Patient Case Study
advertisement

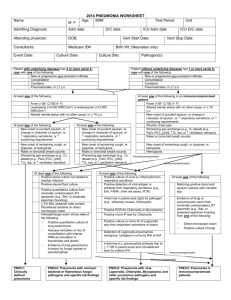
Deserae Vickery MS EBP CASE STUDY 02/01/15 Patient c/o fever, chills, nausea, abdominal pain, and vomiting (green) for the past 5 hours escalating to the point of cramping and inability to stand or walk. Patient called EMS. Upon admit to the ER vitals : Temp 95.3, P 81, BP 79/63, RR 12, 96% RA. INR > 17.2 and PT > 148.7 RT poor management of coumadin at home. Given 3 L NS bolus. DX: Toxic megacolon perforation septic shock requiring emergent subcolectomy and ileocolostomy. General patient information: Age: 70 yr Sex: F Height: 5’5” Weight: 61.5 kg (135.3 lbs.) Review of General Health : A-fib (Past), HT (Past), Thrombocytopenia(Current), Bipolar (Current), Pneumonia (Past), GERD (Current), Smoker (Current), Breast implants (80’s), hysterectomy (70s), Lap removal of ovaries/tubes 07/19/13. Potential medical/psycho/social/cultural barriers to care: Acute trauma. Emergent subcolectomy and ileocolostomy. Elderly. Patient lives alone. Never married. No children. Diagnosis of Bipolar. Patient is affiliated with the Baptist faith. Previous career as a super model. Current Pathology: Toxic Megacolon Marked enlargement of the colon, esp. the transverse colon. Manifestations include tachycardia, fever, leukocytosis, abdominal tenderness, palpable abdominal mass, confusion, cramping, and change in number of bowel movements. (Venes, & Taber, 2009, pg. 1428) Perforation Abdominal crisis in which a hole forms in the GI tract resulting in the release of intestinal fluids into the peritoneum encompassing abdominal organs. Requiring surgical treatment ((Venes, & Taber, 2009, pg. 1742) Septic Shock Presence of pathogens and their toxins in the blood initiate a systemic inflammatory response and vascular damage. (Venes, & Taber, 2009, pg. 2119) Related Labs: (Kee, 2014) Hct 34.5 LOW NML 0.36 – 0.46 Hct is the volume of packed RBCs. Low Hct is found frequently in anemia and is influenced byantibiotics. ( pg 228) RT Patient: prescribed antibiotics and is postop (blood loss) Hgb 12.0 LOW NML 12-15 Hgb is a protein substance founds in RBCs. Gives blood its red color and is composed of Fe, which is an O2 carrier. Low Hgb is found in anemias. Can be influenced by excess IV fluids and antibiotics. RT patient: prescribed antibiotics and is postop (blood loss) WBC 3.9 LOW NML 4,500 – 10,000 WBC’s are used to fight infection RT patient: fighting infection and stores are becoming exhausted RBC 2.74 LOW NML RT decreased Hct 4.0 – 6.0 Platelet Ct. 66 LOW NML 150,000-400,000 Low levels indicate anemia and bleeding (pg 339) RT Patient: Postop (loss of blood), and has excessively used Coumadin BUN 53 HIGH NML 5 – 25 Urea is a formed end product and excreted by the kidneys. High BUN could be an indication of dehydration, renal insufficiency/failure RT shock/sepsis, GI bleeding. (Page 90) RT Patient: multi-organ failure RT shock and sepsis Creatinine 2.30 HIGH NML 0.5 – 1.5 Creatinine is a by product of muscle catabolism and broken down by muscle creatine phosphate. Creatinine is considered a more sensitive and specific indicator of renal disease than BUN. It rises later and is not influenced by diet or fluid intake. High creatinine is indicative of acute and chronic renal failure, prolonged shock ( pg 154) RT: Patient: prolonged shock AEB decreased BP Albumin 2 LOW NML 3.5 – 5.0 Low levels may indicate cirrhosis of the liver, acute liver failure, severe burns, severe malnutrition, preeclampsia, renal disorders, certain malignancies, ulcerative colitis, prolonged immobilizations, protein loosing enteropathies, or malabsorption (Pg 17) RT Patient: malnourished and can absorb nutrients ALT 158 HIGH NML 10-35 Alanine aminotransferase is an enzyme found primarily in liver cells and is effective for diagnosing hepatocellular destruction. High levels are seen in liver necrosis and acute hepatitis (page 15) RT patient: multi-organ failure AST 205 HIGH NML 8-35 Aspartate aminotransferase is an enzyme found mainly in the heart muscle and liver. The concentration is normally low in blood except for when there is cellular injury. High levels are found following an acute MI and liver damage (page 73). RT Patient: multi-organ failure ABG’s PH 7.38 NML 7.35 – 7.45 PaCO2 38 NML 35 – 45 HCO3 24.1 NML 22 - 28 Mode: AC Rate: 14 TV: 600 mL Settings FiO2: 50 % Peep: Medications (Vallerand, Sanoski,&Deglin, 2013) Metronidazole (Flagyl) in NaCl 500 mg=100ml q8hrs (pg 856) Indications: (IV) perioperative prophylactic agent in colorectal surgery Nursing Implications: Assess for infection throughout therapy, monitor neurologic status, monitor I&O esp. pts. w/ Na restriction (each 500 mg contains 14 mEq of Na), Assess for rash periodically – May cause Stevens Johnson syndrome, D/C if rash accompanied w/ fever, general malaise, fatigue, muscle/joint aches, blisters, oral lesions,conjunctivitis, hepatitis, and or eosinopilia Pantoprazole (Protonix) (pg 986) Indications: GERD 40 mg = 100 ml q6hrs Nursing Implications: Assess pt. periodically