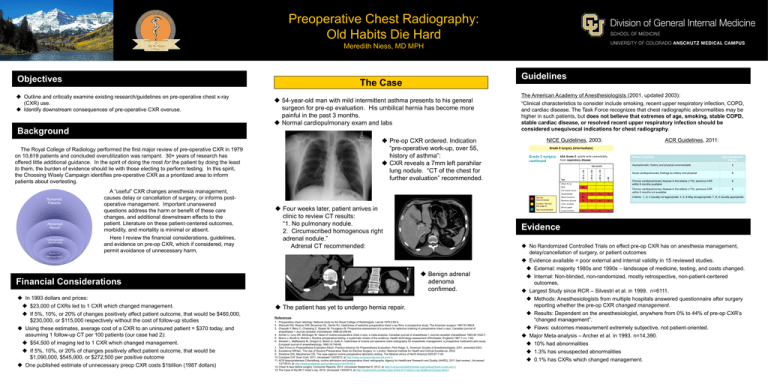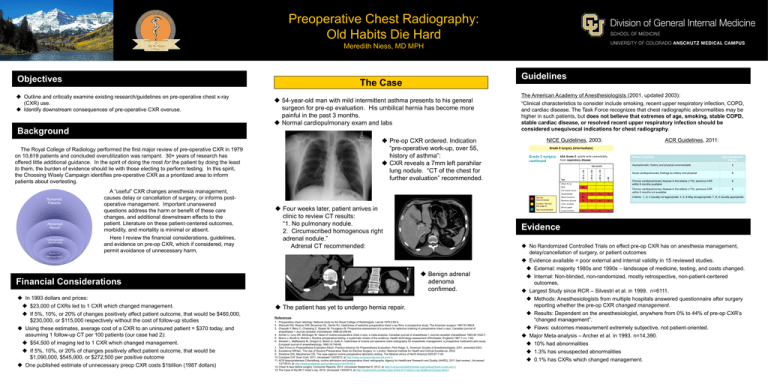
Preoperative Chest Radiography:
Old Habits Die Hard
Meredith Niess, MD MPH
Objectives
Guidelines
The Case
OutIine and critically examine existing research/guidelines on pre-operative chest x-ray
(CXR) use.
Identify downstream consequences of pre-operative CXR overuse.
54-year-old man with mild intermittent asthma presents to his general
surgeon for pre-op evaluation. His umbilical hernia has become more
painful in the past 3 months.
Normal cardiopulmonary exam and labs
Background
Pre-op CXR ordered. Indication
“pre-operative work-up, over 55,
history of asthma”:
CXR reveals a 7mm left parahilar
lung nodule. “CT of the chest for
further evaluation” recommended.
The Royal College of Radiology performed the first major review of pre-operative CXR in 1979
on 10,619 patients and concluded overutilization was rampant. 30+ years of research has
offered little additional guidance. In the spirit of doing the most for the patient by doing the least
to them, the burden of evidence should lie with those electing to perform testing. In this spirit,
the Choosing Wisely Campaign identifies pre-operative CXR as a prioritized area to inform
patients about overtesting.
Screened
Patients
Abnormal
Result
Unsuspected
Abnormality
Useful in
Management
A “useful” CXR changes anesthesia management,
causes delay or cancellation of surgery, or informs postoperative management. Important unanswered
questions address the harm or benefit of these care
changes, and additional downstream effects to the
patient. Literature on these patient-centered outcomes,
morbidity, and mortality is minimal or absent.
Here I review the financial considerations, guidelines,
and evidence on pre-op CXR, which if considered, may
permit avoidance of unnecessary harm.
If 5%, 10%, or 20% of changes positively affect patient outcome, that would be $460,000,
$230,000, or $115,000 respectively without the cost of follow-up studies
Using these estimates, average cost of a CXR to an uninsured patient = $370 today, and
assuming 1 follow-up CT per 100 patients (our case had 2):
$54,500 of imaging led to 1 CXR which changed management.
If 5%, 10%, or 20% of changes positively affect patient outcome, that would be
$1,090,000, $545,000, or $272,500 per positive outcome
One published estimate of unnecessary preop CXR costs $1billion (1987 dollars)
NICE Guidelines, 2003:
ACR Guidelines, 2011:
Patient Condition
Appropriateness
Criteria
Asymptomatic; history and physical unremarkable
2
Acute cardiopulmonary findings by history and physical
9
Chronic cardiopulmonary disease in the elderly (>70), previous CXR
within 6 months available
6
Chronic cardiopulmonary disease in the elderly (>70), previous CXR
within 6 months not available
8
Criteria: 1, 2, 3 Usually not appropriate; 4, 5, 6 May be appropriate; 7, 8, 9 Usually appropriate
Four weeks later, patient arrives in
clinic to review CT results:
“1. No pulmonary nodule.
