Vasopressin Steroids and Epinephrine in Cardiac Arrest
advertisement

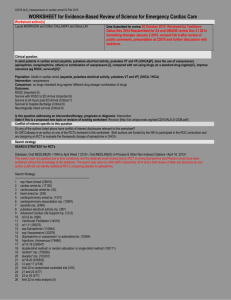
By Greg Gipson 8/30/13 Out-of-hospital ◦ US survival rate 11.4% ◦ King County survival rate 52% In-hospital ◦ ◦ ◦ ◦ Estimated 6.7 per 1000 admissions 200,000 patients/year Neurologic damage Survival to discharge 24.2% Still room for improvement American Heart Association, http://www.heart.org/HEARTORG/, accessed 8/27/13 EMS 2012 Annual Report, available at www.kingcounty.gov/health/ems, accessed 8/27/13 AHA 2010 algorithm ◦ CPR ◦ Shock ◦ Drugs Epi 1mg q3-5min Vasopressin 40 IU Amio 300mg Repeat 150mg ◦ Return of spontaneous circulation (ROSC) American Heart Association, http://www.heart.org/HEARTORG/, accessed 8/27/13 Vasopressin, steroids, and epinephrine and neurologically favorable survival after inhospital cardiac arrest ◦ Previous trial showed benefit RCT, single center, n=100 ↑ROSC, ↑survival to discharge, similar ADEs ◦ Neurologically survival ≠ survival ◦ Further investigate treatment algorithm Published: JAMA - July 2013 Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. Mentzelopoulos S, Zakynthinos S, Tzoufi M, et al. Vasopressin, epinephrine, and corticosteroids for in-hospital cardiac arrest RC, DB, PC, parallel-group, MC ◦ Pharmacists randomized Sept 1, 2008 – Oct 1, 2010 3 Greek tertiary care hospitals N=268 consecutive patients Exclusion ◦ <18 y/o, terminal illness, DNR, exsanguination, arrest before admission, IV steroids, previous enrollment/exclusion Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. Cardiac arrest! Begin CPR (30:2) Intervention q 3 minutes, x 5 times ◦ Tx: Vasopressin 20 IU and epi 1mg ◦ Control: Saline placebo and epi 1mg First cycle ONLY ◦ Tx: Methyprednisolone 40mg IV ◦ Control: Saline placebo Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. No ROSC by 5th cycle ◦ Follow European resuscitation guidelines ◦ Epi 1mg q3-5min ◦ Option: Amio, atropine, magnesium Nolan JP, Deakin CD, Soar J. European resuscitation council. European resuscitation council guidelines for resuscitation 2005: Section 4, Adult advanced life support. Resuscitation. 2005;37(suppl 1):@39-S86 4 hours post resuscitation ◦ Postresuscitation shock? Tx: Hydrocortisone 300 mg/d CI, ≤ 7 days, then taper Unless AMI, then ≤ 3 days Control: Saline infusions Could receive open-label hydrocortisone Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. Primary Secondary ◦ ROSC x ≥20 minutes ◦ Survival to discharge w/ CPC 1 or 2 ◦ ◦ ◦ ◦ Atrial pressure 20 min post ROSC Atrial pressure + ScvO2 (days 1-10) Organ failure free days (days 1-60) Corticosteroid complications Hyperglycemia, infection, PUD, paresis Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. Grenvik A, Safar P. Eds: Brain failure and resuscitation, Churchill Livingstone, New Yortk, 1981; 155-184. Power calculations ◦ N=244 ITT Tested ◦ Normality ◦ Heterogeneity Analysis methods ◦ ◦ ◦ ◦ ◦ Chi2 or Fischer exact T-tests Linear-mixed model Logistic regression Multivariate Cox Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. Figure 1 Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. Comparable baseline characteristics Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. MAP higher on days 1, 2, 4, 5, 10 post resuscitation ScvO2 higher on days 1, 2, 4-10 post resuscitation Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. More organ failure free days and ventilator free days in treatment group Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. Adverse events from corticosteroids ◦ Tx group Used more insulin (p<0.001) No difference in hyperglycemia (>180mg/dL, p=0.88) ◦ No other ADEs reported Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. Epinephrine ◦ Adrenergic agonist Vasoconstriction ↑Cerebral perfusion ↑Coronary perfusion ↑HR, ↑CO ↑Cerebral perfusion ↑Coronary perfusion ↑Myocardial O2 consumption ◦ Effect attenuated in hypoxia and acidosis ◦ T1/2 = 2-3 min ◦ Peak concentration ~90 sec Papastylianou A, Mentzelopoulos S. Current pharmacological advances in the treatment of cardiac arrest. Emergency Medicine International 2012,815857;9. Vasopressin ◦ Vasopressin receptor agonist (V1,2,3) V1 – Vasoconstriction ↑ Cerebral perfusion V2 – Antidiuresis (distal convoluted tubule, medullary collecting duct) V3 – Insulin, ACTH, temp, BP, memory (anterior pituitary, islet cells) ◦ Survivors show low vasopressin levels ◦ T1/2 = 10-35 min ◦ Data shows: Vasopressin = Epi Papastylianou A, Mentzelopoulos S. Current pharmacological advances in the treatment of cardiac arrest. Emergency Medicine International 2012,815857;9. Image from: MCAT Review, http://mcatprep4free.blogspot.com/2011/08/antidiuretic-hormone-adh.html, Accessed 8/28/13 Corticosteroids ◦ Use is controversial ◦ Adrenal dysfunction possible in shock ◦ Not standard of practice for cardiac resuscitation ↑ effect of epinephrine ↑ effect of vasopressin ↑ myocardial function post arrest ◦ Other possibly beneficial effects Anti-inflammatory Increase fluid volume ◦ ADEs Patel G, Balk R. Systemic steroids in severe sepsis and septic shock. American Journal of Respiratory and Critical Care Medicine. 2012;2:133-139 Skyschally A, Haude M, Dorge H, et al. Glucocorticoid treatment prevents progressive myocardial dysfunction resulting from experimental coronary microembloism. Circulation 2004;109(19):2337-2342. Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest. JAMA 2013;310(3):270-279. Image from: http://images.ddccdn.com/drp/images/12/80007201.jpg, Accessed 8/28/13 VSE ◦ ◦ ◦ ◦ ◦ ↑ ROSC ↑ Survival and neurologic outcomes ↑ Hemodynamics ↓ Organ failure ? Corticosteroid complications ↑ Insulin use ↔ Hyperglycemia Can we safely apply these results to a US population? Should we repeat this trial in King County? What will the next AHA ACLS guidelines recommend? ◦ Will they incorporate this data?