for epigastric or abdominal pain and for frank or occult blood in stool, emesis, or gastric aspirate. May cause abnormal LFT (^ AST, ALT, alkaline phosphatase, and bilirubin). May cause hyperMg. Piperacillian/tazobactam (Zosyn) 3.375 gm=100 ml q6hrs (pg 1030) Indications: Appendicitis and peritonitis, skin infections, gynecologic infections, Community acquired infections and nosocomial infections. Nursing Implications: Assess pt. for infection, contraindicated in pts. w/ a hypersensitivity to penicillians, Observe for s/s of anaphylaxis (rash, pruritis, laryngeal edema,wheezing). Monitor bowel function ( report D, abd cramping, F, and bloody stools – may be signs of pseudomembraneous colitis) Nursing Assessment: VS: HR 137, P 142, BP 99/55, and RR 16. NEURO. Intubated. Doesn’t open the eyes. No motor or verbal response to a central stimulus. PERRL. Sluggish response. INTEGUMENT: Skin mostly warm and dry with cooler extremities. Generalized Bruising. Various stages of healing. Poor anticoagulant management at home. Generalized mild jaundice. Right triple lumen subclavian central line and right femoral arterial central line. No site redness. Dressings dry and intact. Sub colectomy abdominal incision. Edges well approximated. Mild redness. Minimal serous drainage. Dressing dry and intact. Stoma site mildly swollen; otherwise, beefy red. Illeostomy drainage is sanguineous without presence of fecal matter. Closed endotracheal tube. Suctioned accordingly. RESP: Coarse bronchi heard upon auscultation throughout all lobes. Suctioned accordingly. Mild improvement noted. CV: S1, S2 auscultated. Tachycardic rate. Amiodarone admin as ordered. Radialpulse 3+ bilat. CRT < 3 sec. Pedal pulse 2+ bilat. MS: Intubated. Flacid UE bilat and LE bilat. No motor response to PROM. GI: One day postop. Absent bowel sounds x 4. Abdomen soft. Mildly swollen. Last bowel movement unknown. GU: Foley catheter present. Urine is light yellow without sediment. 3 Nursing Dx’s Risk for infection RT secondary complications of mechanical ventilation, multiple invasive lines, and ileocolostomy Ineffective airway clearance RT inability to clear secretions AEB presence of endotracheal tube , and coarse ronchi heard upon auscultation Risk for situational low self esteem RT lack of support system and recent trauma requiring hospitalization, subcolectomy, and permanent ileostomy Priority Nursing Dx : Risk for infection RT secondary complications of mechanical ventilation, multiple invasive lines, and ileocolostomy (ASPECT: Oral Care of the ventilated patient) ARTICLE: Intermittent subglottic secretion drainage on ventilator-associated pneumonia: A clinical trial (Safdari,Yazdannik, & Abbasi, 2014) DESIGN: Four general ICUs of selected educational hospitals in Isfahan, Iran with medical, surgical, and trauma patients between November 2012 and February 2013. Randomized control trial to determine the incidence of early-onset VAP (Ventricular Associated Pneumonia) among patients who receive SSD (Subglottic Secretion Drainage) compared to patients who receive endotracheal suctioning without SSD. Frequency : suctioning every 3 hours POPULATION: 408 patients were admitted in the participating ICUs who were 18 – 60 years of age, intubated with a cuffed polyvinyl chloride endotracheal tube (PVC ETT) and likely required mechanical ventilation for at least 48 hrs. Exclusion criteria and unforeseen events limited the analysis to 76 patients 38 patients received SSD via the inspiratory pause method (SSD group) 38 patients received endotracheal suctioning without SSD (Control group) Exclusion Criteria: Patients who were admitted to the ICUs with tracheostomy Patients whose mechanical ventilation was normally shorter than 48 h (psychotropic drug overdose, etc.) Patients who were likely to die in the next 48 h (those who were admitted after cardiac arrest, etc.) Patients who were admitted to these units for treatment of pneumonia Others with lung complications like fibrosis or cancer METHOD: SSD via the inspiratory pause method or endotracheal suctioning without SSD every 3 hours. Oropharyngeal suctioning was performed prior to each suctioning. The Inspiratory Pause Method : Performed using the inspiratory pause or inspiratory hold keys on the ventilator, an inspiratory hold was applied. Inspiration was held in the patient for 3 sec only until the cuff of the ETT was depleted. Air flow rising past the deflated cuff drove the subglottic secretions toward the oropharynx .Secretions were removed with repeated oropharyngeal suctioning by a nurse specialist in critical care. The cuff pressure was maintained between 20 and 30 mm H2O. RESULTS: Within 5 days of mechanical ventilation, 28 patients developed pneumonia: 10 (26.3%) in the SSD group and 18 (47.4%) in the control group. CONCLUSION: Secretions contaminated with oral, nasal, and gastric bacteria accumulate in the subglottic space, above the endotracheal tube cuff. If these secretions are aspirated into lower airways, the intubated patient will