2. Circumscribed homogenous right
adrenal nodule.”
Adrenal CT recommended:
Evidence
Benign adrenal
adenoma
confirmed.
Financial Considerations
In 1993 dollars and prices:
$23,000 of CXRs led to 1 CXR which changed management.
The American Academy of Anesthesiologists (2001, updated 2003):
“Clinical characteristics to consider include smoking, recent upper respiratory infection, COPD,
and cardiac disease. The Task Force recognizes that chest radiographic abnormalities may be
higher in such patients, but does not believe that extremes of age, smoking, stable COPD,
stable cardiac disease, or resolved recent upper respiratory infection should be
considered unequivocal indications for chest radiography.
The patient has yet to undergo hernia repair.
References
1. Preoperative chest radiology. National study by the Royal College of Radiologists. Lancet 1979;2:83-6.
2. Wiencek RG, Weaver DW, Bouwman DL, Sachs RJ. Usefulness of selective preoperative chest x-ray films. A prospective study. The American surgeon 1987;53:396-8.
3. Charpak Y, Blery C, Chastang C, Szatan M, Fourgeaux B. Prospective assessment of a protocol for selective ordering of preoperative chest x-rays. Canadian journal of
anaesthesia = Journal canadien d'anesthesie 1988;35:259-64.
4. Archer C, Levy AR, McGregor M. Value of routine preoperative chest x-rays: a meta-analysis. Canadian journal of anaesthesia = Journal canadien d'anesthesie 1993;40:1022-7.
5. Munro J, Booth A, Nicholl J. Routine preoperative testing: a systematic review of the evidence. Health technology assessment (Winchester, England) 1997;1:i-iv; 1-62.
6. Silvestri L, Maffessanti M, Gregori D, Berlot G, Gullo A. Usefulness of routine pre-operative chest radiography for anaesthetic management: a prospective multicentre pilot study.
European journal of anaesthesiology 1999;16:749-60.
7. Task Force on Preanesthesia Evaluation ASoA. Practice Advisory for Preanesthesia Evaluation. Park Ridge, IL: American Society of Anesthesiologists; 2001, amended 2003.
8. Excellence NIfHaC. The Use of Routine Preoperative Tests for Elective Surgery. In. London: National Institute for Health and Clinical Excellence; 2003.
9. Smetana GW, Macpherson DS. The case against routine preoperative laboratory testing. The Medical clinics of North America 2003;87:7-40.
10. Compare CAT Scan Cost. 2011. (Accessed 1/20/2013, at http://www.comparecatscancost.com/.)
11. ACR Appropriateness Criteria® routine admission and preoperative chest radiography. Agency for Healthcare Research and Quality (AHRQ), 2011 (last review). (Accessed
1/27/2013, at http://www.guidelines.gov/content.aspx?id=35150.)
12. Chest X-rays before surgery. Consumer Reports, 2012. (Accessed September 8, 2012, at http://consumerhealthchoices.org/catalog/chest-x-rays-acr/.)
13. The Case of the $517 chest x-ray. 2012. (Accessed 1/20/2013, at http://mydoctorsf.com/the-case-of-the-517-chest-x-ray-healthcare-prices.html.)
No Randomized Controlled Trials on effect pre-op CXR has on anesthesia management,
delay/cancellation of surgery, or patient outcomes
Evidence available = poor external and internal validity in 15 reviewed studies.
External: majority 1980s and 1990s – landscape of medicine, testing, and costs changed.
Internal: Non-blinded, non-randomized, mostly retrospective, non-patient-centered
outcomes,
Largest Study since RCR – Silvestri et al. in 1999. n=6111.
Methods: Anesthesiologists from multiple hospitals answered questionnaire after surgery
reporting whether the pre-op CXR changed management.
Results: Dependent on the anesthesiologist, anywhere from 0% to 44% of pre-op CXR’s
“changed management”.
Flaws: outcomes measurement extremely subjective, not patient-oriented.
Major Meta-analysis – Archer et al. in 1993. n=14,390.
10% had abnormalities
1.3% has unsuspected abnormalities
0.1% has CXRs which changed management.