Plastic Surgery Techniques in Podiatry
advertisement

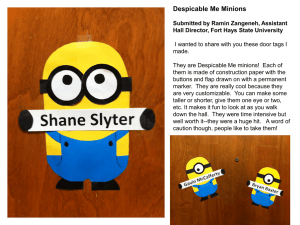
Dan Preece DPM, PGY-1 The Best Plastic Surgery? Wound Prevention: Puncture vs Crush: skin hooks and toothed pick ups instead of flat. Tension: think undermining, blanching is bad, more suture lines = crossing wound less force per suture Vasculature: check perfusion, adequate vasc supply?, vasc consult if necessary prior to intervention. Protection: trust pt to remain NWB?, offload potential wounds. Soft Tissue Envelope: fractures etc, this envelope needs protection, key to healing. 1. Levin, S. Nunley, J. Soft Tissue Reconstruction for the Foot and Ankle. Foot and Ankle Surgery. Ch 34, pg 1869-90. Tissue Planes: The soft tissue envelope is composed of several tissue layers, each with a specific function and its own vascular supply. Skin, which consists of epidermis and dermis. Subcutaneous tissue, is less vascular, provides a cushion around bony prominences. Fascia surrounds muscle compartments and neurovascular canals, tendons, ligaments, contains a rich vascular plexus. Muscles are richly vascularized, can be manipulated as transposition flaps, island pedicle flaps, and free tissue transplantations (free flaps). Periosteum surrounds all long bones and is vital to the response of bone to injury and repair. Can be used as a free flap to augment conventional methods of bone grafting. Skin Layers: 2. http://upload.wikimedia.org/wikipedia/commons/3/34/Skin.jpg Deep Fascia: 3. http://www.somaxsports.com/ images/analysis/fascia_of_thi gh.jpg 4. http://www.cals.ncsu.edu/course/zo250/bone-structure-2.jpg Wound Preparation: Irreversibly damaged or nonviable tissues need to be replaced. Marginally viable tissue left behind can subsequently desiccate, infarct, and become infected, adding further delay in healing. Bone debridement: until “paprika sign” is found (punctate bleeding). Options: Ultrasound, versajet, pulse lavage, sharp debridement. 5. http://wound.smith-nephew.com/ca_en/Standard.asp?NodeId=3169 Skin Grafts Site Candidates: Full thickness wounds. Full thickness wounds: if allowed to heal by primary intention will lack dermal appendages anchoring epidermis with dermis. Wounds experience contraction and reepithelialization from the wound periphery, leaving central tissue that is relatively unstable in terms of long-term durability. 6.http://www.nlm.nih.gov/medlineplus/ency/images/ency/fullsize/19083.jpg Skin Graft Keys: Thickness: Sweat glands (both apocrine and eccrine): Split thickness: 0.008-0.02 in, less durable. Full thickness: >0.02 in, or the full thickness of dermis/epidermis. More stable/durable. Grafts/flapswill temporarily lose nervous control in grafts, newly grafted skin may be dry, requiring moisturizing with common over-the-counter preparations. Wound bed: Bad: Exposed bone, tendon, nerve and cartilage, necrotic tissue, and devascularized fat. Good: muscle, periosteum, perichondrium, fascia, healthy fat, and epitenon will all accept skin grafts, any highly fascular surface. 7. Malay, S. Plastic Surgery Techniques. The PI Manual. Ch 6, Page 126. Flaps: Rotation, Transitional, Advancement Flaps: May include muscle, skin, and fascia, or a combination. Can add much-needed vascularized tissue Obliterate dead space Close the wound without tension May be limited by location and donor site options. Rotational Flap Flap Types: Advancement Flap Transposition Flap 16. http://emedicine.medscape.com/article/1284569-overview V-Y Advancement Flap: BCC excision V-Y Advancement Flap: Undermine deeply to preserve vascular tissue and increase distance allowed to move flap. V-Y Advancement Flap: Rotational Flap: BCC Excision Rotational Flap: Rotational Flap: Free Flaps Compound types: Fasciocutaneous, musculocutaneous, bone with or without other tissues and vascular supply intact (example target: AVN of talus). Require microvascular surgical techniques. Muscular Flap Classification: Type 1: one vascular pedicle (extensor digitorum brevis, tensor fascia lata) Type 2: dominant pedicle and minor pedicles (abductor hallucis gracilis) Type 3: two dominant pedicles (rectus abdominis, serratus anterior) Type 4: segmental vascular pedicles (none) Type 5: one dominant and secondary vascular pedicles (latissimus dorsi, pectoralis major, pectoralis minor) 8. http://emedicine.medscape.com/article/1284776-overview Muscle Flaps Examples: Flexor Digitorum Brevis: used in heel deficit reconstruction. 