be susceptible to ventilator-associated pneumonia (VAP) Endotracheal suctioning is effective at reducing bacterial colonization of the lower airways; however, subglottic secretion drainage is more effective LIMITATIONS: Small sample size Family member gave permission ARTICLE: The effect of different oral hygiene treatments on the occurrence of ventilator associated pneumonia (VAP) in ventilated patients (Lev, Aied, & Arshed 2015). DESIGN: General ICU in the Emek Medical Center, Israel between August 2007 and October 2009. Prospective, controlled study to determine the incidence of VAP in ventilated Patients who received a comprehensive oral hygiene regimen compared to a conventional treatment regimen POPULATION: Upon admission to the ICU, ventilated patients were alternately allocated to either the study group (n=45) or the control group (n=45). Excluded: patients who were younger than 18 years, patients with a clinical diagnosis of pneumonia at the time of intubation, immunosuppressed patients, pregnant women, and burn patients METHOD: The oral care protocol was implemented 3x/ day Patients in the study group received a comprehensive oral hygiene treatment regimen that involved a soft-bristle suction toothbrush w/ sodium bicarbonate (to mechanically clean, refresh, and deodorize the oral cavity), rinsing with an antiseptic solution (1.5% hydrogen peroxide) and applying a mouth moisturizer containing vitamin E to promote the healing of lesions Patients in the control group received a more conventional treatment that included cleaning with a sponge and rinsing with an antiseptic solution (0.2% chlorhexidine gluconate.) RESULTS 8.9% of the study group (comprehensive) developed VAP compared with 33.3% of the control group (conventional). Patients in the study group spent a mean of 11.09 days in the ICU compared to those in the control group (14.98 days). The mean number of days on a ventilator was 8.39 in the study group compared to 12.69 days in the control group. The mean number of days of hospitalization was 25.38 in the study group compared to 31.71 days in the control group . The study group patients had a mean of 7.2 treatment days with antibiotics compared with 9.7 days in the control group CONCLUSION In patients who are ventilated, a comprehensive oral hygiene treatment regimen that includes tooth brushing, suctioning, rinsing with an antiseptic, and application of a moisturizer is more effective in preventing VAP than more conventional protocols. Comprehensive oral hygiene decreases length of hospitalization, antibiotic use, and days on mechanical ventilation LIMITATIONS Patients were alternately allocated to either the study or control group. The unblinded nature of the study has the potential to introduce bias. Patients received varying antibiotic regimens, which could have affected VAP rates. Providers of oral care could have varying skill in the application of the protocol, introducing the possibility of operator bias. CARE PLAN: Risk for infection RT secondary complications of mechanical ventilation, multiple invasive lines, and ileocolostomy Patient goals/outcomes Patient will maintain a patent airway remaining clear of secretions for the entire shift. Patient will remain free of respiratory infection for length of hospitalization. Nursing Intervention Nurse will perform subglottic suctioning q 3 hrs to maintain a patent airway and reduce bacterial colonization Rationale Secretions contaminated with oral, nasal, and gastric bacteria accumulate in the subglottic space, above the endotracheal tube cuff. If these secretions are aspirated into lower airways, the intubated patient will be susceptible to ventilator-associated pneumonia (VAP) (Safdari,Yazdannik, & Abbasi, 2014). Patient goals/outcomes Patient will remain free from respiratory infection for length of hospital stay Nursing Interventions Nurse will perform oral care 2 x while on shift using a suction toothbrush Rationale Mouth-related risk factors for infection include the formation of bacterial colonies in the mouth, the accumulation of pathogenic bacteria on the surface of the teeth, development of plaque, and aspiration of secretions from the oral cavity (Lev, Aied, & Arshed 2015). REFERENCES Kee, J. L. (2014). Laboratory and diagnostic tests with nursing implications (9th ed.). Upper Saddle River, NJ: Pearson. Lev, A., Aied, A. S., & Arshed, S. (2015). The effect of different oral hygiene treatments on the occurrence of ventilator associated pneumonia (VAP) in ventilated patients. Journal of Infection Prevention, 16(2), 76-81. Safdari, R., Yazdannik, A., & Abbasi, S. (2014). Effect of intermittent subglottic secretion drainage on ventilator-associated pneumonia: A clinical trial. Iranian Journal of Nursing & Midwifery Research, 19(4), 376-380. Vallerand, A. H., Sanoski, C. A., & Deglin, J. H. (2013). Davis's drug guide for nurses(13th ed.). PA: F.A Davis. Venes, D., & Taber, C. W. (2009). Taber's cyclopedic medical dictionary (21st ed.). Philadelphia, PA: F. A. Davis Co.