necessary •Until a donor heart is available or as an end treatment A short video • One of the most commonly used LVADs in the area is the Thoratec HeartMate II. • The Thoratec company has released a training film for EMS responders. • Click here ↓ for the LVAD video from Thoratec: http://www.thoratec.com/videos/pc-considering-vad.aspx?id=pc_hm_xveLvasPatEduProg • There are other brands on the market. – If you have patients with LVADs in your community, confirm with them which models they carry and how EMS instructions may differ. Popularity of LVAD • So advanced that many patients now use them not while waiting for a heart, but as an end-treatment. • Research suggests releasing patients home with LVAD contributes to positive outcomes. • Studies show depression and co-morbidities normally linked to heart surgery and transplants are much lower with the LVAD. VP Dick Chaney has one DO NOT PERFORM CPR IF PATIENT HAS A Ventricular Assist Device While the patient may appear unconscious and not seem to have a pulse the pump is still circulating blood and can keeping the patient in a viable condition. Pressure on the chest (chest compressions) may cause the tubing to detach from the heart or damage the device itself causing severe internal blood loss and the patient could bleed to death. Unless the patient is in obvious cardiac arrest and the pump isn’t working, then use the assistance of the VAD coordinator or Medical Control to figure this out before any compressions are performed. Special Care Considerations • Let patient and/or caregiver lead/advise. They will be the experts. • Defibrillation/cardioversion may be performed as normal, but pads should not go over the device that is under the patient’s skin. • Advise EMS these patients typically have an extremely reduced pulse rate or none at all. • Advise EMS to be careful no cords are cut, kinked, or twisted. • Advise EMS to take the patient’s emergency travel bag when leaving the scene. It has an extra controller, batteries and the VAD coordinator’s emergency contact number. Transport Considerations • Use of aeromedical transport may be considered, depending on the length of transport and the patient's condition. Every attempt should be made to contact the patient's doctor or emergency contact person to identify the nearest implant or transplant center. Patients should then be transported to that identified center by the most appropriate means of transportation. An example of a call - A 911 call is made. A male patient collapses and seems too sluggish to move. An Ambulance is immediately dispatched to the location. The paramedics arrive and finds the patient sitting on the floor with his wife by his side. The male is conscious and answers the questions the paramedics ask. He states he became dizzy and passed out. The patient continues to say that he has a Left Ventricular Assist Device (LVAD) implanted and grafted to his heart. The LVAD helps pump oxygen-enriched blood that his damaged heart can not do. The male patient also claims that due to the design of the LVAD, basic equipment WILL NOT detect his Blood Pressure nor Pulse. Another call example • On arrival at the scene, Ambulance 1 finds First Responders are preparing to start CPR. In a tense and somewhat confused voice, the Officer says, “He has no pulse, but his wife won’t let us do CPR. What should we do?” An EMS member from Ambulance 1 immediately feels for his pulses and finds none. Then he hears the man’s wife repeatedly saying, “He has a VAD.” The medic sees a cord coming out of the patient’s abdomen, connected to a small electronic pack attached to the patient’s belt. His ECG shows ventricular tachycardia (v tach), and his wife hands you a card and says, “Call this special ventricular assist device consultation line; they will tell you what to do.” • In this case, the patient is lucky his wife is present to stop the responders from starting compressions and causing further harm. LVAD wrap-up • LVAD patients usually contact local fire departments and ambulance services to offer training. • If unsure how to treat an LVAD patient on scene, contact medical control and the patient’s hospital liaison (VAD Coordinator) as soon as possible. • Again, remember this CME only covered the most common LVAD in the Chicago area. – Other models may require different procedures for CPR, for example hand-pumps, etc. EMD Instructions The EMS System has no protocol for LVAD patients and there’s nothing in the EMDPRS to address these patients. You can refer the caller to the patient’s doctor or LVAD coordinator for further instructions and send an ambulance. If callers are asking for specific help (i.e. CPR, bleeding control, etc.) refer to the proper protocol. Advise EMS that there’s an LVAD patient and pass along any other pertinent information to responders. SUGGESTION Work with your fire departments and community to identify “Special Needs” patients, before they call 9-1-1. Keep a database or CAD notes on these patients, with considerations for special situations. Additional Info http://www.mylvad.com/ems Visit this web site for additional information on EMS treatment of LVAD patients and a complete guide of the various models. YouTube has many inspirational stories and training videos on LVAD patients also.