15. Malay, S. Plastic Surgery Techniques. The PI Manual. Chap 6, pg 131. •PT Fasciocutaneous Flaps: -Designed on the medial aspect of the leg from the knee to the medial malleolus. -Based on septocutaneous perforators of the posterior tibial artery. The pedicle is 2-4 cm long. -It is used for coverage of defects of the middle and lower third of the leg and foot can include the saphenous nerve for sensory innervation Dorsalis Pedis flap: based on the dorsal skin of the medial two thirds of the foot from the ankle to the toes. Blood supply is from the septocutaneous perforators of the dorsalis pedis artery and first dorsal metatarsal artery. Its pedicle length is 6-10 cm. This flap can be used for defects around the ankle, foot, and lower leg, and it is often used as a free flap. Lateral Tarsal Artery Flap (free flap), shows How flaps in this region can be developed 9. http://emedicine.medscape.com/article/1284631-overview 10. http://www.cmj.org/periodical/images/200909/200991516139475.jpg Medial plantar artery flap: Located on the instep of the foot and based on the medial plantar artery. The pedicle is 12 cm long and has a diameter of 1.5 mm. Use this flap for coverage of plantar foot and ankle defects. Sural artery flap: Based on the sural artery direct cutaneous branch of the popliteal artery. The pedicle is 3 cm long and has a diameter of 1.4 mm. It is located between the popliteal fossa and the midposterior leg between the medial and lateral heads of the gastrocnemius muscle. The flap can measure 15 x 6 cm and may include the sural nerve as a neurosensory flap. Use this flap for wounds around the knee and upper leg. Sural fascioneurocutaneous flap: Chronic DM foot ulcer. 11. http://www.owm.com/files/owm/imagecache/normal/files/photo s/owm_0604_f2i1b.gif Sural Fasciocutaneous Flap: 24. Menke, C. Reverse Sural Fasciocutaneous Flap. PI Update 2010. Ch 21, Pg 111-114. Sural Fasciocutaneous Flap: Delay Phenomenom: Once flap has been created it can be transferred immediately or transfer can be delayed. Delay will result in increased blood flow to the flap and increased flap survivability. 23. Ghali S, et al. A modified technique for transposition of the reverse sural artery flap. Plastic Reconstruction Surgery 2006;117:2488-92. •A meta-analysis of 50 papers that report the use of the unmodified distally based sural flap was performed. •587 of 720 flaps (82%) were reported to heal without necrosis or any other flap-related complications. •Complete flap necrosis was reported as a complication in only 24 of 720 flaps (3.3%), •Partial or marginal flap necrosis was reported in 76 of 720 flaps (11%). •Other flap-related complications, such as venous congestion, edema, infection, and recurrent osteomyelitis, were reported in 33 of 720 flaps (4.6%). •18% experienced significant complications overall. 12. Donski PK, Fogdestam I: Distally based fased fasciocutaneous flap from the sural region: A preliminary report. Scand J Plast Reconstr Surg 17:191-196, 1983. Flap Failure: Acute complications occur usually in the first 48 hours and include: venous thrombosis arterial thrombosis hematoma, and hemorrhage excessive flap edema. Flap Arterial Insufficiency: Arterial insufficiency can be recognized by: decreased capillary refill pallor, reduced temperature the absence of bleeding after pinprick Causes: -arterial spasm, -vessel plaque, -torsion of the pedicle, -pressure on the flap, -technical error with injury to the pedicle, -a flap that is too large for its blood supply, -small vessel disease (due to smoking or diabetes). Flap Viability Monitoring: pH monitoring and transcutaneous oxygen tension (PO2) can aid in early detection of flap ischemia. Doppler ultrasound. Laser Doppler. Surface temperature monitoring. 17. 18. 19. 20. 21. 22. Serafin D, Lesesne CB, Mullen RY, Georgiade NG. Transcutaneous PO2 monitoring for assessing viability and predicting survival of skin flaps: experimental and clinical correlations. J Microsurg. Mar 1981;2(3):165-78. Hirigoyen MB, Blackwell KE, Zhang WX, Silver L, Weinberg H, Urken ML. Continuous tissue oxygen tension measurement as a monitor of free-flap viability. Plast Reconstr Surg. Mar 1997;99(3):763-73. Levinsohn DG, Gordon L, Sessler DI. Comparison of four objective methods of monitoring digital venous congestion. J Hand Surg [Am]. Nov 1991;16(6):1056-62. Solomon GA, Yaremchuk MJ, Manson PN. Doppler ultrasound surface monitoring of both arterial and venous flow in clinical free tissue transfers. J Reconstr Microsurg. Oct 1986;3(1):39-41. ones BM, Mayou BJ. The Laser Doppler flowmeter for microvascular monitoring: a preliminary report. Br J Plast Surg. Apr 1982;35(2):147-9. Sloan GM, Sasaki GH. Noninvasive monitoring of tissue viability. Clin Plast Surg. Apr 1985;12(2):185-95. Arterial Compromise Management: 13. Pharmacologic intervention at the time of exploration includes vasodilators, calcium channel blockers, and systemic anticoagulants. If the above measures fail, anastomosis should be redone to rule out intraarterial thrombus. Pang CY, Forrest CR, Morris SF: Pharmacological augmentation of skin flap viability: A hypothesis to mimic the surgical delay phenomenon or a wishful thought. Ann Plast Surg 22:293-306, 1989. Venous Outflow Obstruction: Signs: violaceous color brisk capillary refill normal or elevated temperature and production of dark blood after pinprick. Venous insufficiency can occur due to: torsion of the pedicle, flap edema, hematoma, or tight closure of the tissue over the pedicle. The venous outflow obstruction can result in: extravasation of red blood cells, endothelial breakdown, microvascular collapse, thrombosis in the microcirculation, and flap death. Venous Congestion: Clinical observation and the monitoring of the patient (such as with laser Doppler) should alert the surgeon. Conservative treatment may include drainage of the hematoma at the bedside. Release of a few sutures to decrease pressure. Leeches may be helpful if insufficient venous outflow cannot be established despite a patent venous anastomosis. (The leeches inject a salivary component (hirudin) that inhibits platelet aggregation and the coagulation cascade.) Leech Tx for Venous Congestion or Arterial Compromise of Flaps… 14. Utley DS, Koch RJ, Goode RL: The failing flap in facial plastic and reconstructive surgery: Role of the medicinal leech. Laryngoscope 108:1129-1135, 1998. Bottom Line: Be Prepared… Sources: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. Levin, S. Nunley, J. Soft Tissue Reconstruction for the Foot and Ankle. Foot and Ankle Surgery. Ch 34, pg 1869-90. http://upload.wikimedia.org/wikipedia/commons/3/34/Skin.jpg http://www.somaxsports.com/images/analysis/fascia_of_thigh.jpg http://www.cals.ncsu.edu/course/zo250/bone-structure-2.jpg http://wound.smith-nephew.com/ca_en/Standard.asp?NodeId=3169 http://www.nlm.nih.gov/medlineplus/ency/images/ency/fullsize/19083.jpg Malay, S. Plastic Surgery Techniques. The PI Manual. Ch 6, Page 126. http://emedicine.medscape.com/article/1284776-overview http://emedicine.medscape.com/article/1284631-overview http://www.cmj.org/periodical/images/200909/200991516139475.jpg http://www.o-wm.com/files/owm/imagecache/normal/files/photos/owm_0604_f2i1b.gif Donski PK, Fogdestam I: Distally based fased fasciocutaneous flap from the sural region: A preliminary report. Scand J Plast Reconstr Surg 17:191-196, 1983. Pang CY, Forrest CR, Morris SF: Pharmacological augmentation of skin flap viability: A hypothesis to mimic the surgical delay phenomenon or a wishful thought. Ann Plast Surg 22:293-306, 1989. Utley DS, Koch RJ, Goode RL: The failing flap in facial plastic and reconstructive surgery: Role of the medicinal leech. Laryngoscope 108:1129-1135, 1998. Malay, S. Plastic Surgery Techniques. The PI Manual. Chap 6, pg 131. http://emedicine.medscape.com/article/1284569-overview Serafin D, Lesesne CB, Mullen RY, Georgiade NG. Transcutaneous PO2 monitoring for assessing viability and predicting survival of skin flaps: experimental and clinical correlations. J Microsurg. Mar 1981;2(3):165-78. Hirigoyen MB, Blackwell KE, Zhang WX, Silver L, Weinberg H, Urken ML. Continuous tissue oxygen tension measurement as a monitor of free-flap viability. Plast Reconstr Surg. Mar 1997;99(3):763-73. Levinsohn DG, Gordon L, Sessler DI. Comparison of four objective methods of monitoring digital venous congestion. J Hand Surg [Am]. Nov 1991;16(6):1056-62. Solomon GA, Yaremchuk MJ, Manson PN. Doppler ultrasound surface monitoring of both arterial and venous flow in clinical free tissue transfers. J Reconstr Microsurg. Oct 1986;3(1):39-41. Jones BM, Mayou BJ. The Laser Doppler flowmeter for microvascular monitoring: a preliminary report. Br J Plast Surg. Apr 1982;35(2):147-9. Sloan GM, Sasaki GH. Noninvasive monitoring of tissue viability. Clin Plast Surg. Apr 1985;12(2):185-95. 23.. Ghali S, et al. A modified technique for transposition of the reverse sural artery flap. Plastic Reconstruction Surgery 2006;117:2488-92. 24. Menke, C. Reverse Sural Fasciocutaneous Flap. PI Update 2010. Ch 21, Pg 111-114.